Vital Signs
Objectives
• Explain the principles and mechanisms of thermoregulation.
• Describe nursing measures that promote heat loss and heat conservation.
• Discuss physiological changes associated with fever.
• Accurately assess body temperature, pulse, respirations, oxygen saturation, and blood pressure.
• Describe cultural and ethnic variations with blood pressure assessment.
• Identify ranges of acceptable vital sign values for an infant, a child, and an adult.
• Explain variations in technique used to assess an infant’s, a child’s, and an adult’s vital signs.
• Describe the benefits and precautions involving self-measurement of blood pressure.
• Identify when to take vital signs.
• Accurately record and report vital sign measurements.
• Appropriately delegate measurement of vital signs to nursing assistive personnel.
Key Terms
Afebrile, p. 445
Antipyretics, p. 452
Auscultatory gap, p. 463
Basal metabolic rate (BMR), p. 443
Blood pressure, p. 458
Bradycardia, p. 455
Cardiac output, p. 452
Celsius, p. 447
Conduction, p. 443
Convection, p. 444
Core temperature, p. 442
Diaphoresis, p. 444
Diastolic pressure, p. 458
Diffusion, p. 456
Dysrhythmia, p. 455
Eupnea, p. 456
Evaporation, p. 444
Fahrenheit, p. 447
Febrile, p. 445
Fever, p. 445
Fever of unknown origin (FUO), p. 445
Frostbite, p. 446
Heat exhaustion, p. 446
Heatstroke, p. 446
Hematocrit, p. 459
Hypertension, p. 460
Hyperthermia, p. 446
Hypotension, p. 461
Hypothermia, p. 446
Hypoxemia, p. 456
Malignant hyperthermia, p. 446
Nonshivering thermogenesis, p. 443
Orthostatic hypotension, p. 461
Oxygen saturation, p. 457
Perfusion, p. 456
Postural hypotension, p. 461
Pulse deficit, p. 455
Pulse pressure, p. 459
Pyrexia, p. 445
Pyrogens, p. 445
Radiation, p. 443
Shivering, p. 443
Sphygmomanometer, p. 461
Systolic pressure, p. 458
Tachycardia, p. 454
Thermoregulation, p. 446
Ventilation, p. 456
Vital signs, p. 441
![]()
The most frequent measurements obtained by health care providers are those of temperature, pulse, blood pressure (BP), respiratory rate, and oxygen saturation. As indicators of health status, these measures indicate the effectiveness of circulatory, respiratory, neural, and endocrine body functions. Because of their importance they are referred to as vital signs. Pain, a subjective symptom, is often called the fifth vital sign and is frequently measured with the others (see Chapter 43). Measurement of vital signs provides data to determine a patient’s usual state of health (baseline data). Many factors such as the temperature of the environment, the patient’s physical exertion, and the effects of illness cause vital signs to change, sometimes outside an acceptable range. Assessment of vital signs provides data to identify nursing diagnoses, implement planned interventions, and evaluate outcomes of care. An alteration in vital signs signals a change in physiological function and the need for medical or nursing intervention.
Vital signs are a quick and efficient way of monitoring a patient’s condition or identifying problems and evaluating his or her response to intervention. When you learn the physiological variables influencing vital signs and recognize the relationship of their changes to other physical assessment findings, you can make precise determinations about a patient’s health problems. Vital signs and other physiological measurements are the basis for clinical decision making and problem solving.
Guidelines for Measuring Vital Signs
Vital signs are a part of the assessment database. You include them in a complete physical assessment (see Chapter 30) or obtain them individually to assess a patient’s condition. Establishing a database of vital signs during a routine physical examination serves as a baseline for future assessments. The patient’s needs and condition determine when, where, how, and by whom vital signs are measured. You need to measure them correctly, and at times you appropriately delegate their measurement. You also need to know expected values (Box 29-1), interpret your patient’s values, communicate findings appropriately, and begin interventions as needed. Use the following guidelines to incorporate measurements of vital signs into nursing practice:
• Based on the patient’s condition, collaborate with health care providers to decide the frequency of vital sign assessment. In the hospital, health care providers order a minimum frequency of vital sign measurements for each patient. Following surgery or treatment intervention you measure vital signs more frequently to detect complications. In a clinic or outpatient setting you take vital signs before the health care provider examines the patient and after any invasive procedures. As a patient’s physical condition worsens, it is often necessary to monitor vital signs as often as every 5 to 10 minutes. The nurse is responsible for judging whether more frequent assessments are necessary (Box 29-2).
• Instruct the patient or family caregiver in vital sign assessment and the significance of findings.
Body Temperature
Physiology
Body temperature is the difference between the amount of heat produced by body processes and the amount of heat lost to the external environment.
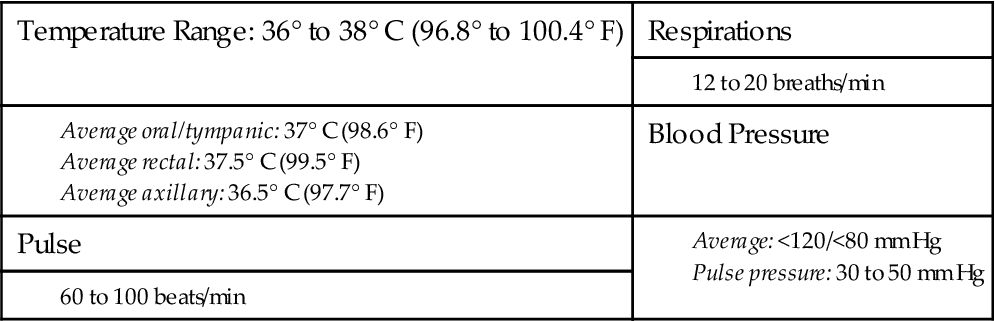
Despite extremes in environmental conditions and physical activity, temperature-control mechanisms of humans keep body core temperature (temperature of the deep tissues) relatively constant (Fig. 29-1). However, surface temperature varies, depending on blood flow to the skin and the amount of heat lost to the external environment. Because of these surface temperature changes, the acceptable temperature of humans ranges from 36° to 38° C (96.8° to 100.4° F). Bodily tissues and cells function best within the relatively narrow temperature range.
The site of temperature measurement (oral, rectal, axillary, tympanic membrane, temporal artery, esophageal, pulmonary artery, or even urinary bladder) is one factor that determines a patient’s temperature. For healthy young adults the average oral temperature is 37° C (98.6° F). In clinical practice you learn the temperature range of individual patients. No single temperature is normal for all people.
The measurement of body temperature aims to obtain a representative average temperature of core body tissues. Sites reflecting core temperatures are more reliable indicators of body temperature than those reflecting surface temperatures. In addition, the temperature value obtained often differs, depending on the measurement site.
Regulation
Physiological and behavioral mechanisms regulate the balance between heat lost and heat produced, or thermoregulation. For the body temperature to stay constant and within an acceptable range, various mechanisms maintain the relationship between heat production and heat loss. Apply knowledge of temperature-control mechanisms to promote temperature regulation.
Neural and Vascular Control
The hypothalamus, located between the cerebral hemispheres, controls body temperature the same way a thermostat works in the home. A comfortable temperature is the “set point” at which a heating system operates. In the home a drop in environmental temperature activates the furnace, whereas a rise in temperature shuts the system down.
The hypothalamus senses minor changes in body temperature. The anterior hypothalamus controls heat loss, and the posterior hypothalamus controls heat production. When nerve cells in the anterior hypothalamus become heated beyond the set point, impulses are sent out to reduce body temperature. Mechanisms of heat loss include sweating, vasodilation (widening) of blood vessels, and inhibition of heat production. The body redistributes blood to surface vessels to promote heat loss.
If the posterior hypothalamus senses that body temperature is lower than the set point, the body initiates heat-conservation mechanisms. Vasoconstriction (narrowing) of blood vessels reduces blood flow to the skin and extremities. Compensatory heat production is stimulated through voluntary muscle contraction and muscle shivering. When vasoconstriction is ineffective in preventing additional heat loss, shivering begins. Disease or trauma to the hypothalamus or the spinal cord, which carries hypothalamic messages, causes serious alterations in temperature control.
Heat Production
Thermoregulation depends on the normal function of heat production processes. Heat produced by the body is a by-product of metabolism, which is the chemical reaction in all body cells. Food is the primary fuel source for metabolism. Activities requiring additional chemical reactions increase the metabolic rate. As metabolism increases, additional heat is produced. When metabolism decreases, less heat is produced. Heat production occurs during rest, voluntary movements, involuntary shivering, and nonshivering thermogenesis.
Heat Loss
Heat loss and heat production occur simultaneously. Skin structure and exposure to the environment result in constant, normal heat loss through radiation, conduction, convection, and evaporation.
Radiation is the transfer of heat from the surface of one object to the surface of another without direct contact between the two. As much as 85% of the surface area of the human body radiates heat to the environment. Peripheral vasodilation increases blood flow from the internal organs to the skin to increase radiant heat loss. Peripheral vasoconstriction minimizes radiant heat loss. Radiation increases as the temperature difference between the objects increases. Radiation heat loss can be considerable during surgery when the patient’s skin is exposed to a cool environment. However, if the environment is warmer than the skin, the body absorbs heat through radiation.
The patient’s position enhances radiation heat loss (e.g., standing exposes a greater radiating surface area, and lying in a fetal position minimizes heat radiation). Help promote heat loss through radiation by removing clothing or blankets. Covering the body with dark, closely woven clothing decreases the amount of heat lost from radiation.
Conduction is the transfer of heat from one object to another with direct contact. Solids, liquids, and gases conduct heat through contact. When the warm skin touches a cooler object, heat is lost. Conduction normally accounts for a small amount of heat loss. Applying an ice pack or bathing a patient with a cool cloth increases conductive heat loss. Applying several layers of clothing reduces conductive loss. The body gains heat by conduction when it makes contact with materials warmer than skin temperature (e.g., application of an aquathermia pad).
Convection is the transfer of heat away by air movement. A fan promotes heat loss through convection. Convective heat loss increases when moistened skin comes into contact with slightly moving air.
Evaporation is the transfer of heat energy when a liquid is changed to a gas. The body continuously loses heat by evaporation. Approximately 600 to 900 mL a day evaporates from the skin and lungs, resulting in water and heat loss. By regulating perspiration or sweating, the body promotes additional evaporative heat loss. When body temperature rises, the anterior hypothalamus signals the sweat glands to release sweat through tiny ducts on the surface of the skin. Sweat evaporates, resulting in heat loss. During physical exercise over 80% of the heat produced is lost by evaporation (Lim, Byrne, and Lee, 2008).
Diaphoresis is visible perspiration primarily occurring on the forehead and upper thorax, although you can see it in other places on the body. For each hour of exercise in hot conditions approximately 1 L of body fluid is lost in sweat (Lim, Byrne, and Lee, 2008). Excessive evaporation causes skin scaling and itching and drying of the nares and pharynx. A lowered body temperature inhibits sweat gland secretion. People who have a congenital absence of sweat glands or a serious skin disease that impairs sweating are unable to tolerate warm temperatures because they cannot cool themselves adequately.
Skin in Temperature Regulation
The skin regulates temperature through insulation of the body, vasoconstriction (which affects the amount of blood flow and heat loss to the skin), and temperature sensation. The skin, subcutaneous tissue, and fat keep heat inside the body. Persons with more body fat have more natural insulation than do slim and muscular people.
The way the skin controls body temperature is similar to the way an automobile radiator controls engine temperature. An automobile engine generates a great deal of heat. Water is pumped through the engine to collect the heat and carry it to the radiator, where a fan transfers the heat from the water to the outside air. In the human body the internal organs produce heat; during exercise or increased sympathetic stimulation the amount of heat produced is greater than the usual core temperature. Blood flows from the internal organs, carrying heat to the body surface. The skin has many blood vessels, especially the areas of the hands, feet, and ears. Blood flow through these vascular areas of the skin varies from minimal flow to as much as 30% of the blood ejected from the heart. Heat transfers from the blood, through vessel walls, to the surface of the skin and is lost to the environment through the heat-loss mechanisms. The core temperature of the body remains within safe limits.
The degree of vasoconstriction determines the amount of blood flow and heat loss to the skin. If the core temperature is too high, the hypothalamus inhibits vasoconstriction. As a result, blood vessels dilate, and more blood reaches the surface of the skin. On a hot, humid day the blood vessels in the hands are dilated and easily visible. In contrast, if the core temperature becomes too low, the hypothalamus initiates vasoconstriction, and blood flow to the skin lessens to conserve heat.
Behavioral Control
Healthy individuals are able to maintain comfortable body temperature when exposed to temperature extremes. The ability of a person to control body temperature depends on (1) the degree of temperature extreme, (2) the person’s ability to sense feeling comfortable or uncomfortable, (3) thought processes or emotions, and (4) the person’s mobility or ability to remove or add clothes. Individuals are unable to control body temperature if any of these abilities is lost. For example, infants are able to sense uncomfortable warm conditions but need assistance in changing their environment. Older adults sometimes need help in detecting cold environments and minimizing heat loss. Illnesses, a decreased level of consciousness, or impaired thought processes result in an inability to recognize the need to change behavior for temperature control. When temperatures become extremely hot or cold, health-promoting behaviors such as removing or adding clothing have a limited effect on controlling temperature.
Factors Affecting Body Temperature
Many factors affect body temperature. Changes in body temperature within an acceptable range occur when physiological or behavioral mechanisms alter the relationship between heat production and heat loss. Be aware of these factors when assessing temperature variations and evaluating deviations from normal.
Age
At birth the newborn leaves a warm, relatively constant environment and enters one in which temperatures fluctuate widely. Temperature-control mechanisms are immature. An infant’s temperature responds drastically to changes in the environment. Take extra care to protect newborns from environmental temperatures. Provide adequate clothing, and avoid exposing infants to temperature extremes. A newborn loses up to 30% of body heat through the head and therefore needs to wear a cap to prevent heat loss. When protected from environmental extremes, the newborn’s body temperature is usually within 35.5° to 37.5° C (95.9° to 99.5° F).
Temperature regulation is unstable until children reach puberty. The usual temperature range gradually drops as individuals approach older adulthood. The older adult has a narrower range of body temperatures than the younger adult. Oral temperatures of 35° C (95° F) are sometimes found in older adults in cold weather. However, the average body temperature of older adults is approximately 36° C (96.8° F). Older adults are particularly sensitive to temperature extremes because of deterioration in control mechanisms, particularly poor vasomotor control (control of vasoconstriction and vasodilation), reduced amounts of subcutaneous tissue, reduced sweat gland activity, and reduced metabolism.
Exercise
Muscle activity requires an increased blood supply and carbohydrate and fat breakdown. Any form of exercise increases metabolism and heat production and thus body temperature. Prolonged strenuous exercise such as long-distance running temporarily raises body temperature.
Hormone Level
Women generally experience greater fluctuations in body temperature than men. Hormonal variations during the menstrual cycle cause body temperature fluctuations. Progesterone levels rise and fall cyclically during the menstrual cycle. When progesterone levels are low, the body temperature is a few tenths of a degree below the baseline level. The lower temperature persists until ovulation occurs. During ovulation greater amounts of progesterone enter the circulatory system and raise the body temperature to previous baseline levels or higher. These temperature variations help to predict a woman’s most fertile time to achieve pregnancy.
Body temperature changes also occur in women during menopause (cessation of menstruation). Women who have stopped menstruating often experience periods of intense body heat and sweating lasting from 30 seconds to 5 minutes. During these periods often intermittent skin temperature increases up to 4° C (7.2° F), referred to as hot flashes. This is caused by the instability of the vasomotor controls for vasodilation and vasoconstriction.
Circadian Rhythm
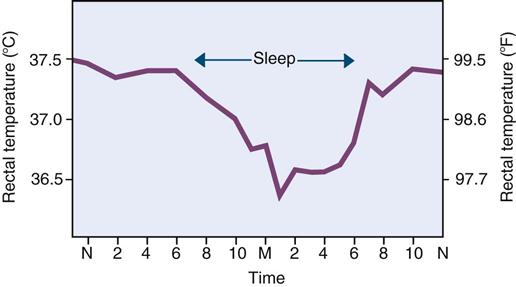
Body temperature normally changes 0.5° to 1° C (0.9° to 1.8° F) during a 24-hour period. However, temperature is one of the most stable rhythms in humans. The temperature is usually lowest between 1:00 and 4:00 AM (Fig. 29-2). During the day body temperature rises steadily until a maximum temperature value at about 4:00 PM and then declines to early-morning levels (Henker and Carlson, 2007). Temperature patterns are not automatically reversed in people who work at night and sleep during the day. It takes 1 to 3 weeks for the cycle to reverse. In general, the circadian temperature rhythm does not change with age.
Stress
Physical and emotional stress increase body temperature through hormonal and neural stimulation. These physiological changes increase metabolism, which increases heat production. A patient who is anxious about entering a hospital or a health care provider’s office often has a higher normal temperature.
Environment
Environment influences body temperature. When placed in a warm room a patient may be unable to regulate body temperature by heat-loss mechanisms, and the body temperature may elevate. If the patient were outside in the cold without warm clothing, body temperature may be low as a result of extensive radiant and conductive heat loss. Environmental temperatures affect infants and older adults more often because their temperature-regulating mechanisms are less efficient.
Temperature Alterations
Changes in body temperature outside the usual range are related to excessive heat production, excessive heat loss, minimal heat production, minimal heat loss, or any combination of these alterations.
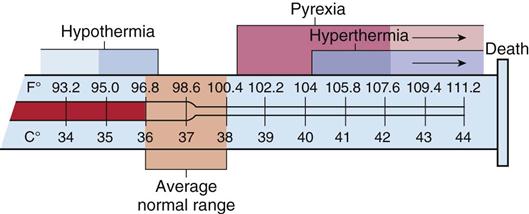
Fever
Fever, or pyrexia, occurs because heat-loss mechanisms are unable to keep pace with excessive heat production, resulting in an abnormal rise in body temperature. A fever is usually not harmful if it stays below 39° C (102.2° F). A single temperature reading does not always indicate a fever. In addition to physical signs and symptoms of infection, fever determination is based on several temperature readings at different times of the day compared with the usual value for that person at that time.
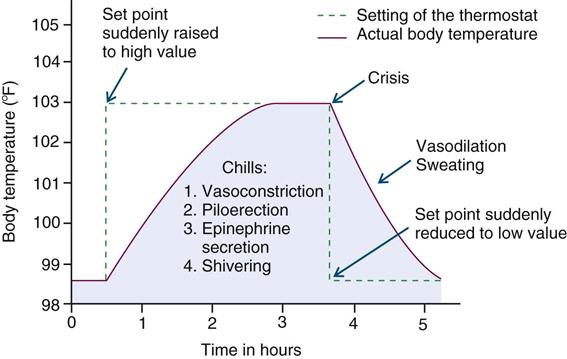
A true fever results from an alteration in the hypothalamic set point. Pyrogens such as bacteria and viruses elevate body temperature. Pyrogens act as antigens, triggering immune system responses. The hypothalamus reacts to raise the set point, and the body responds by producing and conserving heat. Several hours pass before the body temperature reaches the new set point. During this period a person experiences chills, shivers, and feels cold, even though the body temperature is rising (Fig. 29-3). The chill phase resolves when the new set point, a higher temperature, is achieved. During the next phase, the plateau, the chills subside, and the person feels warm and dry. If the new set point is “overshot” or the pyrogens are removed (e.g., destruction of bacteria by antibiotics), the third phase of a febrile episode occurs. The hypothalamus set point drops, initiating heat loss responses. The skin becomes warm and flushed because of vasodilation. Diaphoresis assists in evaporative heat loss. When the fever “breaks,” the patient becomes afebrile.
Fever is an important defense mechanism. Mild temperature elevations as high as 39° C (102.2° F) enhance the immune system of the body. During a febrile episode white blood cell production is stimulated. Increased temperature reduces the concentration of iron in the blood plasma, suppressing the growth of bacteria. Fever also fights viral infections by stimulating interferon, the natural virus-fighting substance of the body.
Fevers and fever patterns serve a diagnostic purpose. Fever patterns differ, depending on the causative pyrogen (Box 29-3). The increase or decrease in pyrogen activity results in fever spikes and declines at different times of the day. The duration and degree of fever depend on the strength of the pyrogen and the ability of the individual to respond. The term fever of unknown origin (FUO) refers to a fever with an undetermined cause.
During a fever cellular metabolism increases, and oxygen consumption rises. Body metabolism increases 10% for every degree Celsius of temperature elevation (Henker and Carlson, 2007). Heart and respiratory rates increase to meet the metabolic needs of the body for nutrients. The increased metabolism uses energy that produces additional heat. If a patient has a cardiac or respiratory problem, the stress of a fever is great. A prolonged fever weakens a patient by exhausting energy stores. Increased metabolism requires additional oxygen. If the body cannot meet the demand for additional oxygen, cellular hypoxia (inadequate oxygen) occurs. Myocardial hypoxia produces angina (chest pain). Cerebral hypoxia produces confusion. Interventions during a fever include oxygen therapy. When water loss through increased respiration and diaphoresis is excessive, the patient is at risk for fluid volume deficit. Dehydration is a serious problem for older adults and children with low body weight. Maintaining optimum fluid volume status is an important nursing action (see Chapter 41).
Hyperthermia
An elevated body temperature related to the inability of the body to promote heat loss or reduce heat production is hyperthermia. Whereas fever is an upward shift in the set point, hyperthermia results from an overload of the thermoregulatory mechanisms of the body. Any disease or trauma to the hypothalamus impairs heat-loss mechanisms. Malignant hyperthermia is a hereditary condition of uncontrolled heat production that occurs when susceptible people receive certain anesthetic drugs.
Heatstroke
Heat depresses hypothalamic function. Prolonged exposure to the sun or a high environmental temperature overwhelms the heat-loss mechanisms of the body. These conditions cause heatstroke, defined as a body temperature of 40° C (104° F) or more (Lewis, 2007). Heatstroke is a dangerous heat emergency with a high mortality rate. Patients at risk include the very young or very old and those who have cardiovascular disease, hypothyroidism, diabetes, or alcoholism. Also at risk are those who take medications that decrease the ability of the body to lose heat (e.g., phenothiazines, anticholinergics, diuretics, amphetamines, and beta-adrenergic receptor antagonists) and those who exercise or work strenuously (e.g., athletes, construction workers, and farmers).
Signs and symptoms of heatstroke include giddiness, confusion, delirium, excess thirst, nausea, muscle cramps, visual disturbances, and even incontinence. Vital signs reveal a body temperature sometimes as high as 45° C (113° F), with an increase in heart rate (HR) and lowering of BP. The most important sign of heatstroke is hot, dry skin. Victims of heatstroke do not sweat because of severe electrolyte loss and hypothalamic malfunction. If the condition progresses, the patient with heatstroke becomes unconscious, with fixed, nonreactive pupils. Permanent neurological damage occurs unless cooling measures are rapidly started.
Heat Exhaustion
Heat exhaustion occurs when profuse diaphoresis results in excess water and electrolyte loss. Caused by environmental heat exposure, the patient exhibits signs and symptoms of fluid volume deficit (see Chapter 41). First aid includes transporting him or her to a cooler environment and restoring fluid and electrolyte balance.
Hypothermia
Heat loss during prolonged exposure to cold overwhelms the ability of the body to produce heat, causing hypothermia. Hypothermia is classified by core temperature measurements (Table 29-1). It is sometimes unintentional such as falling through the ice of a frozen lake. Occasionally hypothermia is intentionally induced during surgical or emergency procedures to reduce metabolic demand and the need of the body for oxygen.
TABLE 29-1
| Celsius | Fahrenheit | |
| Mild | 34°-36° | 93.2°-96.8° |
| Moderate | 30°-34° | 86.0°-93.2° |
| Severe | <30° | <86° |
Accidental hypothermia usually develops gradually and goes unnoticed for several hours. When skin temperature drops below 35° C (95° F), the patient suffers uncontrolled shivering, loss of memory, depression, and poor judgment. As the body temperature falls below 34.4° C (94° F), HR, respiratory rate, and BP fall. The skin becomes cyanotic. Patients experience cardiac dysrhythmias, loss of consciousness, and unresponsiveness to painful stimuli if hypothermia progresses. In cases of severe hypothermia a person demonstrates clinical signs similar to those of death (e.g., lack of response to stimuli and extremely slow respirations and pulse). When you suspect hypothermia, assessment of core temperature is critical. A special low-reading thermometer is required because standard devices do not register below 35° C (95° F).
Frostbite occurs when the body is exposed to subnormal temperatures. Ice crystals form inside the cell, and permanent circulatory and tissue damage occurs. Areas particularly susceptible to frostbite are the earlobes, tip of the nose, and fingers and toes. The injured area becomes white, waxy, and firm to the touch. The patient loses sensation in the affected area. Interventions include gradual warming measures, analgesia, and protection of the injured tissue.
Nursing Process
Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care. Knowledge of the physiology of body temperature regulation is essential to assess and evaluate a patient’s response to temperature alterations and intervene safely. Implement independent measures to increase or minimize heat loss, promote heat conservation, and increase comfort. These measures complement the effects of medically ordered therapies during illness. You also provide education to family members, parents of children, or other caregivers.
Assessment
Through the Patient’s Eyes
During the assessment process thoroughly assess each patient, explore his or her beliefs and experiences, and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care.
Sites
Core and surface body temperature can be measured at several sites. Intensive care units use the core temperatures of the pulmonary artery, esophagus, and urinary bladder. These measurements require the use of continuous invasive devices placed in body cavities or organs and continually display readings on an electronic monitor.
Use a thermometer to obtain intermittent temperature measurements from the mouth, rectum, tympanic membrane, temporal artery, and axilla. You can also apply noninvasive chemically prepared thermometer patches to the skin. Oral, rectal, axillary, and skin temperature sites rely on effective blood circulation at the measurement site. The heat of the blood is conducted to the thermometer probe. Tympanic temperature relies on the radiation of body heat to an infrared sensor. Because the tympanic membrane shares the same arterial blood supply as the hypothalamus, it is a core temperature. Temporal artery measurements detect the temperature of cutaneous blood flow.
To ensure accurate temperature readings, measure each site correctly (see Skill 29-1 on pp. 467-471). The temperature obtained varies, depending on the site used, but it is usually between 36° C (96.8° F) and 38° C (100.4° F). Rectal temperatures are usually 0.5° C (0.9° F) higher than oral temperatures, and axillary temperatures are usually 0.5° C (0.9° F) lower than oral temperatures. Each of the common temperature measurement sites has advantages and disadvantages (Box 29-4). Choose the safest and most accurate site for the patient. When possible, use the same site when repeated measurements are necessary.