Becky Dorner, RDN, LD, FAND
We gratefully acknowledge the contributions of David R. Thomas, MD for his work on previous editions of this chapter.
Objectives
After completing this chapter, you’ll be able to:
- describe the process of nutritional screening using a validated form to identify risk for malnutrition and pressure ulcers
- identify the parameters involved in completing a nutritional assessment
- define the importance of nutrients for wound healing
- implement validated nutrition guidelines for the prevention and healing of pressure ulcers.
Nutrition plays a key role in both the prevention and treatment of wounds. The goal in preventing pressure ulcers is to screen, identify, and provide appropriate interventions for individuals at risk for malnutrition and pressure ulcer development. A nutritional assessment should be completed both for individuals who are at high risk for developing pressure ulcers and for those who currently have wounds. The data derived from the assessment should be used to develop the nutritional section of the wound treatment and/or care plan. The nutritional interventions selected to manage the current condition should be individualized, based on standard guidelines, and reviewed as new research data become available.
Impact of Undernutrition/Malnutrition
The National Pressure Ulcer Long-Term Care cohort study of 1,524 residents in 95 nursing homes noted a higher-pressure ulcer incidence among frail residents and those who had more severe illness, low BMI, significant weight loss, and difficulty eating independently.1 A study demonstrated that weight loss and/or preexisting malnutrition was a positive predictive variable in all eight major surgery–associated “never events” defined by the Centers for Medicare and Medicaid Services (CMS) including pressure ulcers where the odds increased 3.8 times.2 Studies diagnosing malnutrition have used various criteria, such as anthropometric benchmarks, biochemical tests, or physical assessment parameters, to define malnutrition often failing to differentiate between undernutrition and severe malnutrition.3–5 Malnutrition was defined by the Agency for Healthcare Research and Quality (AHRQ) as one of the common syndromes associated with increased risk for mortality and institutionalization that may be impacted by primary and secondary preventions.6 Malnutrition is defined as any nutritional imbalance7; therefore, even overweight or obese individuals who experience a severe acute illness or major traumatic event are at risk for malnutrition. The consensus statement of the Academy of Nutrition and Dietetics (Academy) and the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) recommends a set of diagnostic characteristics be used to identify and document adult malnutrition.5
Chronic starvation occurs solely as a result of inadequate nutrient intake as metabolism adapts by lowering energy expenditure, thus protecting lean body mass (LBM). Inflammation is the body’s method of protecting itself when metabolic stress arises from the impact of injury, illness, or infection. Inflammation is necessary to remove damaged cells or pathogens and begin the healing process. The pathophysiology of malnutrition and the inflammatory process are associated with declining nutritional status and health. Diseases such as diabetes mellitus (DM), cardiovascular diseases, arthritis, and cancers cause chronic inflammation that is sustained, low grade, and persistent. Elevated energy expenditure and catabolism of LBM is associated with chronic inflammation. Individuals with severe acute illness or trauma experience severe inflammation and increased metabolic stress, which lead to increased energy expenditure and nitrogen excretion. This process triggered by the acute-phase inflammatory response leads to malnutrition and can limit the effectiveness of nutritional interventions.8 The anorexia accompanying inflammation promotes continued loss of lean tissue, especially if nutrient intake is inadequate. Jensen describes the severity and length of inflammation leading to the loss of LBM and physical function as disease-related malnutrition.8 Individuals with chronic or acute disease/injury and inflammation have elevated inflammatory markers (tumor necrosis factor, interleukin-6, and alpha interleukin-18), reduced cell mass, and loss of lean body protein.9 LBM is vital for wound healing, muscle strength, plus immune and organ function. An international guideline committee composed of members from A.S.P.E.N and the European Society for Enteral and Parenteral Nutrition (ESPEN) recommended an etiology-based approach for diagnosing adult malnutrition, which was adapted by the Academy and A.S.P.E.N.8 Figure 10-1 etiology-based malnutrition syndromes, is based on Jensen’s proposal that malnutrition is driven by various etiologies and degrees of inflammation.
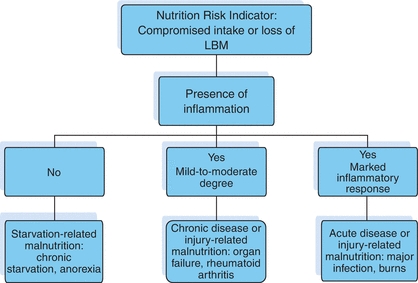
Figure 10-1. Etiology-Based Malnutrition. Adapted with permission from White, J., Guenter, P., Jensen, G., et al. “Consensus Statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics Recommended for the Identification and Documentation of Adult Malnutrition (Undernutrition),” Journal of the Academy of Nutrition and Dietetics 112:730, 2012. Copyright © 2012 American Society for Parenteral and Enteral Nutrition and the Academy of Nutrition and Dietetics. Published by Elsevier Inc. All rights reserved.
The Academy and A.S.P.E.N consensus statement recommends identifying two or more of the following six characteristics when diagnosing malnutrition5:
- Insufficient energy intake based on individual’s estimated needs
- Weight loss
- Loss of muscle mass
- Loss of subcutaneous fat
- Localized or generalized fluid accumulation that may sometimes mask weight loss
- Diminished functional status as measured by handgrip strength
Implementing this standardized method to diagnose the nutritional status of adults should become part of the interdisciplinary team’s (IDT) protocol for prevention and/or treatment of individuals with wounds. Nutritional screening supports the concept of a standardized method to diagnose malnutrition.
Nutritional Screening
Nutritional screening is the process of identifying characteristics that are known to be associated with nutrition problems. Its purpose is to pinpoint individuals who are malnourished or at nutritional risk and then to determine appropriate interventions based on the findings. Screening tools should be cost-effective, validated for the population served, easy for the practitioner to use, and acceptable to the individual. Any qualified member of the healthcare team, including the registered dietitian, nutritionist (RDN) dietetic technician, registered (DTR), nurse, physician, or other qualified health professional, can complete a nutritional screening tool. The result should be documented in the medical record and communicated to the RDN and IDT.
A number of validated nutritional screening tools are available, including the Mini Nutritional Assessment (MNA), the Malnutrition Universal Screening Tool (MUST), the Malnutrition Screening Tool (MST), and the Subjective Global Assessment (SGA).1 The MNA screens six areas, recent food intake, weight loss mobility, psychological stress, neuropsychological problems, and body mass index (BMI), and assigns each a numerical score. The total score defines the risk of malnutrition. It has been validated in the elderly population in community and long-term care settings.10,11 Research comparing the nutritional status of individuals with and without pressure ulcers concluded that the MNA is easy to use for assessing older adults with pressure ulcers and multiple comorbidities.12 Tsai et al. in a comparative study of six screening tools used to sample elderly people established the MNA had a sensitivity of 98.1% and specificity of 75% for identifying nutritional risk.13
The Malnutrition Universal Screening Tool (MUST) has been validated in acute care, long-term care, and community settings. Poulia et al. concluded that the MUST was the most appropriate tool for evaluating the risk of malnutrition in older adults admitted to hospitals, with a high sensitivity (87.3%) and a high negative predictive value (75%) for identifying nutritional risk.14
The Nutrition Risk Screening (NRS) 2002 is also a validated screening tool for adults in hospitals.15 The Short Nutritional Assessment Questionnaire (SNAQ) has been validated in both the hospital and residential care. Weight change, appetite, supplements, and tube feeding are the parameters of the SNAQ.16
When the screening tool triggers risk for or actual malnutrition, undernutrition, or unintended weight loss, a timely referral to the RDN is critical for nutritional assessment and intervention. Conditions that require immediate nutritional assessment and intervention include:
- Unintended weight loss: 5% in 30 days, or 10% in 180 days
- Disease states and conditions: diabetes, malabsorption, dementia, chronic obstructive pulmonary disease (COPD), cancer, or renal disease
- Immobility and inactivity: hip fracture, spinal cord injury, and stroke
- Chewing and swallowing difficulties (dysphagia) resulting from stroke, Parkinson’s disease, cerebral palsy, or other conditions
- Appetite decline, anorexia, and poor food and fluid intake
- Adverse effects of medications
Altered mental status often limits an individual’s ability to eat independently or to comprehend the importance of consuming a balanced diet. Advanced dementia can result in weight loss, dysphagia, and malnutrition. When individuals become incapable of responding to caregivers’ assistance to nourish them, this can lead to unintended weight loss, which may in turn increase their risk for pressure ulcer development.
Immobility affects an individual’s ability to purchase food, prepare meals, or travel to a restaurant or congregate setting for meals and sometimes affects ability to enjoy food or metabolize food properly. This may result in the consumption of a diet lacking in the proper nutrients. For example, hip fracture and spinal cord injury restrict mobility, and hip fracture often results in increased pain that makes it difficult for the individual to concentrate on consuming healthy meals. Functional limitations, such as difficulty chewing or swallowing, affect the individual’s ability to ingest adequate calories and fluids. Sensory problems, such as declining hearing and vision, compromise a person’s communication skills, often resulting in reduced caloric intake.
Nutritional Assessment
Nutritional assessment is a systematic process of obtaining, verifying, and interpreting data in order to make decisions about the nature and cause of nutrition-related problems. It is an ongoing process that involves initial data collection followed by continued reassessment and analysis of the individual’s status compared with specific criteria.11 The Academy of Nutrition and Dietetics Nutrition Care Process (NCP), which is designed to improve the quality and consistency of individualized nutrition care for individuals, should be followed by RDNs and DTRs in all healthcare settings.17 The NCP consists of four steps: nutritional assessment, nutritional diagnosis, nutritional intervention, and nutritional evaluation and monitoring. RDNs and DTRs are the only healthcare professionals who utilize the NCP. Table 10-1 describes the Nutrition Care Process.
Table 10-1 Nutritional Care Process
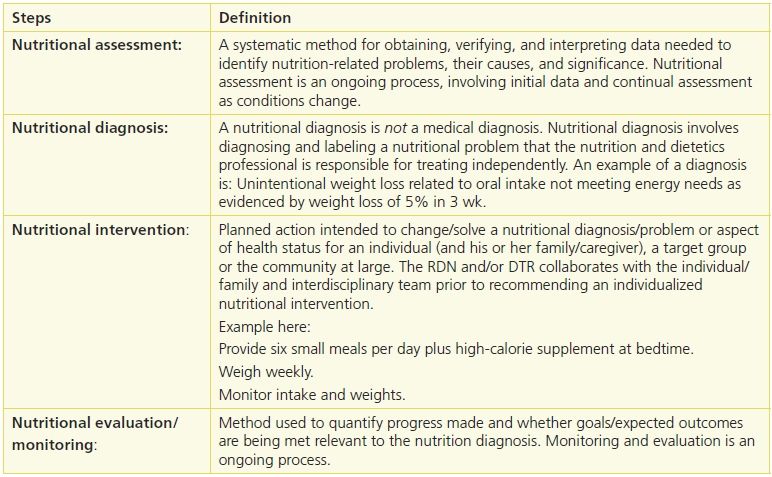
Reprinted from Academy of Nutrition and Dietetics. International Dietetics and Nutrition Terminology Reference Manual: Standardized Language for the Nutrition Care Process, 4th ed. Chicago, IL: Academy of Nutrition and Dietetics, 2013. Copyright © 2013.
The NCP identifies five domains for nutritional assessment: Food–Nutrition Related History, Biochemical Data, Anthropometric Measurements, Nutrition-Focused Physical Findings, and Client History. Nutritional assessment also includes interpretation of data from the screening process as well as a review of entries from other disciplines (such as speech, occupational, or physical therapy) that may affect the evaluation process. Nutritional assessment leads to identification of a nutritional diagnosis or problem that can be resolved or improved through a treatment (nutritional intervention).
Food–Nutrition Related History
The RDN should evaluate the adequacy of the individual’s current and previous food intake and meal pattern including any supplements, food intolerances, allergies, and cultural food preferences.
As part of the nutritional assessment, observation during mealtime gives the healthcare professional the opportunity to determine whether the individual has self-feeding, chewing, or swallowing problems that may require either speech or occupational therapy screening and/or treatment. Inability to feed oneself has been identified as a risk for unintended weight loss.18 Adequate consumption of food and fluid is also a concern for those with swallowing problems, which places them at risk for malnutrition and pressure ulcers. The speech language pathologist (SLP) screens, assesses, and defines the food texture and fluid consistency as well as the need for individualized feeding techniques such as positioning for ease of swallowing. These interventions are implemented by the dining services department and nursing staff and monitored and evaluated by the RDN. For example, individuals may require thickened liquids to prevent aspiration. The occupational therapist determines the appropriate self-help feeding devices to promote eating independence. Similarly, the physical therapy sessions often result in the need for both increased calories and fluid, which the RDN will calculate and arrange to provide in the form of food and/or supplements at appropriate times.
Medications can influence an individual’s nutritional status and have been identified as a cause of weight loss.19 Drugs may either inhibit or induce metabolism of a nutrient or increase the excretion of a nutrient. Medicine designed to calm and reduce agitation may in turn reduce mobility and activity levels and place individuals at risk for pressure ulcer development. Medications may increase or decrease appetite, alter sense of taste or smell, or cause gastric disturbances. Radiation therapy, chemotherapy, and renal dialysis can result in increased nausea and vomiting as well as decreased activity, placing the individual at nutritional risk. Drug therapy may trigger adverse effects; for example, antibiotics often cause nausea and gastric disturbances that curtail an individual’s food and fluid intake. The list of medications that may influence nutrient intake or interfere with nutrition is very long and complicated.20 Consultation with a pharmacist may be helpful.
Biochemical Data
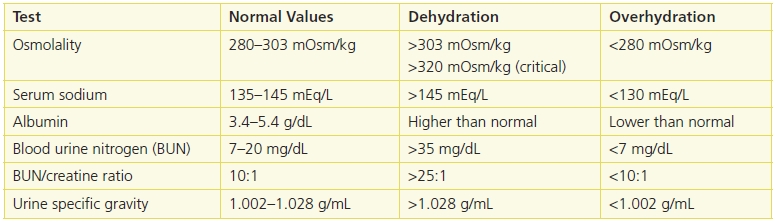
Biochemical tests are evaluated as part of the nutritional assessment process. However, there is no one test specific to nutritional status (Table 10-2).
Table 10-2 Useful Lab Values to Screen for Hydration Status
Albumin is a serum protein with a large body pool size distributed between the vascular and interstitial spaces, with 50% located in extravascular spaces. It functions as a carrier protein and assists in maintaining oncotic pressure. Only 5% of albumin is synthesized every day by the liver; therefore, protein intake does not affect the albumin pool on a daily basis. The majority of the changes in albumin are caused by the redistribution between the intravascular and extravascular spaces. For example, edema, ascites, and overhydration depress albumin levels, and dehydration falsely elevates albumin.
Prealbumin (transthyretin) is a transport protein for thyroxine and a carrier for retinal binding protein. Prealbumin levels are elevated in acute renal failure as the kidneys degrade it. It is also affected by some of the same factors as albumin.
Transferrin has been touted as a marker of nutritional status, but since it is involved in iron transport, its levels are affected by iron status.
Albumin, prealbumin, and transferrin are negative acute-phase reactants that are stimulated by the inflammatory process including infection, trauma, surgery, autoimmune processes, burns, etc. Acute-phase proteins change by approximately 25% during inflammation and are expected to return to normal once the inflammatory response resolves. The response in acute and chronic inflammation is a release of cytokines such as interleukin-6 that is responsible for the production of most acute-phase proteins.21 Cytokines are responsible for fever, inflammation of chronic disease, and cachexia. However, serum albumin levels may drop in as few as 8 hours in severe stress or inflammatory conditions even when protein intake is adequate. The Academy’s Evidence Analysis Library analyzed changes in albumin and prealbumin for several conditions and indicated that these acute-phase proteins do not consistently or predictably change with weight loss, calorie restriction, or nitrogen balance. They reflect severity of the inflammatory response rather than nutritional status. 22 For this reason, a decrease in serum albumin is increasingly seen as a poor reflection of nutritional status.5,23–27 Low serum protein levels may indicate that the individual is ill and therefore at risk for malnutrition. Frequent monitoring of weight status and oral intake would be important, especially if the individual is at risk for impaired skin integrity.
Other biochemical data that should be evaluated include glucose levels (fasting blood sugar and HgbA1c) for persons with diabetes along with renal function to determine if individuals can tolerate the increased protein that is recommended for wound healing.
Anemia, defined as a blood disorder in which there are a reduced number of red blood cells, low hemoglobin, and low hematocrit, can have a negative effect on wound healing. When anemia is present, the blood has reduced oxygen-carrying capacity leading to various side effects and negative consequences such as lower endurance, poor temperature regulation, decreased immune function, increased rates of infection, impaired memory/cognitive function, and possibly increased mortality in the elderly.28 Since impaired wound healing may be a symptom of anemia, establishing the type of deficiency quickly and implementing a nutritional intervention is essential.
The nutritional assessment should focus on identifying risk factors that may contribute to the development of dehydration (Table 10-3). Dehydration can have serious consequences especially for the frail older adult: decreased functional ability, predisposition to falls, infections, and fluid and electrolyte imbalances. The dehydrated individual exhibits unintended weight loss (2%, mild; 5%, moderate; and 8%, severe), dry skin and mucous membranes, rapid pulse, decreased venous pressure, subnormal body temperature, low blood pressure, and altered sensation.
Table 10-3 Signs of Dehydration
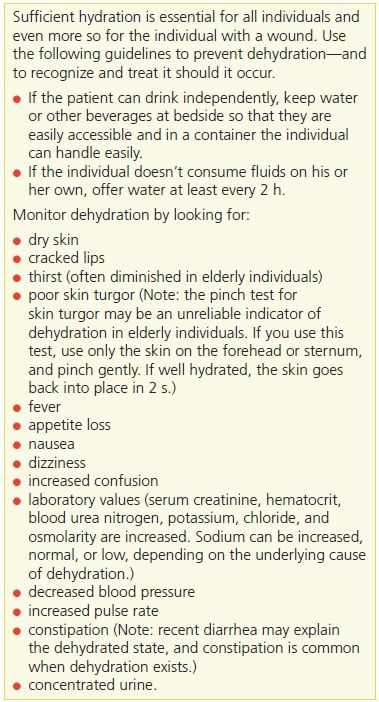
Individuals who are at risk of dehydration require careful monitoring, such as daily weights (Table 10-4). A weight loss of 2 kg in 48 hours indicates a corresponding loss of 2 L of fluid. Elderly patients, whose sense of thirst often declines, should be offered fluids more frequently. The American Medical Directors Association recently published a guideline, which may be helpful to those working with older adults for the management of dehydration.29
Table 10-4 Nutrition Screening
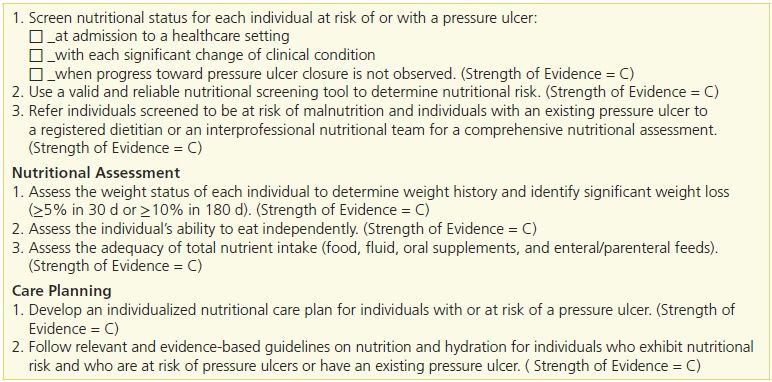
Adapted with permission Haesler, E., ed. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Osborne Park, Western Australia: Cambridge Media, 2014.
Anthropometric Factors
Anthropometry, the measurement of body size, weight, and proportions, is used to evaluate an individual’s nutritional status. A change in anthropometric values can signal problems such as wasting or edema, reflecting nutritional excess or deficit. Accurate heights and weights are critical as they are the basis for determining caloric and nutrient requirements. Adjustment or notations should be made for casts and other appliances that alter true weight.
 Practice Point
Practice Point
Weigh your patient each time on the same scale, at the same time of day, and with minimal clothing. Be careful to subtract wheel chair weights, if weighing on a wheel chair scale. Make sure to note any casts or braces, if you are unable to remove them before taking the weight.
Body mass index (BMI) is a weight-to-height ratio derived from body weight in kilograms divided by the square of the height in meters:

or
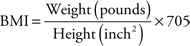
A normally hydrated person with a BMI greater than 30 is considered obese (see Chapter 21, Bariatric Population). A BMI less than 19 is considered underweight for adults and may place the individual at nutritional risk.30
One measurement of determining the severity of undernutrition/malnutrition is any deviation from usual body weight.
For example, a usual body weight of 145 pounds that decreased to 137 pounds in 30-day period is a 5.5% loss.
When evaluating the severity of weight variances, it is important to determine whether the weight loss was intended or unintended. If the weight loss was unintended, it is essential to determine possible causes, such as recent surgery, diuretic therapy, or other new treatments, that may affect weight status. Unintended weight loss can signify malnutrition and increase the risk of mortality. Weight loss, especially in older adults, results in undernutrition and increases the risk of mortality. A 5% loss in 30 days or a 10% decline in 6 months increases the risk of death.31,32
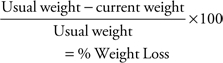
Nutrition-Focused Physical Findings
The RDN and IDT should assess the individual’s skin condition, checking for loss of subcutaneous fat as evidenced by loose skin in the extremities. Observe for listlessness, muscle wasting, and the presence of peripheral edema in the absence of cardiac disease or circulatory disorder. Dull, dry, sparse hair can signify a possible protein–energy deficiency.
The older adult is particularly prone to pressure ulcers as a result of decreased mobility, multiple comorbid conditions, poor nutrition, and loss of muscle mass. In addition to malnutrition, undernutrition, and unintended weight loss, nutritional factors thought to contribute to skin breakdown include protein deficiency, which creates a negative nitrogen balance; anemia, which inhibits the formation of red blood cells; and dehydration, which causes dry, fragile skin.
Immune function declines with age, thus increasing the risk of infection. With advancing age also comes decreased skin response to temperature, pain, and pressure. This affects the skin’s elasticity and the healing process. (For further signs,33 see Table 10-5.)
Table 10-5 Physical Signs of Malnutrition33
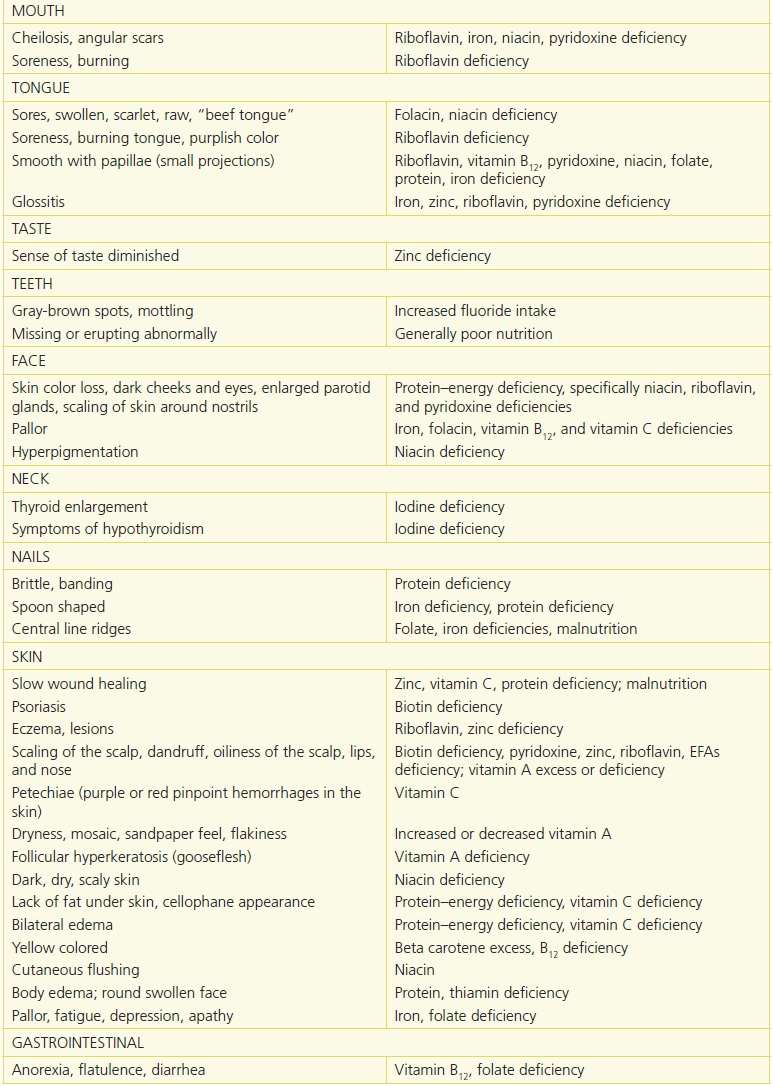
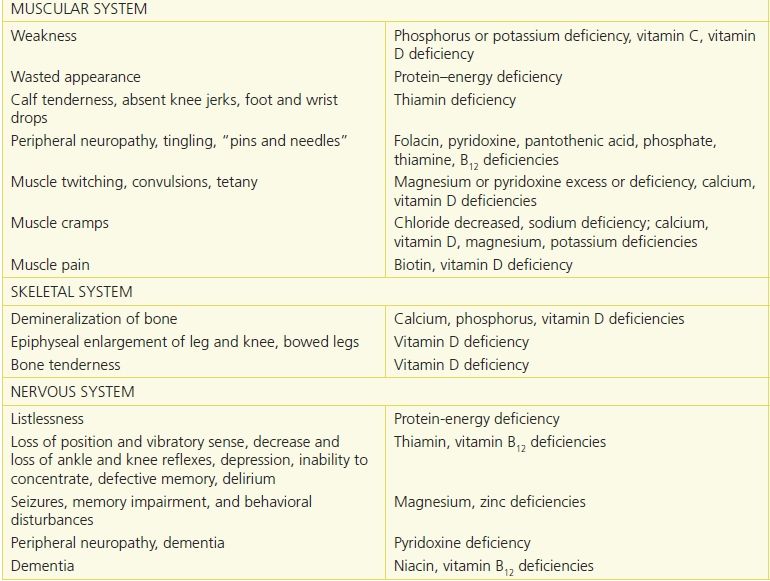
Reprinted from Physical Signs of Malnutrition: Pocket Resource for Nutrition Assessment. Chicago, IL: Dietetics in Health Care Communities, 2013:129–32, with permission.
The nutritional assessment information collected is documented in the medical record, and an individualized interdisciplinary care plan is established.
Table 10-4 outlines nutritional screening, assessing, and care planning recommendations from the 2014 of the National Pressure Ulcer Advisory Panel (NPUAP), European Pressure Ulcer Advisory Panel (EPUAP) and Pan Pacific Pressure Injury Alliance, Prevention and Treatment of Pressure Ulcers Clinical Practice Guidelines.34
Role of Nutrients in Healing
There are six major classes of nutrients: carbohydrates, proteins, fats, vitamins, minerals, and water. Through the process of metabolism, organic nutrients are broken down to yield energy, rearranged to build body structures, or used in chemical reactions for body processes.
Calories
Individuals at risk of malnutrition and pressure ulcers or who currently have wounds require additional calories to compensate for the increased metabolic stress due to hypermetabolism. Stress as a result of injury, surgery, burn, fracture, or wounds results in depletion of the nutrient stores required for healing.
Carbohydrates provide energy and prevent gluconeogenesis, which occurs when the body is forced to convert protein stores for energy. Approximately 50% to 60% of an individual’s total caloric intake should come from carbohydrates. Glucose is the main source of fuel for collagen synthesis required for wound healing. The current recommendation for calories for individuals with pressure ulcers is 30 to 35 calories/kg/body weight34 (Table 10-6).
Table 10-6 Function and Sources of Nutrients
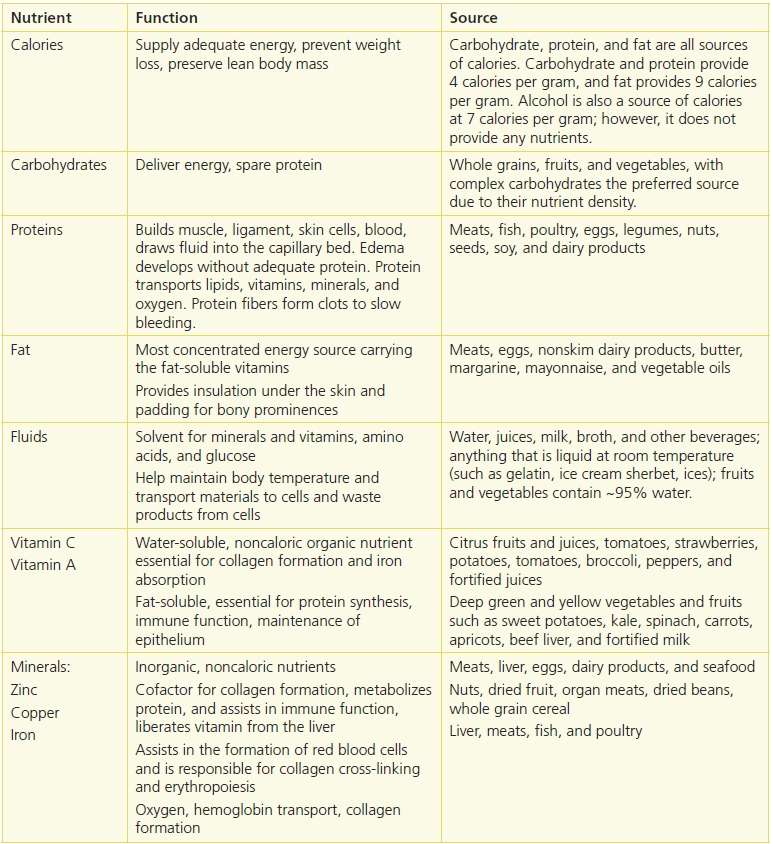
Protein and Amino Acids
Protein accounts for 17% of an individual’s body weight, mainly in the form of lean tissue, muscle, and connective tissue. Half of the body’s protein consists of collagen, actin, and myosin, which provide structure to the body, and hemoglobin, which transports oxygen to the cells. Protein is responsible for repair and synthesis of enzymes involved in wound healing, cell multiplication, and collagen and connective tissue synthesis. It is essential for promoting positive nitrogen balance, and increased protein levels have been linked to improved healing rates.35,36 The recommended dietary allowance (RDA) for all adults, including older adults, is 0.8 g/kg/body weight. Current evidence supports the concept that LBM can be better maintained when an older adult consumes higher levels of protein in the range of 1.0 to 1.2 g/kg/d.37–39 A report by the PROT-AGE Study Group suggested that individuals with severe injury or illness might need 2.0 g/kg/body of protein daily.40 The 2014 NPUAP/EPUAP/PPPIA guideline recommendation is 1.25 to 1.5 g protein/kg body weight for an individual assessed to be at risk for a pressure ulcer and malnutrition and for individuals with pressure ulcers, when it is compatible with goals of care.34 Clinical judgment should be used to determine individual protein requirements, considering the number and severity of wounds, renal function, and comorbidities, as well as tolerance to interventions. For example, high protein levels may not be appropriate for individuals with chronic kidney disease.
When the body is under stress, glutamine, cysteine, and arginine become conditionally indispensable amino acids. L-arginine is composed of 32% nitrogen, and its function is to stimulate the insulinlike growth factor that is involved in wound healing. Arginine enhances immune function and wound collagen deposition in healthy elderly people.41 A 12-week RCT study by Cereda et al. in four nursing homes concluded that the rate of pressure ulcer healing accelerated when a nutritional formula enriched with protein, arginine, zinc, and vitamin C was consumed daily for at least 8 weeks.42 Another RCT by van Anholt et al. investigated the same formula used in the Cereda study to improve healing in well-nourished older adults with stage III and IV pressure ulcers. Participants in the trial were from eight healthcare centers, hospitals, or nursing homes in four European countries. The study concluded that a high-protein supplement with arginine and micronutrients might be associated with improved healing rate in older adults who were not malnourished.43
Fats and Fatty Acids
Fat is the most concentrated source of energy and provides a reserve source of energy in the form of stored triglycerides in adipose tissue. Fat calories should constitute 20% to 25% of total caloric intake. Lean meats, poultry, fish, low-fat dairy products, and vegetable oils are appropriate sources of fat.
Fat-Soluble Vitamins
Fat-soluble vitamins A, D, E, and K remain in the liver and fat tissue of the body until used. Because the body does not excrete excess fat-soluble vitamins, the risk of toxicity from overdose exists.
 Practice Point
Practice Point
Older adults may have a difficult time consuming adequate amounts of calcium, vitamin D, and Vitamin B12 without supplementation. A multivitamin with minerals supplement daily is appropriate for older adults. However, if a vitamin or mineral deficiency is confirmed or the diet intake is extremely inadequate, additional supplementation may be warranted.
Vitamin A is responsible for epithelium maintenance. It also stimulates cellular differentiation in fibroblasts and collagen formation. Vitamin A deficiency, which is uncommon, may result in delayed wound healing and increased susceptibility to infection. The wound healing process may be compromised for individuals taking steroids; however, there is limited research to support mega doses of vitamin A to accelerate healing.
Vitamin E is an antioxidant and is responsible for normal fat metabolism and collagen synthesis. Vitamin E deficiency does not appear to play an active role in wound healing, 44 and it impedes the absorption of vitamin A by reducing the rate of hepatic retinyl ester hydrolysis.45
Water-Soluble Vitamins
Water-soluble vitamins C and B play a role in wound healing. Vitamin C is essential for collagen synthesis. Collagen and fibroblasts compose the basis for the structure of a new wound bed. A deficiency of vitamin C prolongs healing time and contributes to reduced resistance to infection.46 However, there is no clinical evidence that wound healing is improved by providing doses of vitamin C above the dietary reference intake (DRI) of 70 to 90 mg/d. A multicenter, blinded trial of 88 patients with pressure ulcers who were randomized to either 10 or 500 mg of vitamin C twice daily failed to demonstrate any improved healing or closure rate between groups.47
Coenzymes (B vitamins) are necessary for the production of energy from glucose, amino acids, and fat. Pyridoxine (vitamin B6) is important for maintaining cellular immunity and forming red blood cells. Thiamine and riboflavin are needed for adequate cross-linking and collagenation, but their effect has not been demonstrated in pressure ulcers.
Minerals
Minerals also contribute to a patient’s well-being. Zinc, a cofactor for collagen formation, also metabolizes protein, liberates vitamin A from storage in the liver, interacts with platelets in blood clotting, and assists in immune function. Deficiency may occur rapidly through wound drainage or excessive gastrointestinal (GI) fluid loss or from long-term poor dietary intake. Albumin transports zinc through the body, so zinc absorption declines as plasma albumin declines (e.g., with infection, sepsis, or trauma). No clinical evidence exists to support supplementation (such as with zinc sulfate 200 to 300 mg daily, which contains more than 50 mg of elemental zinc). In a small study of individuals with pressure ulcers, no effect on ulcer healing was seen at 12 weeks in zinc-supplemented versus non–zinc-supplemented individuals.48 The DRI for zinc is 8 to 11 mg, and the maximum daily intake or tolerable upper intake level for elemental zinc is 40 mg.49 High serum zinc levels may inhibit healing, impair phagocytosis, and interfere with copper metabolism.50
Copper is essential for preserving the strength of the skin, blood vessels, and epithelial and connective tissue throughout the body. The ratio of copper to zinc is clinically more important than the concentration of either of these trace minerals.
Iron is needed for hemoglobin, collagen formation, and oxygen transport. Iron is essential for new cell generation, amino acids, and hormones. Individuals who consume a diet low in nutrient rich foods, those who are food insecure, or individuals with poor nutrient absorption or metabolism may not be consuming an adequate diet to meet established nutritional reference standards.51
A multivitamin with 100% of the DRI for minerals is the general recommendation if the diet is inadequate or if deficiencies are suspected or confirmed. Many of the oral supplements, enteral formulas, and fortified foods recommended for individuals with wounds contain additional micronutrients that should be considered before recommending additional supplementation.34
Water
Water constitutes about 60% of the adult body weight. It is distributed in the body in three fluid compartments (intracellular, interstitial, and intravascular). Water serves many vital functions in the body, including:
- aiding in hydration of wound sites and in oxygen perfusion
- acting as a solvent for minerals, vitamins, amino acids, glucose, and other small molecules and enabling them to diffuse into and out of cells
- transporting vital materials to cells and removing waste from cells.
Individuals with draining wounds, emesis, diarrhea, elevated temperature, or increased perspiration need additional fluids to replace lost fluid. Individuals on air-fluidized beds may require additional fluids daily. Total fluid needs are met from the water content of food plus liquids. Food accounts for 19% to 27% of the total fluid intake of healthy adults.52 Refer to Estimating How Much Fluid You Need Daily (Table 10-7).
Table 10-7 Estimating How Much Fluid You Need Daily
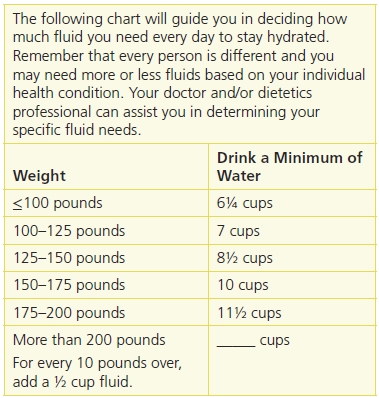
Reprinted from The Complete Guide to Nutrition Care for Pressure Ulcers. Naples, FL: Becky Dorner & Associates, Inc., with permission.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


