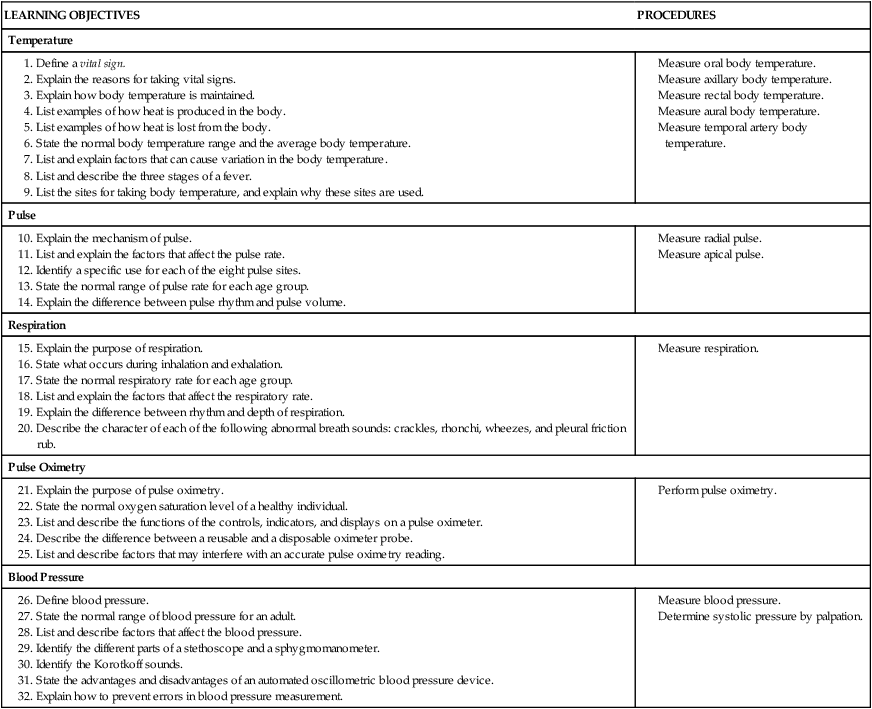
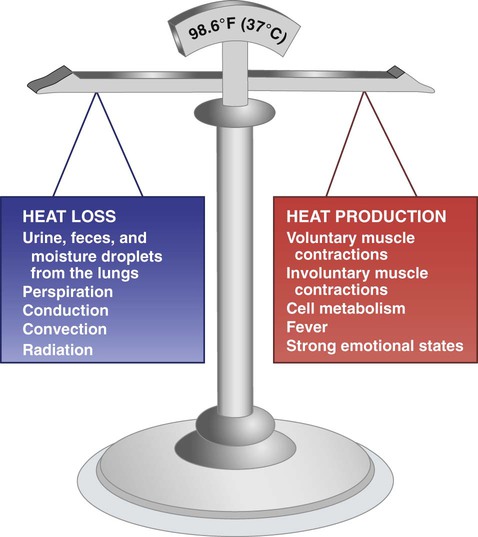
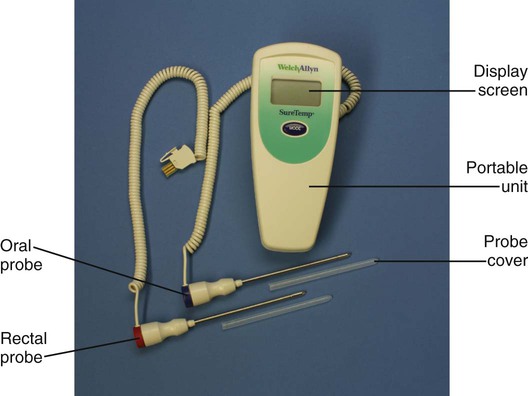
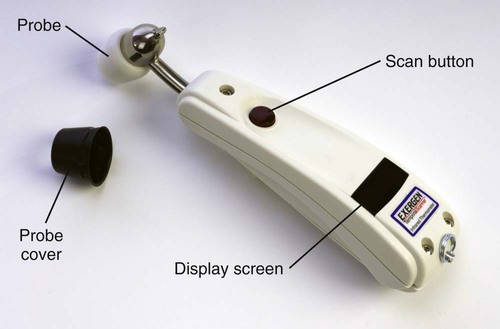
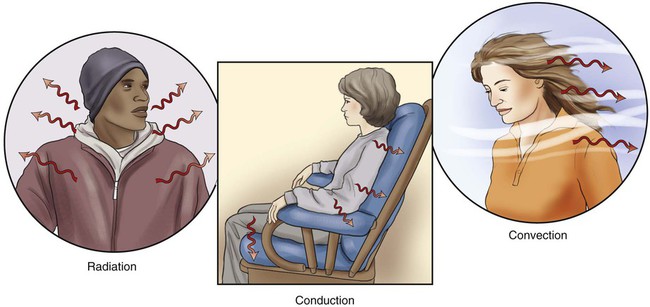
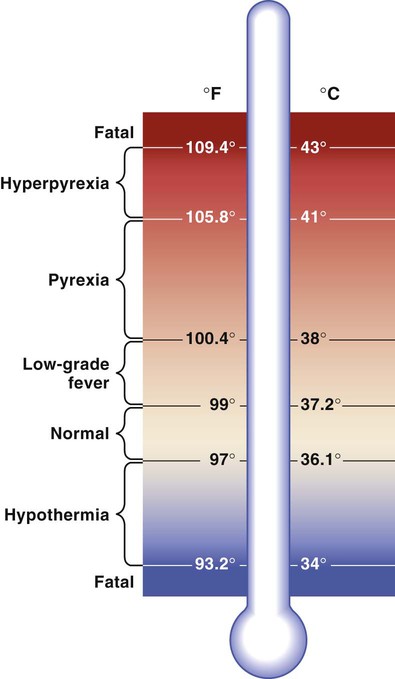
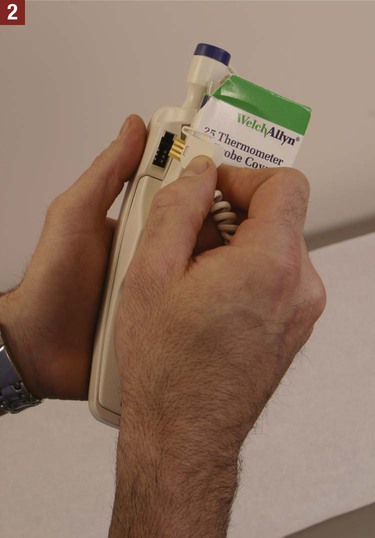
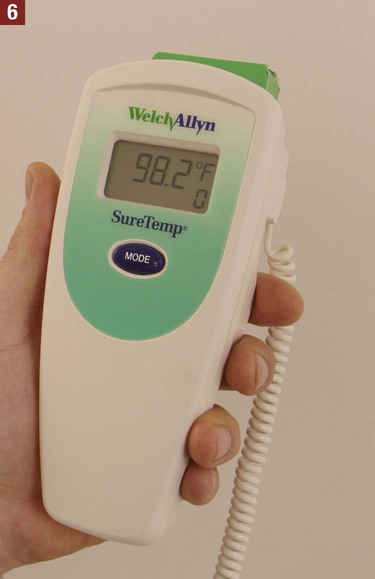
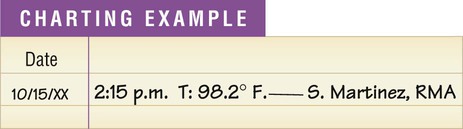
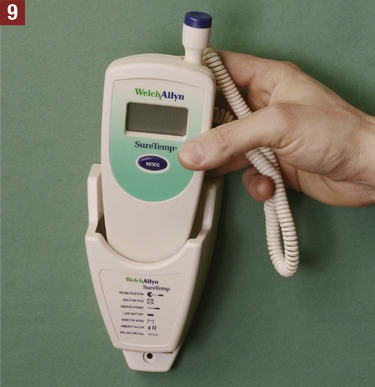
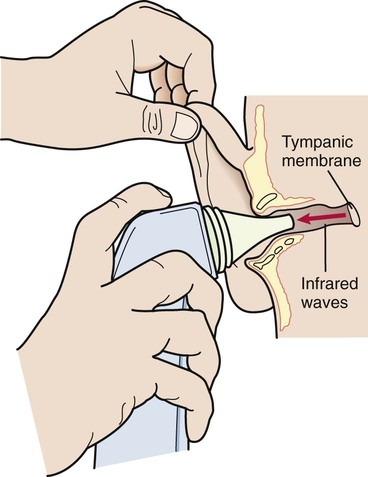
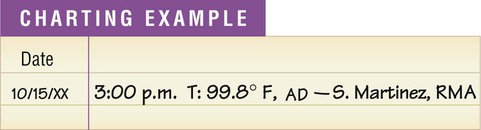
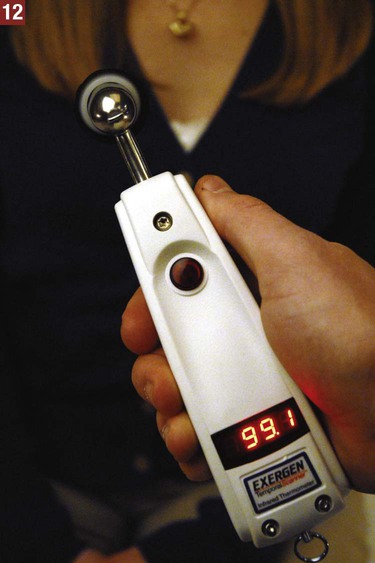
1. Be familiar with the normal ranges for all vital signs. Keep in mind that normal ranges vary based on the different age groups (infant, child, adult, elder). 2. Make sure that all equipment for measuring vital signs is in proper working condition to ensure accurate findings. 3. Eliminate or minimize factors that affect the vital signs, such as exercise, food and beverage consumption, smoking, and emotional state. 4. Use an organized approach when measuring the vital signs. If all of the vital signs are ordered, they are usually measured starting with temperature, followed by pulse, respiration, blood pressure, and pulse oximetry. Body temperature is maintained through a balance of the heat produced in the body and the heat lost from the body (Figure 19-1). A constant temperature range must be maintained for the body to function properly. When minor changes in the temperature of the body occur, the hypothalamus senses this and makes adjustments as necessary to ensure that the body temperature stays within a normal and safe range. If an individual is playing tennis on a hot day, the body’s heat-cooling mechanism is activated to remove excess heat from the body through perspiration. Radiation, conduction, and convection all cause loss of heat from the body. Radiation is the transfer of heat in the form of waves; body heat is continually radiating into cooler surroundings. Conduction is the transfer of heat from one object to another by direct contact; heat can be transferred by conduction from the body to a cooler object it touches. Convection is the transfer of heat through air currents; cool air currents can cause the body to lose heat. These processes are illustrated in Figure 19-2. The purposes of measuring body temperature are to establish the patient’s baseline temperature and to monitor an abnormally high or low body temperature. The normal body temperature range is 97° F to 99° F (36.1° C to 37.2° C), the average temperature being 98.6° F (37° C). Body temperature is usually recorded using the Fahrenheit system of measurement. Table 19-1 lists comparable Fahrenheit and Celsius temperatures and explains how to convert temperatures from one scale to the other. Table 19-1 Equivalent Fahrenheit and Celsius Temperatures From Bonewit-West K: Clinical procedures for medical assistants, ed 8, St Louis, 2011, Saunders. A body temperature less than 97° F (36.1° C) is classified as subnormal, or hypothermia. This means that the heat the body is losing is greater than the heat it is producing. A person usually cannot survive with a temperature less than 93.2° F (34° C). Terms used to describe alterations in body temperature are illustrated in Figure 19-3. 1. Age. Infants and young children normally have a higher body temperature than adults because their thermoregulatory system is not yet fully established. Elderly individuals usually have a lower body temperature owing to factors such as loss of subcutaneous fat, lack of exercise, and loss of thermoregulatory control. Table 19-2 shows the normal ranges of body temperature according to age group. Table 19-2 Variations in Body Temperature by Age From Bonewit-West K: Clinical procedures for medical assistants, ed 8, St Louis, 2011, Saunders. 2. Diurnal variations. During sleep, body metabolism slows down, as do muscle contractions. The body’s temperature is lowest in the morning before metabolism and muscle contractions begin increasing. 3. Emotional states. Strong emotions, such as crying and extreme anger, can increase the body temperature. This is important to consider when working with young children, who frequently cry during examination procedures or when they are ill. 4. Environment. Cold weather tends to decrease the body temperature, whereas hot weather increases it. 5. Exercise. Vigorous physical exercise causes an increase in voluntary muscle contractions, which elevates the body temperature. 6. Patient’s normal body temperature. Some patients normally run a low or high temperature. The medical assistant should review the patient’s past vital sign recordings. 7. Pregnancy. Cell metabolism increases during pregnancy, and this elevates body temperature. A fever can be divided into the following three stages: 1. The onset is when the temperature first begins to increase. This increase may be slow or sudden, the patient often experiences coldness and chills, and the pulse and respiratory rate increase. 2. During the course of a fever, the temperature rises and falls in one of the following three fever patterns: continuous, intermittent, or remittent. Fever patterns are described and illustrated in Table 19-3. During this stage the patient has an increased pulse and respiratory rate and feels warm to the touch. The patient also may experience one or more of the following: flushed appearance, increased thirst, loss of appetite, headache, and malaise. Malaise refers to a vague sense of body discomfort, weakness, and fatigue. Table 19-3 From Bonewit-West K: Clinical procedures for medical assistants, ed 8, St Louis, 2011, Saunders. 3. During the subsiding stage, the temperature returns to normal. It can return to normal gradually or suddenly (known as a crisis). As the body temperature is returning to normal, the patient usually perspires and may become dehydrated. The temperature obtained through the axillary method measures approximately 1° F lower than the same person’s temperature taken through the oral route (see Table 19-2). The medical assistant should make a notation to tell the physician that the temperature was taken through the axillary route. The rectal temperature provides an extremely accurate measurement of body temperature because few factors can alter the results. The rectum is highly vascular and, of the five sites, provides the most closed cavity. The temperature obtained through the rectal route measures approximately 1° F higher than the same person’s temperature taken through the oral route (see Table 19-2). The medical assistant should make a notation on the patient’s chart if the temperature has been taken rectally. An electronic thermometer measures body temperature in a brief time, which varies between 4 and 20 seconds, depending on the brand of thermometer used. The temperature results are digitally displayed on an LCD screen. An electronic thermometer consists of interchangeable oral and rectal probes attached to a battery-operated portable unit (Figure 19-4). The probes are color-coded for ease in identifying them. The oral probe is color-coded with blue on its collar and is used to take oral and axillary temperatures; the rectal probe is color-coded with red on its collar and is used to take rectal temperatures only. Procedures 19-1, 19-2, and 19-3 outline the methods for measuring oral, axillary, and rectal temperatures using an electronic thermometer. The tympanic membrane thermometer is used at the aural site. The tympanic membrane thermometer functions by detecting thermal energy that is naturally radiated from the body. As with the rest of the body, the tympanic membrane gives off heat waves known as infrared waves. The tympanic thermometer functions like a camera by taking a “picture” of these infrared waves, which are considered a documented indicator of body temperature (Figure 19-5). The thermometer calculates the body temperature from the energy generated by the waves and converts it to an oral or rectal equivalent. The tympanic membrane thermometer is battery operated and consists of a small handheld device with a sensor probe (Figure 19-6). To operate the thermometer, the probe is covered with a disposable soft plastic cover and is placed in the outer third of the external ear canal. An activation button is depressed momentarily, and the results are displayed in 1 to 2 seconds on a digital screen. The probe cover is ejected into a regular waste container. The procedure for taking aural body temperature using a tympanic membrane thermometer is presented in Procedure 19-4. Measuring temperature using a temporal artery thermometer is the newest method for assessing body temperature. A temporal artery thermometer is an electronic device consisting of a probe attached to a portable unit (Figure 19-7). Along with measuring the peak temperature, the probe sensor automatically measures the ambient temperature, which is the surrounding air temperature. This is done because there is a small heat loss from the forehead that occurs as a result of cooling by ambient temperature. The thermometer’s computer determines and automatically corrects for any effect from ambient temperature. An accurate body temperature reading is digitally displayed on the screen on the thermometer. The procedure for measuring temperature using a temporal artery thermometer is presented in Procedure 19-5.
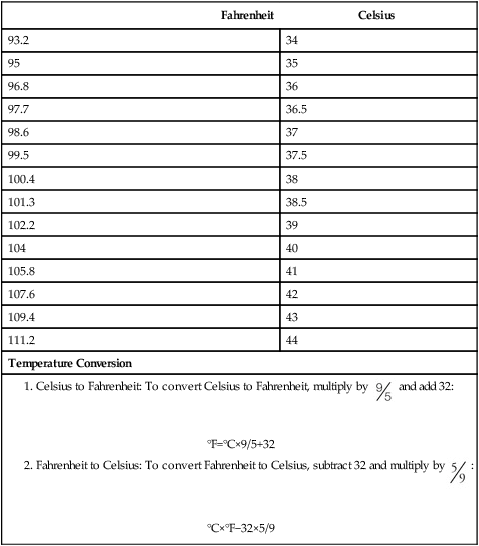
Vital Signs
Introduction to Vital Signs
Temperature
Regulation of Body Temperature
Heat Loss
Body Temperature Range
Fahrenheit
Celsius
93.2
34
95
35
96.8
36
97.7
36.5
98.6
37
99.5
37.5
100.4
38
101.3
38.5
102.2
39
104
40
105.8
41
107.6
42
109.4
43
111.2
44
Temperature Conversion
Alterations in Body Temperature
Variations in Body Temperature
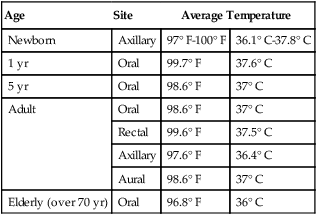
Age
Site
Average Temperature
Newborn
Axillary
97° F-100° F
36.1° C-37.8° C
1 yr
Oral
99.7° F
37.6° C
5 yr
Oral
98.6° F
37° C
Adult
Oral
98.6° F
37° C
Rectal
99.6° F
37.5° C
Axillary
97.6° F
36.4° C
Aural
98.6° F
37° C
Elderly (over 70 yr)
Oral
96.8° F
36° C
Fever
Stages of a Fever
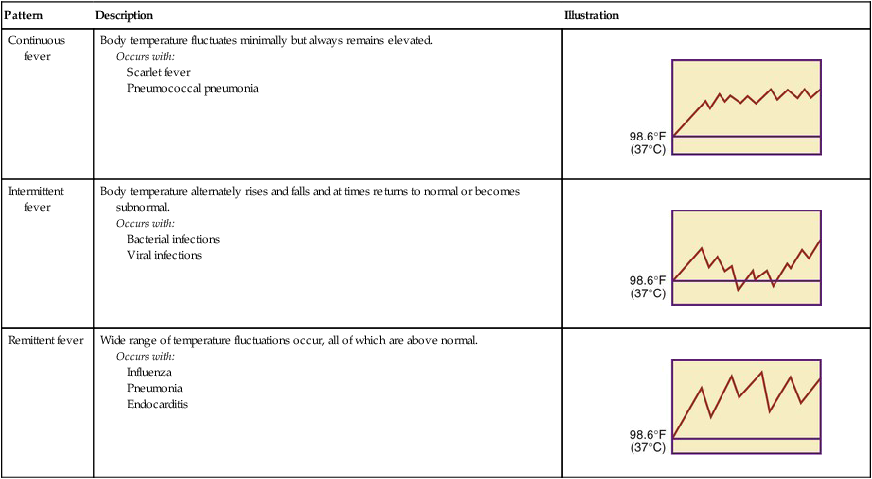
Pattern
Description
Illustration
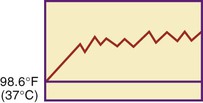
Continuous fever
Body temperature fluctuates minimally but always remains elevated.
Occurs with:
Scarlet fever
Pneumococcal pneumonia
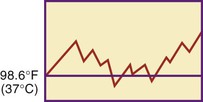
Intermittent fever
Body temperature alternately rises and falls and at times returns to normal or becomes subnormal.
Occurs with:
Bacterial infections
Viral infections
Remittent fever
Wide range of temperature fluctuations occur, all of which are above normal.
Occurs with:
Influenza
Pneumonia
Endocarditis

Assessment of Body Temperature
Assessment Sites
Axillary Temperature
Rectal Temperature
Types of Thermometers
Electronic Thermometer
Tympanic Membrane Thermometer

Temporal Artery Thermometer

Vital Signs
Get Clinical Tree app for offline access
 and add 32:
and add 32: 
 :
: 






 must be charted next to the temperature reading to tell the physician that an axillary reading was taken.
must be charted next to the temperature reading to tell the physician that an axillary reading was taken.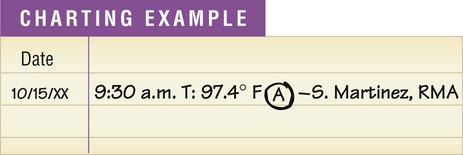

 inch in children, and
inch in children, and  inch in infants. Do not force insertion of the probe. Hold the probe in place until the temperature registers.
inch in infants. Do not force insertion of the probe. Hold the probe in place until the temperature registers.
 inch into the rectum.
inch into the rectum. must be charted next to the temperature reading to tell the physician that a rectal reading was taken.
must be charted next to the temperature reading to tell the physician that a rectal reading was taken.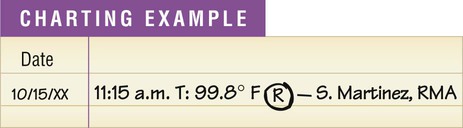











 must be charted next to the temperature reading to tell the physician that a temporal artery reading was taken. Store the thermometer in a clean, dry area.
must be charted next to the temperature reading to tell the physician that a temporal artery reading was taken. Store the thermometer in a clean, dry area.