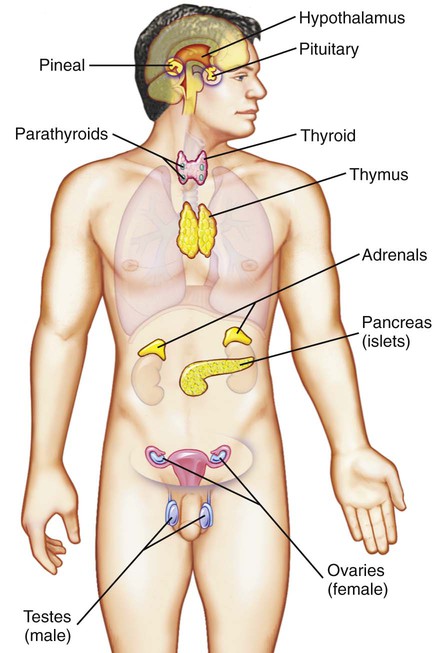
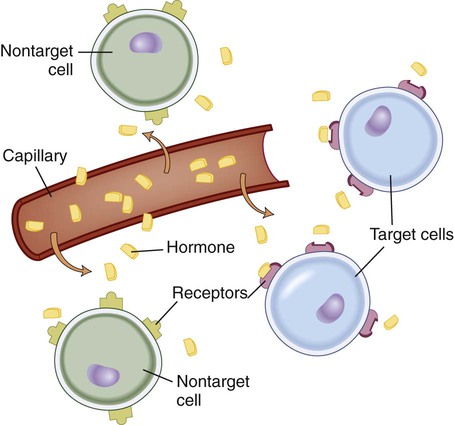
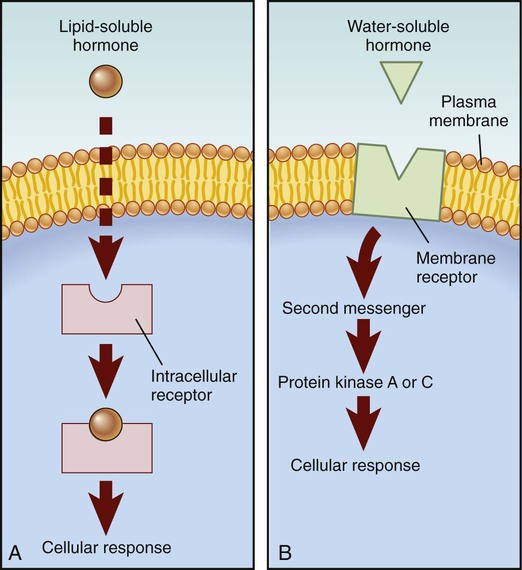
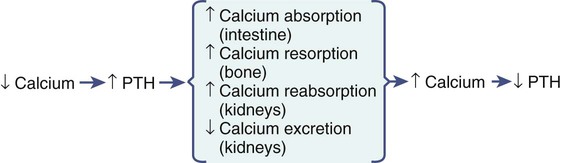
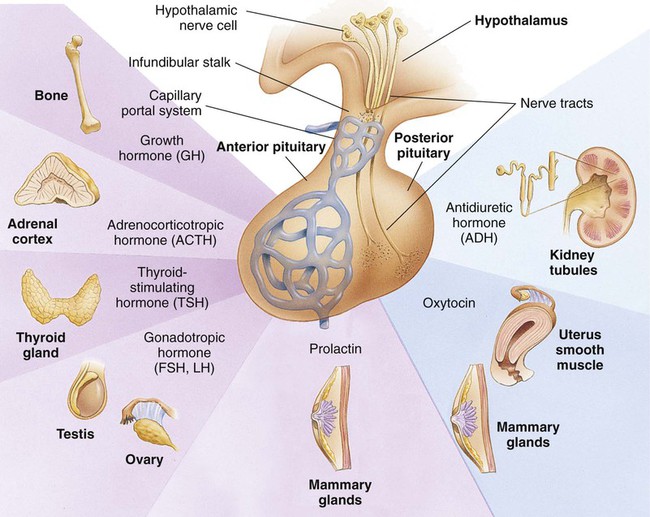
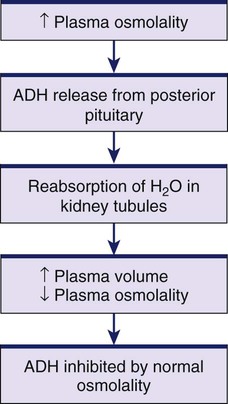
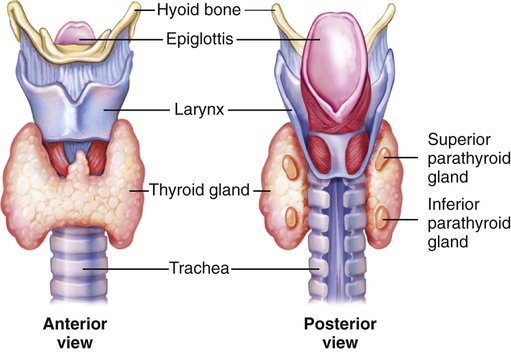
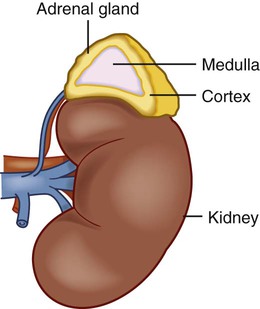
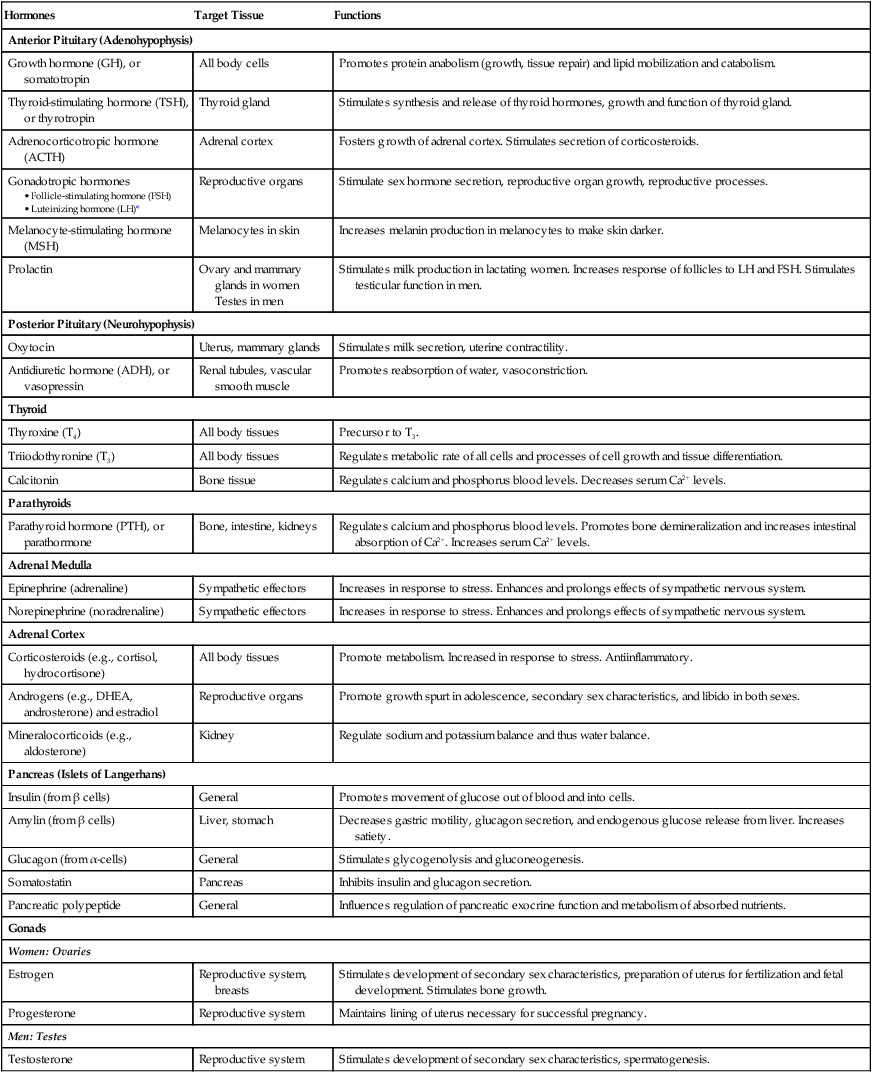
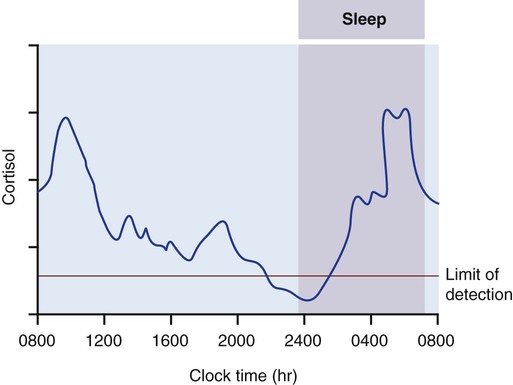
Chapter 48 1. Describe the common characteristics and functions of hormones. 2. Identify the locations of the endocrine glands. 3. Describe the functions of hormones secreted by the pituitary, thyroid, parathyroid, and adrenal glands and the pancreas. 4. Describe the locations and roles of hormone receptors. 5. Select the significant subjective and objective assessment data related to the endocrine system that should be obtained from a patient. 6. Link age-related changes in the endocrine system to differences in assessment findings. 7. Differentiate normal from common abnormal findings of a physical assessment of the endocrine system. 8. Describe the purpose, significance of results, and nursing responsibilities related to diagnostic studies of the endocrine system. Endocrine glands include the hypothalamus, pituitary, thyroid, parathyroids, adrenals, pancreas, ovaries, testes, and pineal gland (Fig. 48-1). Exocrine glands are not part of the endocrine system. They secrete their substances into ducts that then empty into a body cavity or onto a surface. For example, salivary glands produce saliva, which is secreted through salivary ducts into the mouth. Most hormones have common characteristics, including (1) secretion in small amounts at variable but predictable rates; (2) regulation by feedback systems; and (3) binding to specific target cell receptors. Table 48-1 summarizes the major hormones, glands or tissues from which they are synthesized, target organs or tissues, and functions. TABLE 48-1 *In men, sometimes referred to as interstitial cell–stimulating hormone (ICSH). In addition to important physiologic activities, hormones help regulate the nervous system. For example, catecholamines are hormones when they are secreted by the adrenal medulla, but act as neurotransmitters when secreted by nerve cells in the brain and peripheral nervous system. When epinephrine, a catecholamine, travels through the blood, it is a hormone and affects target tissues. When it travels across synaptic junctions, it acts as a neurotransmitter.1 Lipid-soluble hormones are synthesized from cholesterol and are produced by the adrenal cortex, sex glands, and thyroid.2 Lipid-soluble hormones (steroids, thyroid) are relatively small molecules that cross the target cell membrane by simple diffusion. Steroid and thyroid hormone receptors are located inside the cell (Fig. 48-3). Lipid-soluble hormones are bound to plasma proteins for transport in the blood. Although lipid-soluble hormones are inactive when bound to plasma proteins, they can be released when appropriate and immediately exert their action at the target tissue. Water-soluble hormones (insulin, growth hormone [GH], and prolactin) have receptors on or in the cell membrane.3 Water-soluble hormones circulate freely in the blood to their target tissues, where they act. Water-soluble hormones are not dependent on plasma proteins for transport (see Fig. 48-3). The pattern of insulin secretion is a physiologic example of negative feedback between glucose and insulin. Elevated blood glucose levels stimulate the secretion of insulin from the pancreas (see eFig. 48-1 available on the website for this chapter). As blood glucose levels decrease, the stimulus for insulin secretion also decreases. The homeostatic mechanism is considered negative feedback because it reverses the change in blood glucose level. Another example of negative feedback is the relationship between calcium and parathyroid hormone (PTH). Low blood levels of calcium stimulate the parathyroid gland to release PTH, which acts on bone, the intestine, and the kidneys to increase blood calcium levels. The increased blood calcium level then inhibits further PTH release (Fig. 48-4). In addition to chemical regulation, some endocrine glands are directly affected by the activity of the nervous system. Pain, emotion, sexual excitement, and stress can stimulate the nervous system to modulate hormone secretion. Neural involvement is initiated by the central nervous system (CNS) and implemented by the sympathetic nervous system (SNS). For example, stress is sensed or perceived by the CNS with subsequent stimulation of the SNS. The SNS secretes catecholamines that increase heart rate and blood pressure to deal with stress more effectively. (Effects of stress are discussed in Chapter 7.) A common physiologic rhythm is the circadian rhythm. This is an endogenous 24-hour rhythm that can be driven and altered by sleep-wake or dark-light 24-hour (diurnal) cycles. Hormone levels fluctuate predictably during these cycles. For example, cortisol rises early in the day, declines toward evening, and rises again toward the end of sleep to peak by morning (Fig. 48-5). GH, thyroid-stimulating hormone (TSH), and prolactin secretions peak during sleep. The menstrual cycle is an example of a body rhythm that is longer than 24 hours (ultradian). These rhythms must be considered when interpreting laboratory results for hormone levels. (See diagnostic studies section in this chapter and Chapter 51.) Although the pituitary gland has been referred to as the “master gland,” most of its functions rely on its interrelationship with the hypothalamus. Two important groups of hormones from the hypothalamus are releasing hormones and inhibiting hormones. The function of these hormones is to either stimulate the release or inhibit the release of hormones from the anterior pituitary (Table 48-2). TABLE 48-2 The pituitary gland (hypophysis) is located in the sella turcica under the hypothalamus at the base of the brain above the sphenoid bone (see Fig. 48-1). The pituitary is connected to the hypothalamus by the infundibular (hypophyseal) stalk. This stalk relays information between the hypothalamus and the pituitary. The pituitary consists of two major parts, the anterior lobe (adenohypophysis) and the posterior lobe (neurohypophysis). A smaller intermediate lobe produces melanocyte-stimulating hormone. The anterior lobe accounts for 80% of the gland by weight and is regulated by the hypothalamus through releasing and inhibiting hormones. These hypothalamic hormones reach the anterior pituitary through a network of capillaries known as the hypothalamus-hypophyseal portal system. The releasing and inhibiting hormones in turn affect the secretion of six hormones from the anterior pituitary (Fig. 48-6). The posterior pituitary is composed of nerve tissue and is essentially an extension of the hypothalamus. Communication between the hypothalamus and posterior pituitary occurs through nerve tracts known as the median eminence. The hormones secreted by the posterior pituitary, antidiuretic hormone (ADH) and oxytocin, are actually produced in the hypothalamus. These hormones travel down the nerve tracts from the hypothalamus to the posterior pituitary and are stored until their release is triggered by the appropriate stimuli (see Fig. 48-6). The major physiologic role of ADH (also called arginine vasopressin) is regulation of fluid volume by stimulating reabsorption of water in the renal tubules. ADH is also a potent vasoconstrictor. ADH secretion is stimulated by plasma osmolality (a measure of solute concentration of circulating blood) and hypovolemia (Fig. 48-7). Plasma osmolality increases when there is a decrease in ECF or an increase in solute concentration. The increased plasma osmolality activates osmoreceptors, which are extremely sensitive, specialized neurons in the hypothalamus. These activated osmoreceptors stimulate ADH release. Volume receptors in large veins, heart atria, and carotid arteries that sense pressure changes also contribute to ADH control. When ADH is released, the renal tubules reabsorb water and the urine becomes more concentrated. When ADH release is inhibited, renal tubules do not reabsorb water, resulting in a more dilute urine excretion. The thyroid gland is located in the anterior portion of the neck in front of the trachea. It consists of two encapsulated lateral lobes connected by a narrow isthmus (Fig. 48-8). The thyroid gland is a highly vascular organ, and its size is regulated by TSH from the anterior pituitary. The three hormones produced and secreted by the thyroid gland are thyroxine (T4), triiodothyronine (T3), and calcitonin. The adrenal glands are small, paired, highly vascularized glands located on the upper portion of each kidney. Each gland consists of two parts, the medulla and the cortex (Fig. 48-9). Each part has distinct functions, and the glands act independently from one another. The adrenal medulla is the inner part of the gland and consists of sympathetic postganglionic neurons. The medulla secretes the catecholamines epinephrine (adrenaline), norepinephrine (noradrenaline), and dopamine. Catecholamines are synthesized from the amino acid phenylalanine. Catecholamines, usually considered neurotransmitters, are hormones when secreted by the adrenal medulla because they are released into the circulation. They are an essential part of the body’s “fight or flight” response to stress (see Chapter 7). Cortisol, the most abundant and potent glucocorticoid, is necessary to maintain life and protect the body from stress. Cortisol is secreted in a diurnal pattern (see Fig. 48-5). The major control of cortisol is through a negative feedback mechanism that involves the secretion of corticotropin-releasing hormone (CRH) from the hypothalamus. CRH stimulates the secretion of ACTH by the anterior pituitary. Glucocorticoids inhibit the inflammatory response and are considered antiinflammatory. Cortisol decreases the inflammatory response by stabilizing the membranes of cellular lysosomes and preventing increased capillary permeability. The lysosomal stabilization reduces the release of proteolytic enzymes and thereby their destructive effects on surrounding tissue. Cortisol can also inhibit production of prostaglandins, thromboxanes, and leukotrienes (see Chapter 12, Fig. 12-2) and alter the cell-mediated immune response. Normal aging has many effects on the endocrine system (Table 48-3). These include (1) decreased hormone production and secretion, (2) altered hormone metabolism and biologic activity, (3) decreased responsiveness of target tissues to hormones, and (4) alterations in circadian rhythms. TABLE 48-3 GERONTOLOGIC ASSESSMENT DIFFERENCES
Nursing Assessment
Endocrine System
Structures and Functions of Endocrine System
Glands
Hormones
Hormones
Target Tissue
Functions
Anterior Pituitary (Adenohypophysis)
Growth hormone (GH), or somatotropin
All body cells
Promotes protein anabolism (growth, tissue repair) and lipid mobilization and catabolism.
Thyroid-stimulating hormone (TSH), or thyrotropin
Thyroid gland
Stimulates synthesis and release of thyroid hormones, growth and function of thyroid gland.
Adrenocorticotropic hormone (ACTH)
Adrenal cortex
Fosters growth of adrenal cortex. Stimulates secretion of corticosteroids.
Gonadotropic hormones
Reproductive organs
Stimulate sex hormone secretion, reproductive organ growth, reproductive processes.
Melanocyte-stimulating hormone (MSH)
Melanocytes in skin
Increases melanin production in melanocytes to make skin darker.
Prolactin
Ovary and mammary glands in women
Testes in men
Stimulates milk production in lactating women. Increases response of follicles to LH and FSH. Stimulates testicular function in men.
Posterior Pituitary (Neurohypophysis)
Oxytocin
Uterus, mammary glands
Stimulates milk secretion, uterine contractility.
Antidiuretic hormone (ADH), or vasopressin
Renal tubules, vascular smooth muscle
Promotes reabsorption of water, vasoconstriction.
Thyroid
Thyroxine (T4)
All body tissues
Precursor to T3.
Triiodothyronine (T3)
All body tissues
Regulates metabolic rate of all cells and processes of cell growth and tissue differentiation.
Calcitonin
Bone tissue
Regulates calcium and phosphorus blood levels. Decreases serum Ca2+ levels.
Parathyroids
Parathyroid hormone (PTH), or parathormone
Bone, intestine, kidneys
Regulates calcium and phosphorus blood levels. Promotes bone demineralization and increases intestinal absorption of Ca2+. Increases serum Ca2+ levels.
Adrenal Medulla
Epinephrine (adrenaline)
Sympathetic effectors
Increases in response to stress. Enhances and prolongs effects of sympathetic nervous system.
Norepinephrine (noradrenaline)
Sympathetic effectors
Increases in response to stress. Enhances and prolongs effects of sympathetic nervous system.
Adrenal Cortex
Corticosteroids (e.g., cortisol, hydrocortisone)
All body tissues
Promote metabolism. Increased in response to stress. Antiinflammatory.
Androgens (e.g., DHEA, androsterone) and estradiol
Reproductive organs
Promote growth spurt in adolescence, secondary sex characteristics, and libido in both sexes.
Mineralocorticoids (e.g., aldosterone)
Kidney
Regulate sodium and potassium balance and thus water balance.
Pancreas (Islets of Langerhans)
Insulin (from β cells)
General
Promotes movement of glucose out of blood and into cells.
Amylin (from β cells)
Liver, stomach
Decreases gastric motility, glucagon secretion, and endogenous glucose release from liver. Increases satiety.
Glucagon (from α-cells)
General
Stimulates glycogenolysis and gluconeogenesis.
Somatostatin
Pancreas
Inhibits insulin and glucagon secretion.
Pancreatic polypeptide
General
Influences regulation of pancreatic exocrine function and metabolism of absorbed nutrients.
Gonads
Women: Ovaries
Estrogen
Reproductive system, breasts
Stimulates development of secondary sex characteristics, preparation of uterus for fertilization and fetal development. Stimulates bone growth.
Progesterone
Reproductive system
Maintains lining of uterus necessary for successful pregnancy.
Men: Testes
Testosterone
Reproductive system
Stimulates development of secondary sex characteristics, spermatogenesis.
Lipid-Soluble and Water-Soluble Hormones.
Regulation of Hormonal Secretion.
Simple Feedback.
Nervous System Control.
Rhythms.
Hypothalamus
The following hormones from the hypothalamus target the anterior pituitary.
Releasing Hormones
Inhibiting Hormones
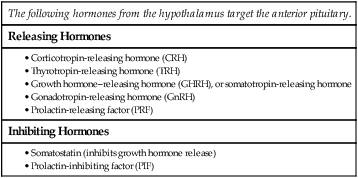
Pituitary
Anterior Pituitary.
Posterior Pituitary.
Thyroid Gland
Adrenal Glands
Adrenal Medulla.
Adrenal Cortex.
Cortisol.
Gerontologic Considerations
Effects of Aging on Endocrine System
Endocrine System
Changes
Clinical Significance
Thyroid
Atrophy of thyroid gland. TSH, T3, and T4 secretion are decreased. Increased nodules.
Increased incidence of hypothyroidism with aging. However, most older adults maintain adequate thyroid function. Thyroid hormone replacement dose lower in older adults.
Parathyroid
Increased secretion of PTH and increased basal level of PTH.
Increased calcium resorption from bone. Hypercalcemia, hypercalciuria (may reflect defective renal mechanism).
Adrenal Cortex
Adrenal cortex becomes more fibrotic and slightly smaller. Decreased metabolism of cortisol. Decreased plasma levels of adrenal androgens and aldosterone.
Decreased metabolic clearance rate for glucocorticoids.
Adrenal Medulla
Increased secretion and basal level of norepinephrine. No change in plasma epinephrine levels.
Decreased responsiveness to β-adrenergic agonists and receptor blockers.
Decreased β-adrenergic receptor response to norepinephrine.
May partly explain increased incidence of hypertension with aging.
Pancreas
Increase in fibrosis and fatty deposits in pancreas. Increased glucose intolerance and decreased sensitivity to insulin.
May partly contribute to increased incidence of diabetes mellitus with advanced aging.
Gonads
Women: Decline in estrogen secretion.
Women experience symptoms associated with menopause and have increased risk for atherosclerosis and osteoporosis.
Men: Decline in testosterone secretion.
Men may or may not experience symptoms. ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Assessment: Endocrine System
Get Clinical Tree app for offline access