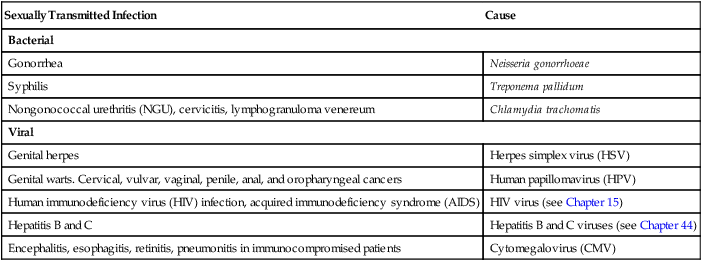
1. Assess the factors contributing to the high incidence of sexually transmitted infections (STIs). 2. Describe the etiology, clinical manifestations, complications, and diagnostic abnormalities of gonorrhea, syphilis, chlamydial infections, genital herpes, and genital warts. 3. Compare and contrast primary genital herpes with recurrent genital herpes. 4. Explain the collaborative care and drug therapy of gonorrhea, syphilis, chlamydial infections, genital herpes, and genital warts. 5. Integrate the nursing assessment and nursing diagnoses for patients who have an STI. 6. Summarize the nursing role in the prevention and control of STIs. Sexually transmitted infections (STIs) are infectious diseases that are commonly acquired through sexual contact (Table 53-1). They may also be contracted by other routes such as through blood, blood products, perinatal transmission, and autoinoculation. STI is becoming the more common term used for sexually transmitted disease. TABLE 53-1 CAUSES OF SEXUALLY TRANSMITTED INFECTIONS In the United States all cases of gonorrhea and syphilis, and in most states chlamydial infection, must be reported to the state or local public health authorities for purposes of surveillance and partner notification. In spite of this requirement, many cases of these infections go unreported. An estimated 65 million Americans are currently infected with one or more STI. Every year an additional 19 million Americans are newly infected with an STI. About 50% of these new cases are in persons 15 to 24 years old.1 The most commonly diagnosed STIs are discussed in this chapter. Human immunodeficiency virus (HIV) infection is discussed in Chapter 15. Hepatitis B and C infections are discussed in Chapter 44. Changes in the methods of contraception are also reflected in the incidence of STIs. The condom is considered to be the best form of protection (other than abstinence) against STIs. Although condom use has increased, condoms are still not used frequently in the general population.2 Commonly used oral contraceptives cause the secretions of the cervix and the vagina to become more alkaline. This change produces a more favorable environment for the growth of organisms that cause STIs at these sites. Women who take oral contraceptives may have a lower risk of pelvic inflammatory disease (PID) as a result of the ability of the cervical mucus to act as a barrier against bacteria. However, the proliferation of Chlamydia organisms, the leading cause of nongonococcal PID, may be enhanced by oral contraceptive use. Gonorrhea is the second most frequently reported STI in the United States (chlamydial infections are the most common). In 2009 the gonorrhea rates were the lowest since recording of rates began. Since that time gonorrhea rates have increased slightly. A total of 309,341 cases of gonorrhea have been reported in the United States.3 Gonorrhea rates are highest in adolescents of all racial and ethnic groups and among African Americans. Most states have enacted laws that permit examination and treatment of minors without parental consent. The initial site of infection in men is usually the urethra. Symptoms of urethritis consist of dysuria and profuse, purulent urethral discharge developing 2 to 5 days after infection (Fig. 53-1). Painful or swollen testicles may also occur. Men generally seek medical evaluation early in the infection because their symptoms are usually obvious and distressing. It is unusual for men with gonorrhea to be asymptomatic.4 Many women who contract gonorrhea are asymptomatic or have minor symptoms that are often overlooked, making it possible for them to remain a source of infection. A few women may complain of vaginal discharge, dysuria, or frequency of urination. Changes in menstruation may be a symptom, but the women often disregard these changes. After the incubation period, redness and swelling occur at the site of contact, which is usually the cervix or urethra (Fig. 53-2). A greenish yellow purulent exudate often develops with a potential for abscess formation. The infection may remain local or can spread by direct tissue extension to the uterus, fallopian tubes, and ovaries. Although the vulva and vagina are uncommon sites for a gonorrheal infection, they may become involved when little or no estrogen is present, as in prepubertal girls and postmenopausal women. Because the vagina acts as a natural reservoir for infectious secretions, transmission is often more efficient from men to women than it is from women to men. Anorectal gonorrhea may be present, usually as a result of anal intercourse. Symptoms may include mucopurulent anal discharge, bleeding, and tenesmus.5 Most patients with anorectal infections and infections in the throat have few symptoms. A small percentage of individuals develop gonococcal pharyngitis from orogenital sexual contact. When the gonococcus can be demonstrated by a laboratory culture, individuals of either gender are infectious to their sexual partners. Because men often seek treatment early in the course of the infection, they are less likely to develop complications. The complications that do occur in men are prostatitis, urethral strictures, and sterility from orchitis or epididymitis. Because women who are asymptomatic seldom seek treatment, complications are more common and usually constitute the reason for seeking medical attention. PID, Bartholin’s abscess, ectopic pregnancy, and infertility are the main complications of gonorrhea in women. A small percentage of infected persons, mainly women, may develop a disseminated gonococcal infection (DGI). In DGI the appearance of skin lesions, fever, arthralgia, arthritis, or endocarditis usually causes the patient to seek medical help (Fig. 53-3). For men, a presumptive diagnosis of gonorrhea is made if there is a history of sexual contact with a new or infected partner followed within a few days by a urethral discharge. Typical clinical manifestations, combined with a positive finding on a Gram-stained smear of the purulent discharge from the penis, give an almost certain diagnosis. A culture of the discharge is indicated for men whose smears are negative in the presence of strong clinical evidence. The nucleic acid amplification test (NAAT) (using ligase or polymerase chain reaction) is a nonculture test with sensitivity similar to culture tests for N. gonorrhoeae. It can be done on a wide variety of samples, including vaginal, endocervical, urethral, and urine specimens.6 Because of a short incubation period and high infectivity, treatment is generally instituted without awaiting culture results. The treatment of gonorrhea in the early stage is curative with a cephalosporin antibiotic. Treatment for gonorrhea is an intramuscular (IM) dose of ceftriaxone (Rocephin) or cefixime (Suprax) orally (Table 53-2). TABLE 53-2 Diagnostic History and physical examination Gram-stained smears of urethral or endocervical exudate Culture for Neisseria gonorrhoeae Nucleic acid amplification test (NAAT) to detect N. gonorrhoeae Testing for other STIs (syphilis, HIV, chlamydial infection) Collaborative Therapy Uncomplicated gonorrhea: ceftriaxone (Rocephin) IM or cefixime (Suprax) orally If chlamydial infection is not ruled out: azithromycin (Zithromax) or doxycycline (Vibramycin) Treatment of sexual contacts Instruction on abstinence from sexual intercourse and alcohol during treatment Reexamination if symptoms persist or recur after completion of treatment Source: Centers for Disease Control and Prevention: Sexually transmitted diseases treatment guidelines, 2010. Retrieved from www.cdc.gov/STD/treatment. Over the years, N. gonorrhoeae has developed a resistance to multiple classes of antimicrobial drugs, including fluoroquinolones (ciprofloxacin [Cipro], ofloxacin [Floxin], levofloxacin [Levaquin]) and tetracyclines (doxycycline [Vibramycin]). Gonococcal resistance to cephalosporin has recently been reported.7 The incidence of syphilis reported in the United States in 2000 was at its lowest rate since reporting started in 1941. During the past decade, syphilis rates increased until 2010 when the rate slightly decreased.1 Many new cases of syphilis are being seen in men who have sex with men. T. pallidum is extremely fragile and easily destroyed by drying, heating, or washing. The incubation period for syphilis ranges from 10 to 90 days (average 21 days). Congenital syphilis is transmitted from an infected mother to the fetus in utero after the tenth week of pregnancy. An infected pregnant woman has a high risk of a stillbirth or a baby dying shortly after birth.8 Pregnant women need to be tested for syphilis at their first prenatal visit. Some states require all women to be screened at delivery. Syphilis has a variety of signs and symptoms that can mimic a number of other diseases. Consequently, compared with other STIs, it is more difficult to recognize syphilis. If it is not treated, specific clinical stages are characteristic of the progression of the disease (Table 53-3). TABLE 53-3 *Several forms such as cardiovascular syphilis and neurosyphilis occur together in approximately 25% of untreated cases. Neurosyphilis causes degeneration of the brain with mental deterioration. Problems related to sensory nerve involvement are a result of tabes dorsalis (progressive locomotor ataxia). There may be sudden attacks of pain anywhere in the body, which can confuse the diagnosis with other conditions. Loss of vision and sense of position in the feet and legs can also occur. Walking may become even more difficult as joint stability is lost. (Late syphilis is also discussed in Chapter 59.) Diagnostic studies for syphilis are presented in Table 53-4. The presence of spirochetes on dark-field microscopy and direct fluorescent antibody (DFA) tests of lesion exudate or tissue can confirm a clinical diagnosis of syphilis. However, syphilis is more commonly diagnosed by a serologic test.4 Tests for syphilis may be classified as those performed for screening and those performed for confirmation of a positive screening test. Nonspecific antitreponemal antibodies can be detected by tests such as the Venereal Disease Research Laboratory (VDRL) test and the rapid plasma reagin (RPR) test. These nontreponemal tests are suitable for screening purposes, and usually become positive 10 to 14 days after the appearance of a chancre. The fluorescent treponemal antibody absorption (FTA-Abs) test and the T. pallidum particle agglutination (TP-PA) test detect specific antitreponemal antibodies and are used for confirming the diagnosis. TABLE 53-4 *If treatment involves alternative antibiotics or treatment failure has occurred. Table 53-4 describes collaborative care of syphilis. Specific management is based on the symptoms. Management of syphilis is aimed at eradicating all syphilitic organisms. Penicillin G benzathine (Bicillin) or aqueous procaine penicillin G is the treatment of choice for all stages of syphilis.9 When penicillin is contraindicated, doxycycline or tetracycline may be used. However, treatment cannot reverse damage that is already present in the late stage of the disease. It is also important that all sexual contacts in the last 90 days be treated.
Nursing Management
Sexually Transmitted Infections
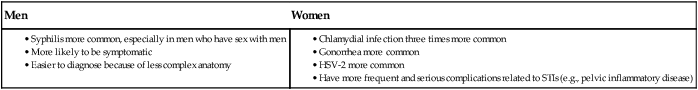
Sexually Transmitted Infection
Cause
Bacterial
Gonorrhea
Neisseria gonorrhoeae
Syphilis
Treponema pallidum
Nongonococcal urethritis (NGU), cervicitis, lymphogranuloma venereum
Chlamydia trachomatis
Viral
Genital herpes
Herpes simplex virus (HSV)
Genital warts. Cervical, vulvar, vaginal, penile, anal, and oropharyngeal cancers
Human papillomavirus (HPV)
Human immunodeficiency virus (HIV) infection, acquired immunodeficiency syndrome (AIDS)
HIV virus (see Chapter 15)
Hepatitis B and C
Hepatitis B and C viruses (see Chapter 44)
Encephalitis, esophagitis, retinitis, pneumonitis in immunocompromised patients
Cytomegalovirus (CMV)
Factors Affecting Incidence of Sexually Transmitted Infections
Bacterial Infections
Gonorrhea
Clinical Manifestations
Men.
Women.
General.
Complications
Diagnostic Studies
Collaborative Care
Drug Therapy.
Syphilis
Etiology and Pathophysiology
Clinical Manifestations
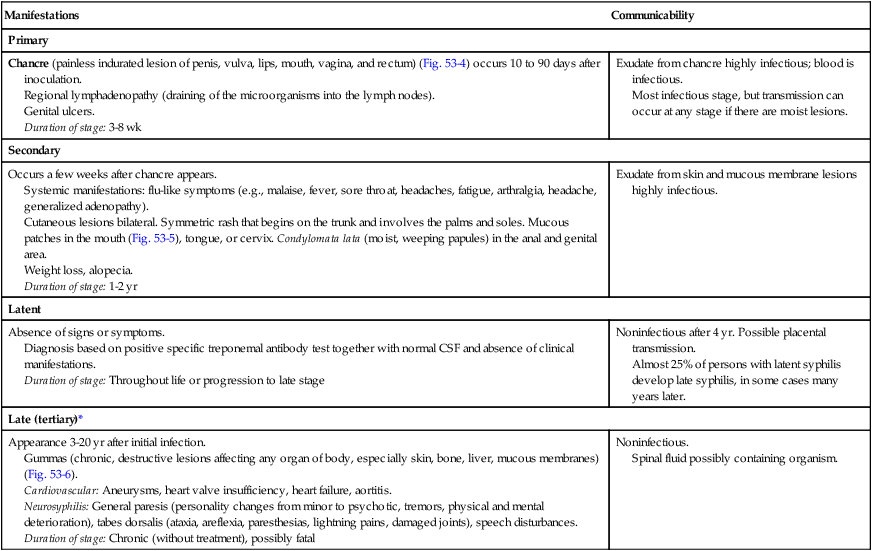
Manifestations
Communicability
Primary
Chancre (painless indurated lesion of penis, vulva, lips, mouth, vagina, and rectum) (Fig. 53-4) occurs 10 to 90 days after inoculation.
Regional lymphadenopathy (draining of the microorganisms into the lymph nodes).
Genital ulcers.
Duration of stage: 3-8 wk
Exudate from chancre highly infectious; blood is infectious.
Most infectious stage, but transmission can occur at any stage if there are moist lesions.
Secondary
Occurs a few weeks after chancre appears.
Systemic manifestations: flu-like symptoms (e.g., malaise, fever, sore throat, headaches, fatigue, arthralgia, headache, generalized adenopathy).
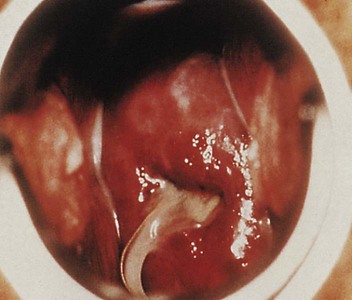
Cutaneous lesions bilateral. Symmetric rash that begins on the trunk and involves the palms and soles. Mucous patches in the mouth (Fig. 53-5), tongue, or cervix. Condylomata lata (moist, weeping papules) in the anal and genital area.
Weight loss, alopecia.
Duration of stage: 1-2 yr
Exudate from skin and mucous membrane lesions highly infectious.
Latent
Absence of signs or symptoms.
Diagnosis based on positive specific treponemal antibody test together with normal CSF and absence of clinical manifestations.
Duration of stage: Throughout life or progression to late stage
Noninfectious after 4 yr. Possible placental transmission.
Almost 25% of persons with latent syphilis develop late syphilis, in some cases many years later.
Late (tertiary)*
Appearance 3-20 yr after initial infection.
Gummas (chronic, destructive lesions affecting any organ of body, especially skin, bone, liver, mucous membranes) (Fig. 53-6).
Cardiovascular: Aneurysms, heart valve insufficiency, heart failure, aortitis.
Neurosyphilis: General paresis (personality changes from minor to psychotic, tremors, physical and mental deterioration), tabes dorsalis (ataxia, areflexia, paresthesias, lightning pains, damaged joints), speech disturbances.
Duration of stage: Chronic (without treatment), possibly fatal
Noninfectious.
Spinal fluid possibly containing organism.

Complications
Diagnostic Studies
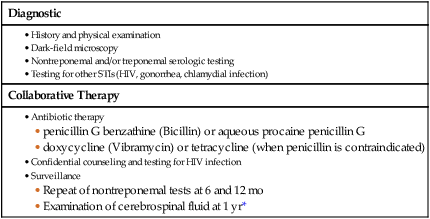
Diagnostic
Collaborative Therapy
Collaborative Care
Drug Therapy.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Management: Sexually Transmitted Infections
Get Clinical Tree app for offline access