Practice Point
End-of-life wound care focuses on:
- pain management
- odor control
- management of exudates
- bleeding control
- self-image
- dignity
- quality of life
Patient and Wound Assessment
It is essential to perform a complete head-to-toe assessment of the end-of-life patient, including physical and psychosocial health and overall quality of life. A thorough assessment will assist the healthcare professional in realistically evaluating the need for preventive interventions as well as efficacy and cost-effectiveness of achieving closure, should there be tissue breakdown. The assessment should establish both the risk for and the presence or absence of skin breakdown, including the presence of a pressure ulcer and the risk for developing additional ulcers. The following areas should be included in the patient assessment:43
- comorbid health problems
- medications the patient is taking
- risk factors present in the patient
- nutritional status
- diagnostic test results
- psychosocial implications
- environmental resources
- patient/family goals.
The Pressure Sore Risk Assessment Scale for Palliative Care68 was developed for use in individuals at or near the end of life. Its seven subscales include sensation, mobility, moisture, activity in bed or chair, nutrition and weight change, skin condition, and friction and shear. Scores can range from 7 to 28, with a score of 12 or lower indicating low risk; 13 to 17, medium risk; 18 to 21, high risk; and 22 or over, very high risk. Risk assessment can be done weekly or with significant changes in condition. (See Box 23-1, Hunters Hill Marie Curie Centre pressure ulcer risk assessment.) Risk reassessments are important given the likelihood of the patient’s deteriorating condition. As the end of life approaches, assessments may be performed less frequently in order to enhance comfort.43
Box 23-1 Hunters Hill Marie Curie Centre Pressure Ulcer Risk Assessment
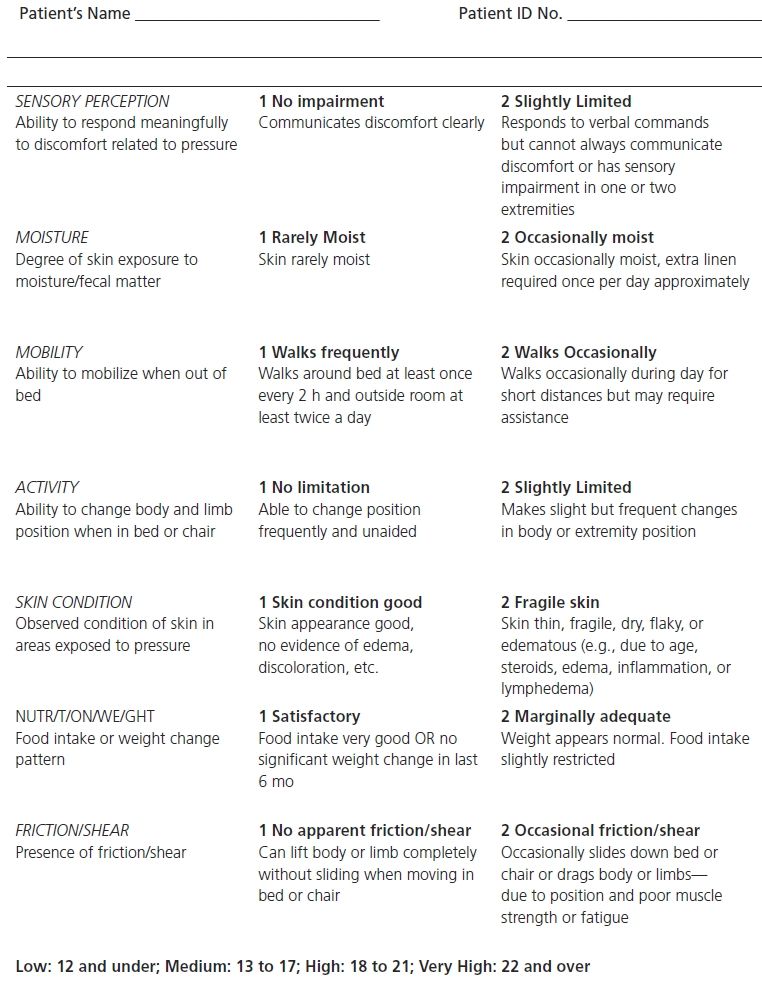
Adapted with permission from Chaplin, J. “Pressure Sore Risk Assessment in Palliative Care,” Journal of Tissue Viability 10(1 ):27–31, 2000. Used with permission. Copyright © 2000 Tissue Viability Society. Published by Elsevier Ltd. All rights reserved.
Wounds or ulcers in end-of-life patients are often chronic in nature, as healing is significantly impaired due to physical condition and existing comorbidities. A chronic pressure ulcer has a well-defined border with surrounding nonblanchable erythema. When induration is present, it can extend outward from the wound edges. Many chronic wounds have rolled-under edges that impede wound healing and closure. Wound edges roll under when the wound bed is dry. In response, the wound attempts to preserve what little moisture is present and epithelialization is slowed, leaving the wound bed unepithelialized. Most wounds have drainage, and chronic wound drainage contains destructive enzymes as well as fibroblasts that are less effective at producing collagen to heal the wound.84 Assess the wound initially and with each dressing change, but at a minimum weekly unless the individual is actively dying.43 (See Chapter 5, Acute and Chronic Wound Healing.)
 Evidence-Based PracticeWound and Patient Assessment in Palliative Care
Evidence-Based PracticeWound and Patient Assessment in Palliative Care
1.0. Set treatment goals consistent with the values and goals of the individual, while considering the family input. (Strength of Evidence = C)
1.1. Set a goal to enhance quality of life, even if the pressure ulcer cannot be healed or treatment does not lead to closure/healing. (Strength of Evidence = C)
1.2. Assess the impact of the pressure ulcer on quality of life of the individual and his or her family. (Strength of Evidence = C)
1.3. Assess the individual initially and with any significant change in condition to reevaluate the plan of care. (Strength of Evidence = C)
Brown, G. “Long-term Outcomes of Full-thickness Pressure Ulcers: Healing and Mortality,” Ostomy/Wound Management 49:42–50, 2003.
 Evidence-Based PracticeMaintaining Skin Integrity in Palliative Care Patients
Evidence-Based PracticeMaintaining Skin Integrity in Palliative Care Patients
1.0.Ensure that a complete skin assessment is part of the risk assessment screening policy in place in all healthcare settings. (Strength of Evidence = C)
Brown, G. “Long-term Outcomes of Full-thickness Pressure Ulcers: Healing and Mortality,” Ostomy/Wound Management 49:42–50, 2003.
Support Surfaces
Support surfaces are “specialized devices for pressure redistribution designed for management of tissue loads, micro-climate, and/or other therapeutic functions (i.e., any mattress, integrated bed system, mattress replacement, overlay, or seat cushion, or seat cushion overlay).”67 Some support surfaces provide the additional capability of turning or rotation assistance. It is important to match the support surface to the needs of the individual such that the surface redistributes weight over a larger area, thereby minimizing tissue pressures, particularly over bony prominences.67 These surfaces are helpful for both the bed and the chair. Refer to the NPUAP/EPUAP/PPPIA guideline43 for more specific recommendations regarding pressure redistribution in palliative care patients.
 Practice Point
Practice Point
Individualize the patient’s turning and positioning schedule based on his or her pain tolerance and comfort level.
 Evidence-Based PracticePressure Redistribution in Palliative Care Patients
Evidence-Based PracticePressure Redistribution in Palliative Care Patients
1.0. Strive to reposition an individual receiving palliative care at least every 4 hours on a pressure-redistributing mattress such as viscoelastic foam or every 2 hours on a regular mattress. (Strength of Evidence = B)
Brown, G. “Long-term Outcomes of Full-thickness Pressure Ulcers: Healing and Mortality,” Ostomy/Wound Management 49:42–50, 2003.
 Evidence-Based PracticeNutrition and Hydration in Palliative Care Patients
Evidence-Based PracticeNutrition and Hydration in Palliative Care Patients
1.0. Allow the individual to ingest fluids and foods of choice. (Strength of Evidence = C)
1.1. Offer several small meals per day. (Strength of Evidence = C)
Brown, G. “Long-term Outcomes of Full-thickness Pressure Ulcers: Healing and Mortality,” Ostomy/Wound Management 49:42–50, 2003.
Pain Management
Both prevention and treatment of skin breakdown can be uncomfortable for individuals at the end of life. The majority of patients with a pressure ulcer experience moderate to severe pain,85–88 especially during dressing changes and wound bed treatments, and the pain can be acute or chronic.88,89 In fact, 21 of 23 patients (91%) in one study reported a pressure ulcer as painful.90 Likewise, in a systematic review of 15 studies addressing the impact of pressure ulcer pain, the authors concluded that “pain was the most significant consequence of having a pressure ulcer and affected every aspect of patients’ lives.”73 In fact, pain from a pressure ulcer can be the most distressing symptom an individual might report.73 It is important to keep in mind that “pain is anything the patient says it is.”91
Wound pain can be caused by the tumor pressing on nerves and blood vessels or by exposure of dermis.92 Pain in wounds often arises from painful procedures, including cleansing and dressing removal, particularly if the dressing is dry and adherent.93 Given that an individual at or near the end of life has a wound that likely will not heal, the wound and wound pain are chronic in nature. Chronic pain is pain that is persistent and can occur even when the wound is not being manipulated.94 Concomitant acute pain can occur with dressing changes, treatments, and additional trauma to the area.
One of the most significant goals in palliative care is to alleviate, or at the very least manage, pain. It is therefore essential to perform regular pain assessments.29,81 Pain assessment tools reported to be valid and reliable include the visual analog scale for pain (VAS pain); the visual rating scale (VRS); the numeric rating scale; the FACES rating scale (FRS); the FLACC scale (face, legs, activity, cry, consolability); and the McGill pain questionnaire (MPQ). A 2005 study95 identified the VAS pain, the FRS, and the MPQ as valid and reliable to identify pressure ulcer pain.
A mild to moderate opioid, such as 1 mg morphine or diamorphine mixed with 1 mg of a hydrogel,96,97 or nonopioid medication can be used to relieve wound pain, as can a topical agent that contains a local anesthetic (e.g., one with lidocaine, such as EMLA cream, Lidoderm, or Regenecare)97–99 or a foam dressing containing ibuprofen (not available everywhere).100,101 One hospital solely dedicated to caring for palliative patients has developed a unique mixture of Balmex and lidocaine 2.75%, which may be applied topically to painful and odorous wounds. They have reported success with this strategy.102 Wound treatment pain can also be minimized by using minimal mechanical force for cleansing (4 to 15 psi irrigation force); using warmed products, such as normal saline or gauze pads103; and avoiding antiseptic and cytotoxic agents.43,72 Nonpharmacological strategies such as music, relaxation, position changes, meditation, guided imagery, healing touch, distraction, etc., are also available.
 Practice Point
Practice Point
Premedicating the patient with pain medication 30 to 60 minutes before changing the dressing is an important part of palliative wound care management.
Wound Dressings
When possible, select a dressing that can remain in place for several days; however, this isn’t always possible when a large amount of exudate is present. A dressing that protects periwound skin is also desirable, as is one that protects the wound from moisture and feces. As a rule, nonadherent, foam, polymeric membrane, and/or silicone dressings are best. Maintain a moist wound care environment to prevent exposure of delicate nerve endings,104 as dry, desiccated wound beds and dressings are nearly always painful.105 (See Wound Treatment Options, Chapter 9.)
 Evidence-Based PracticeTreating Open Pressure Ulcers in Palliative Care Patients
Evidence-Based PracticeTreating Open Pressure Ulcers in Palliative Care Patients
1.0. Diamorphine HDG is an effective treatment for open pressure ulcers [wounds] in the palliative care setting. (Strength of Evidence = B)
Brown, G. “Long-term Outcomes of Full-thickness Pressure Ulcers: Healing and Mortality,” Ostomy/Wound Management 49:42–50, 2003.
Wound Infection, Odor, and Exudate
Tissue deprived of oxygen and nutrients becomes devitalized and nonviable,106 and bacteria thrive on this moist, devitalized tissue.107 As the bacteria colonize, necrotic material appears in the wound and creates an odor, which varies depending on the bacteria present. Nonviable tissue eventually serves as a culture medium to support bacterial growth and inhibit leukocyte phagocytosis of bacteria.106 Odor is generally associated with anaerobic and some gram-negative (e.g., Pseudomonas) microorganisms.83,108 Anaerobic bacteria are usually present in necrotic material, thrive in the absence of oxygen, and can become buried deeper within the wound. Anaerobic bacteria105 also have a stronger, more offensive odor that can be particularly distressing to the patient. The wound appearance becomes black and leathery with exposure to air or yellow-gray when exposed to moisture, which occurs over varying lengths of time depending on the underlying disorder.105
It is the odor, drainage, and pain arising from the infection that are often the most distressing to the individual and therefore should be treated. Wound odor can be embarrassing to the individual and lead to isolation, depression, and poor quality of life.2,22,108 Treatment is aimed at removing the cause of the odor and the odor itself. Because saturated dressings can hold odor, more frequent changing may help control the odor as well as the pain from the weight of the dressing. A secondary dressing may help. Frequent irrigation also helps remove exudate and odor. Nonviable tissue can be debrided, and autolytic debridement is often the least painful for the individual. Sharp debridement is more or less a last resort, and caution must be exercised to prevent excessive bleeding and/or pain.108,109 Topical metronidazole (gel, cream, crushed tablets, oral) has been shown to be effective for anaerobic bacteria as has silver sulfadiazine.4,5,43,110–118 Activated charcoal dressings have also been shown to be helpful.80,84,109,114,118–122
Nonsurgical (autolytic or enzymatic) debridement is recommended due to the tendency for bleeding and “seeding” of malignant cells in fungating and radiation wounds.105 Topical metronidazole has also been used successfully to control odor.2,78 Activated charcoal dressings are effective in controlling odor quickly,22,109,111,115,120,123,124 as are occlusive dressings and frequent dressing changes.22 Cadexomer iodine is an effective antiseptic,116 as is povidone–iodine.117 Silver dressings are effective for treating infections and thus in controlling odor. Dakin’s solution (0.25% sodium hypochlorite) is another effective odor controller; it is saturated into gauze and placed in the wound for a limited time and may cause some discomfort.117 Placement of larvae is another effective method of eliminating infection and controlling odor from wounds with extensive necrotic tissue.118 Room deodorizers are also helpful. Sugar paste and honey are once again being used for their antibacterial and debriding properties.121,122 The high sugar content produces a hyperosmotic wound environment to inhibit bacterial growth and assist in debridement.9,121,122
Periwound skin protection is crucial because exudate, which is liquid and sometimes caustic, can exacerbate skin damage123 by causing maceration, breakdown, and itching.43 Dressings that appropriately control exudate without unnecessarily increasing wetness or dryness are recommended, such as an alginate, Hydrofiber, foam, or a nonadherent dressing (silicone, polymeric foam, foam), often with a secondary absorbent pad.105,124,125 Be sure to change dressings when they become saturated, as heavy or overly saturated dressings can cause wound bed pain and irritate periwound skin. Alternatively, if exudate is minimal, a low-absorbency dressing, such as a hydrocolloid or semipermeable film, is recommended.126 A barrier film around the periwound area is helpful in controlling damage from moisture. See Chapter 9, Wound Treatment Options, for further information on dressings.
 Evidence-Based PracticeWound Dressing and Odor Control Options for Palliative Care Patients
Evidence-Based PracticeWound Dressing and Odor Control Options for Palliative Care Patients
1.0. Manage the pressure ulcer [wound] and periwound area on a regular basis as consistent with the individual’s wishes. (Strength of Evidence = C)
1.1. Use antimicrobial agents as appropriate to control known infection and suspected critical colonization.2,102,108,112,127 (Strength of Evidence = C)
1.2. Consider the use of properly diluted antiseptic solutions for limited periods of time to control odor. (Strength of Evidence = C)
1.3. Consider the use of topical metronidazole to effectively control pressure ulcer [wound] odor associated with anaerobic bacteria and protozoal infections.2,102,108,128–131 (Strength of Evidence = C)
1.4. Consider the use of dressings impregnated with antimicrobial agents (e.g., silver, cadexomer iodine, medical grade honey) to help control bacterial burden and odor.122 (Strength of Evidence = C)
1.5. Consider the use of charcoal or activated charcoal dressings to help control odor.22,108,132,133 (Strength of Evidence = C)
1.6. Consider the use of external odor absorbers for the room (e.g., activated charcoal, kitty litter, vinegar, vanilla, coffee beans, burning candle, potpourri).2,128,132 (Strength of Evidence = C)
1.7. Cleanse the wound with each dressing change using potable water (i.e., water suitable for drinking),134 normal saline, or a noncytotoxic cleanser to minimize trauma to the wound and help control the odor.72,135 (Strength of Evidence = C)
1.8. Debride the ulcer [wound] of devitalized tissue to control infection and odor.43,72 (Strength of Evidence = C)
1.9. Avoid sharp debridement with fragile tissue that bleeds easily.72,136–138 (Strength of Evidence = C)
Brown, G. “Long-term Outcomes of Full-thickness Pressure Ulcers: Healing and Mortality,” Ostomy/Wound Management 49:42–50, 2003.
 Practice Point
Practice Point
Odor control is vital for enhancing quality of life for wound patients receiving palliative care.
The inflammatory fluid that seeps from the extracellular spaces is what is known as exudate. All bacteria produce exudate, the color and odor of which vary according to the causative organism.105 For example, green exudate generally indicates gram-negative, aerobic bacteria, which respond well to silver found in many dressings now on the market.105 The more persistent the inflammation or infection is, the more exudate that will be produced. Exudate frequently contains proteins; when combined with inadequate oral intake of protein commonly seen in the end-of-life individual, the degree of hypoproteinemia can increase. Managing exudates can be a major challenge.127
Fungating Wounds
Fungating wounds occur when the skin and its supporting blood and lymph vessels are infiltrated by a local tumor or by metastatic spread from a primary tumor, resulting in oxygen starvation to the tissue and eventual necrosis.12,120,136 It’s reported that approximately 5% to 19% of patients with metastatic cancer will develop a fungating wound.11,137 The incidence in elderly individuals over age 70 is higher.125,134 Although these wounds often develop during the last months of life, they can be present for years.22 The most common site for development of a fungating wound is the breast, but they can also be found on the head and neck as well as in an area of melanoma. The anatomical location and the delicacy of the surrounding tissue make it challenging to address these wounds.
The term fungating refers to a malignant process of both ulcerating and proliferative growth through direct invasion.139–142 An ulcerating wound will produce a craterlike wound, whereas a lesion with a predominantly proliferative growth pattern often develops into a nodular “fungus”- or “cauliflower”- appearing lesion.137,139 Mixed-appearing lesions can also develop.137,139 Skin tumors tend to become ulcerated because the skin is a bacterially contaminated surface.140 Common symptoms of fungating wounds include exudate, pain, odor, pruritus, and bleeding as well as psychosocial issues.120,136
 Practice Point
Practice Point
Families, support persons, and caregivers may need emotional support when viewing patients with fungating wounds.
Fungating wounds rarely heal;139 thus, management is centered on symptom control, promotion of comfort, and maintenance or improvement of quality of life.137,141 Assessment and management by healthcare providers, especially the nurse and physician, are most challenging.137 Therefore, excellent interdisciplinary care and ongoing patient–caregiver communication are essential.
Care of Fungating Wounds
Woo and Sibbald80 proposed an acronym for treatment of fungating wounds. HOPES provides a systematized approach and includes Hemorrhage, Odor, Pain, Exudate, and Superficial infection.80 Hemorrhage due to erosion of blood vessels is the most common emergency seen in fungating wounds and can also be related to the decreased platelet function within the tumor.142 Blood vessels can become eroded from the tumor cells themselves or secondary to necrosis or sloughing of tissues after radiotherapy.143 Nonsurgical (autolytic or enzymatic) debridement is recommended due to the tendency for bleeding and “seeding” of malignant cells.105,124 Fungating lesions are friable and predisposed to bleeding. To minimize bleeding, use a nonadherent or soft silicone dressing, maintain a moist wound bed, and clean by gentle irrigation rather than swabbing.140 Dry dressings can cause bleeding when they adhere to the wound bed and should be avoided.105 Alginate dressings have a high seaweed content and exchange sodium ions for calcium ions in the wound bed, thus encouraging the clotting cascade. Alginates must be used with caution in fragile tumors, however, because these dressings can also cause bleeding.96 Other natural hemostats are collagen and oxidized cellulose; silver nitrate is a sclerosing agent; epinephrine is a vasoconstrictor; and sucralfate is an astringent.105,120,134 Hemostatic surgical sponges can also be used and left in place for a time.22 Alginates, foam, silicone, and polymeric foam dressings are helpful for odor.144,145
Radiation Wounds
Radiation therapy targets a high-energy x-ray beam to an area of treatment. The target area is usually a tumor, the area surrounding a tumor, or an area where a tumor has been surgically removed. While each treatment is designed to target tissue at a particular depth, the tissues overlying the site can be affected as well.146,147
Radiation-related skin changes or ulcerations can occur in soft tissues during the course of therapy, immediately after therapy, or a long time following therapy.146,147 Skin problems can also be noted in individuals who underwent treatments years ago before technological improvements in radiation machines were implemented. The skin reactions seen are generally specific to the area that was irradiated, and the inflammation can occur almost immediately.147,148 Acute erythematous wounds result from the dilated blood vessels in the irradiated area. The ulceration may be large and may present initially as a draining sinus.149
The more common skin reactions associated with radiation therapy include flaking or peeling, redness, changes in pigmentation, loss of hair, decreased or absent perspiration, superficial blood vessel changes, edema, ulceration, and scarring.140,147 (See Box 23-2, Common radiation wound skin reactions.)
Box 23-2 Common Radiation Wound Skin Reactions
- Flaking or peeling (dry desquamation)
- Erythema
- Alteration in pigmentation
- Hair loss
- Loss of perspiration or sebaceous excretion
- Changes in superficial blood vessels
- Edema
- Ulceration (moist desquamation)
- Scarring
From Smith, S. Skin Care Following Radiation Therapy: The Clinician’s Notebook. Carrington Laboratories, Inc. Newsletter; 1(3):1–3. Available at: http://www.woundcare.org/newsvol2n2./ar3.htm. Accessed June 4, 2014.
Changes at the cellular level can be reflected by poor healing at the site. Healing is impeded related to atrophy of the epidermis and epidermal accessory structures, microvascular occlusions, exuberant connective tissue, decreased fibroblast reproduction, and significant amounts of cellular damage.140,149
Most radiation-related lesions are superficial. In 1994, the Oncology Nursing Society created a classification system for radiation ulcers. This system was refined in 2002. The five-level classification system ranges from “0” or no skin problem within a radiation field to “4” or skin necrosis or ulceration of full-thickness dermis150 (Table 23-1).
Table 23-1 Oncology Nursing Society Classification for Skin Reactions
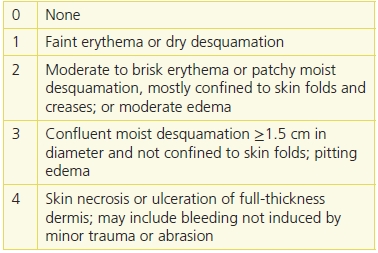
Adapted from Oncology Nursing Society. Radiation Therapy Patient Care Record: A Tool for Documenting Nursing Care. Pittsburgh, PA: Author, 2002, with permission of the publisher.
Treatment of a radiation-induced skin lesion is essentially like treatment for other types of wounds. Any tissue within a radiation field must be considered at high risk for potential breakdown and should be kept clean, appropriately moistened, and protected from potential injury. Skin can also be protected by avoiding restrictive clothing, adhesives, harsh chemicals, heat or sunlight, and trauma. Should a minor skin reaction such as erythema or dry desquamation occur, the same guidelines apply, along with use of a topical hydrogel or a steroid cream.140 Moist desquamation is also treated in the same manner as described above, with the addition of a nonadherent or foam dressing to manage the wound environment. It’s important to cover the wound to prevent evaporation of fluid, control pain, and reduce risk of infection.147,148
Severe ulceration or necrosis needs to be treated as an open wound, using moist wound healing principles.140,147 However, it’s important to first rule out a new malignancy in the area.148 Skin grafting or growth factor application may be required.136 As a consequence of the vascular changes and resultant hypoxia, irradiated tissues have a decreased ability to fight infection. Avoiding or controlling infection is important, and antibiotics are best delivered topically.149 The vascular changes and hypoxia also are responsible for pain being present in these ulcerations.149 These wounds are typically difficult to manage and slow to heal. In all instances, systemic support is necessary to enhance the patient’s healing potential in order to minimize further trauma to the wound site.147
Summary
While cure and/or healing of a wound is not always realistic, it’s possible to provide compassionate and symptom-relieving treatment for palliative care patients who have wounds. This includes balancing the management of local wound symptoms, such as pain, odor, exudate, and bleeding, while preserving patient dignity and self-esteem and maximizing quality of life. Few randomized clinical trials or other research studies exist in the area of palliative wound care. However, there is a consensus document from the International Palliative Wound Care Initiative that looks at managing these wounds across the life continuum.151 Continued study is needed to more clearly understand when a palliative care goal is appropriate. A comprehensive palliative wound care program needs to be developed in clinical agencies that work with these patients. The interdisciplinary team would include the physician, nurses, wound care specialists, dietitian, chaplain services, social services, and pain and hospice consultants.69 Palliative care units are increasing in number, particularly for patients who are chronically, but not terminally, ill.152 Wounds treated appropriately, even when the goal is not healing, can markedly improve in 50% of the cases, even on a hospice unit.7,153,154
 PATIENT SCENARIO
PATIENT SCENARIO
Clinical Data
Mr. M is an 86-year-old widower who has end-stage cancer with bone metastasis. Because he is quite coherent, refuses to be hospitalized, and insists on staying in his home, his family is caring for him with the assistance of hospice. While Mr. M is consuming liquids fairly well, his food intake is very minimal; he eats very little, even with encouragement. With his small frame, his current weight is 109 lbs, down from his usual weight of about 165 lbs. He remains continent and uses a bedside commode with assistance. Upon assessment, the hospice nurse identifies a stage III pressure ulcer over the left greater trochanter measuring 2.5 × 2.3 × 0.3 cm, and there is a moderate amount of tan/green exudate with a slightly foul odor emanating from it. He also has a stage IV pressure ulcer measuring 0.25 × 0.25 cm on the left ear.
The family has tried both a sheepskin and an air overlay on his bed, but Mr. M insisted they be removed because he didn’t like them. Mr. M informs the hospice nurse that he is “ready to go, and doesn’t wish for any fancy or heroic treatments. Just let me be.”
Case Discussion
Based on the initial assessment, the hospice nurse identified a number of problems that needed to be addressed. The assessment included ascertaining both Mr. M’s goals of care and those of his family. Mr. M expressed his desire to just be kept comfortable. His wish was to remain in his own bed with a “pillow top” mattress rather than in a “hospital” bed, and he was adamant that he did not wish to have any other pressure-redistributing devices on his bed. While a plan of care would include regular repositioning, Mr. M verbalized that “it hurt less to lie on my left side on the ulcer than in any other position.” The nurse educated him on the risk for further breakdown of the ulcer and ear as well as other areas of his skin. With encouragement from his family, Mr. M agreed to lie on his back and right side for 30 minutes each and on his left side for 2 hours at a time, on a rotating basis. Bilateral heel protectors were used, and his legs were elevated with pillows placed lengthwise in the bed.
Mr. M’s ulcer was cleansed at each dressing change with an antiseptic solution to assist with odor management and covered with a composite dressing. A foam dressing was used on the ear to cushion and protect it. A pie tin with charcoal was placed under his bed to absorb room odor. A skin protectant was used, particularly over bony prominences, to help prevent further breakdown and protect his fragile skin.
Mr. M’s dietary likes and dislikes were also assessed. After being educated on the need for protein for strength and energy to get up to the bedside commode, he agreed to consume three high-protein liquid drinks per day, along with popsicles, ice cream, and occasionally oatmeal and a piece of cold meat rolled with a slice of cheese, as tolerated.
After pain assessment as well as 30 minutes prior to dressing changes, Mr. M was medicated using a nonopioid medication. Mr. M was encouraged to request a “time-out” during dressing changes if needed.
While the pressure ulcer over the left greater trochanter did not heal, it only increased in size to 3.5 × 3.5 × 0.3 cm prior to his death. This outcome was within the goal of the patient and family. The ulcer on the left ear did not heal either, nor did it increase in size. Taking care to position Mr. M’s head when he was on his left side proved helpful in preventing deterioration. Mr. M remained coherent up until his death. Two days prior to his death, Mr. M expressed his appreciation for allowing him to do things “his way.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


