Nonopioid and Opioid Analgesics
Objectives
• Differentiate between acute and chronic pain.
• Compare indications for nonopioid and opioid analgesics.
• Describe the serum therapeutic ranges of acetaminophen and aspirin.
• Contrast the side effects of aspirin and opioids.
• Explain the methadone treatment program.
• Discuss nursing interventions and patient teaching related to nonopioid and opioid analgesics.
• Apply the nursing process to the patient with patient-controlled analgesia.
Key Terms
addiction, p. 358
adjuvant analgesics, p. 363
analgesics, p. 353
cluster headaches, p. 366
endorphins, p. 353
migraine headaches, p. 365
neuropathic pain, p. 353
nociceptors, p. 353
nonopioid analgesics, p. 354
nonsteroidal antiinflammatory drugs, p. 353
opioid agonist, p. 356
opioid agonist-antagonist, p. 363
opioid antagonist, p. 365
orthostatic hypotension, p. 360
pain threshold, p. 353
pain tolerance, p. 353
patient-controlled analgesia, p. 362
withdrawal syndrome, p. 360
![]() http://evolve.elsevier.com/KeeHayes/pharmacology/
http://evolve.elsevier.com/KeeHayes/pharmacology/
Pain is an unpleasant sensory and emotional experience related to tissue injury. Due to the subjective nature of pain, the nurse must be knowledgeable and skillful in the assessment and measurement of pain to achieve optimal pain management.
Pain management is regarded as such a significant component of nursing care that pain has become known as the “fifth vital sign.” The Joint Commission (TJC) has incorporated the assessment, documentation, and management of pain into its 2003 standards, which reflects the importance of this vital sign. The nurse’s role is to assess the patient’s pain level, alleviate the patient’s pain through nonpharmacologic and pharmacologic treatments, thoroughly document the patient’s response to treatment, and teach patients and their significant others to manage pain control themselves when appropriate.
An individual’s pain threshold reflects the level of stimulus needed to create a painful sensation. Individual genetic makeup contributes to the variations in pain threshold from person to person. The mu (µ) opioid receptor gene controls the number of µ receptors present. When an individual has a large amount of µ receptors, the pain threshold is high and pain sensitivity is reduced.
The amount of pain a person can endure without having it interfere with normal functioning is called pain tolerance. This psychological aspect of pain varies greatly in individuals, because it is very subjective. Pain tolerance is influenced by factors such as age, gender, culture, ethnicity, previous experience, anxiety level, and specific circumstances.
Analgesics, both nonopioid and opioid, are prescribed for the relief of pain. The choice of analgesic depends upon the severity of the pain. Mild to moderate pain is frequently relieved with the use of nonopioid (also known as nonnarcotic) analgesics. Moderate to severe pain usually requires an opioid (also known as narcotic) analgesic.
Drugs used for pain relief are presented in this chapter. Many of the same nonopioid analgesics that are taken for pain, such as the nonsteroidal antiinflammatory drugs (NSAIDs), are also taken for antiinflammatory purposes. This application for these drugs is covered in Chapter 25.
The most common classification of pain is by duration. Acute pain can be mild, moderate, or severe and is usually associated with a specific tissue injury. The onset of acute pain is usually sudden and of short duration. Chronic pain usually has a vague origin and onset with a prolonged duration.
Pain may also be classified by its origin. Nociceptors (sensory pain receptors) are activated by noxious stimuli (mechanical, thermal, and chemical) in peripheral tissues. When tissue damage occurs, injured cells release chemical mediators that affect the exposed nerve endings of the nociceptors. Pain that originates from tissue injury is nociceptor pain, which includes somatic (structural tissues: bones, muscles) and visceral (organ) pain. Neuropathic pain is an unusual sensory disturbance often involving neural supersensitivity. This pain is due to injury or disease of the peripheral or central nervous system (CNS). The patient with neuropathic pain usually complains of burning, tingling, or electrical shocks in the affected area, often triggered by light touch. Diabetic neuropathy associated with diabetes mellitus is an example of peripheral neuropathic pain. Severe, intractable pain from a herniated disk or spinal cord injury is evidence of neuropathic pain in the CNS.
Pathophysiology
The most common pain theory is called the gate theory, proposed by Melzack and Wall in 1965. According to this theory, tissue injury activates nociceptors and causes the release of chemical mediators such as substance P, prostaglandins, bradykinin, histamine, serotonin, acetylcholine, glutamate, adenosine triphosphate, leukotrienes, and potassium. These substances initiate an action potential along a sensory nerve fiber and sensitize pain receptors. Nociceptive action potentials are transmitted via afferent nerve fibers. One type of pain fiber that primarily transmits impulses from the periphery is the A delta (δ) fiber. Because A δ pain fibers are wrapped in a myelin sheath, they transmit impulses rapidly in acute pain. The C fiber is a type of pain fiber that is small and unmyelinated, and because C fibers are unmyelinated, they transmit impulses slowly. C fibers are more often associated with chronic, dull pain.
A pain signal begins at the nociceptors in the periphery and proceeds throughout the CNS. Knowing how and where pharmacologic agents work is essential to controlling pain. The body produces neurohormones called endorphins (peptides) that naturally suppress pain conduction, although the method is not completely understood. Opioids such as morphine activate the same receptors as endorphins to reduce pain. NSAIDs control pain at the peripheral level by blocking the action of cyclooxygenase (pain-sensitizing chemical) and interfering with the production of prostaglandins. Cortisone decreases pain by blocking the action of phospholipase, reducing the production of both prostaglandins and leukotrienes. In neuropathic pain, anticonvulsant drugs prevent the production of nerve impulses by stabilizing the neuronal membrane and inactivating peripheral sodium channels.
To ascertain severity of pain, the health care provider should ask the patient to rate the degree of pain on a scale of 1 to 10, with 10 being the worst or most severe pain. The patient’s comfort level should also be determined. A patient who indicates a pain level of 9 may verbalize a decrease in pain to a level of 3 within 30 to 45 minutes after receiving pain medication. Table 26-1 lists the types of pain and the drug groups that may be effective in relieving each type of pain.
TABLE 26-1

Undertreatment of Pain
Undertreatment of pain is a major issue in health care today. The National Pharmaceutical Council and TJC state that up to 75% of patients have unrelieved pain. Some reasons for undertreatment are sociocultural variables that mediate a patient’s willingness to acknowledge being in pain, the patient’s inability to describe pain, the nurse’s inability to measure pain, lack of regular pain assessment rounds, attitudes of the health care team, an unwillingness to believe the patient’s report of pain, inaccurate knowledge of the health care provider concerning addiction and tolerance, and prescription of an inadequate analgesic dose. Many scales and instruments are available to the nurse for assessment and measurement of the patient’s pain level.
Unrelieved pain leads to a multitude of harmful effects involving almost all organs of the body. As a result of unrelieved pain, the patient may develop increased respiratory rate and heart rate, hypertension, increased stress response, urinary retention, fluid overload, electrolyte imbalance, glucose intolerance, hyperglycemia, pneumonia, atelectasis, anorexia, paralytic ileus, constipation, weakness, confusion, and infection.
In addition to psychological and physical suffering, inadequate pain management leads to high health care costs. It is estimated the cost of extended hospital stays, readmissions to the hospital, and outpatient visits due to inadequate pain management exceeds $100 billion per year.
Nonopioid Analgesics
Nonopioid analgesics (aspirin, acetaminophen, ibuprofen, naproxen) are less potent than opioid analgesics. They are used to treat mild to moderate pain. Nonopioids are usually purchased over-the-counter (OTC), but COX-2 inhibitors require a prescription. Nonopioids are effective for the dull, throbbing pain of headaches, dysmenorrhea (menstrual pain), inflammation, minor abrasions, muscular aches and pain, and mild to moderate arthritis. Most analgesics also have an antipyretic effect and will lower an elevated body temperature. Some, such as aspirin, have antiinflammatory and antiplatelet effects as well.
Nonsteroidal Antiinflammatory Drugs
All NSAIDs have an analgesic effect as well as an antipyretic and antiinflammatory action. NSAIDs such as aspirin (ASA), ibuprofen (Motrin, Advil), and naproxen (Aleve) can be purchased as OTC drugs. Aspirin, a salicylate NSAID, is the oldest nonopioid analgesic drug still in use. Adolf Bayer marketed the original formulation in 1899, and currently aspirin can be purchased under many names and with added ingredients. Examples are Bufferin, Ecotrin (enteric-coated tablet), Anacin (containing caffeine), and Alka-Seltzer.
Aspirin should not be used in children younger than 12 years of age, and it is contraindicated for any elevated temperature, regardless of the cause, because of the danger of Reye’s syndrome (neurologic problems associated with viral infection treated with salicylates). In these circumstances, acetaminophen (Tylenol) is recommended instead of aspirin.
In addition to its analgesic, antipyretic, and antiinflammatory properties, aspirin decreases platelet aggregation (clotting). Some health care providers may therefore prescribe one 81-mg, 162-mg, or 325-mg aspirin tablet every day or one 325-mg tablet every other day as a preventive measure against transient ischemic attacks (TIAs, or “small strokes”), heart attacks, or any thromboembolic episode. Aspirin is discussed in depth in Chapter 25 along with other NSAIDs.
Aspirin and other NSAIDs relieve pain by inhibiting biosynthesis of prostaglandin by different forms of the enzyme cyclooxygenase (COX). Inhibition of COX-2 decreases inflammation and pain, but inhibition of COX-1 decreases protection of the stomach lining. As a result of an NSAID’s inhibition of COX-1, stomach ulcers and bleeding may occur. Aspirin is the drug of choice for alleviating pain and inflammation in arthritic conditions, but when given in high doses, severe GI problems develop in approximately 20% of patients. Some pharmaceutical companies have developed antiinflammatory and analgesic drugs that inhibit only COX-2. The COX-2 inhibitors were developed to eliminate the GI side effects associated with aspirin and other NSAIDs. COX-2 inhibitors are discussed in depth in Chapter 25.
Side Effects and Adverse Reactions
A common side effect of NSAIDs is gastric irritation. These drugs should be taken with food, at mealtime, or with a full glass of fluid to help reduce this problem.
If an NSAID is taken for dysmenorrhea during the first 2 days of menstruation, excess bleeding might occur (more so with aspirin than with ibuprofen).
Some patients are hypersensitive to aspirin. Tinnitus, vertigo, bronchospasm, and urticaria are some of the symptoms that indicate hypersensitivity or overdose of the salicylate product. Certain foods also contain salicylates: prunes, raisins, paprika, and licorice. Those with a hypersensitivity to aspirin and salicylate products may be sensitive to other NSAIDs. This hypersensitivity may be related to inhibition of the enzyme cyclooxygenase by the salicylate product.
Acetaminophen
The analgesic acetaminophen (paraaminophenol derivative) is a popular nonprescription drug for the relief of pain, discomfort, and fever in infants, children, adults, and older adults. Acetaminophen is a nonopioid drug, but it is not an NSAID. Acetaminophen does not have the antiinflammatory properties of aspirin, so it is not the drug of choice for any inflammatory process. It constitutes 25% of all OTC drugs sold. Examples of OTC products that contain acetaminophen include Anacin; Excedrin; Midol: Maximum Strength Menstrual Formula; and Vicks: Cold & Flu Relief. Examples of prescription products on the market that contain acetaminophen include Lortab, Percocet, and Vicodin. Acetaminophen (Tylenol), first marketed in the mid-1950s, is an analgesic and antipyretic drug used for muscular aches and pains and for fever caused by viral infections. It is a safe, effective drug when used at therapeutic doses. It causes little to no gastric distress and does not interfere with platelet aggregation. An IV formulation was FDA approved in 2010 for treating pain and fever. There is no link between acetaminophen and Reye’s syndrome, and it does not increase the potential for excessive bleeding if taken for dysmenorrhea, as do aspirin and NSAIDs (Prototype Drug Chart 26-1).
Pharmacokinetics
Acetaminophen is well absorbed from the gastrointestinal (GI) tract. Rectal absorption may be erratic because of the presence of fecal material or a decrease in blood flow to the colon. Because of acetaminophen’s short half-life, it can be administered every 4 hours as needed with a maximum dose of 4 g/day. However, it is suggested that a patient who frequently takes acetaminophen limit the dose to 2000 mg/day (2 g/day) to avoid the possibility of hepatic or renal dysfunction. More than 85% of acetaminophen is metabolized to drug metabolites by the liver.
Large doses or overdoses can be toxic to the hepatic cells, so when large doses are administered over a long period, the serum level of acetaminophen should be monitored. The therapeutic serum range is 10 to 25 mcg/mL. Liver enzyme levels (aspartate aminotransferase [AST], alanine aminotransferase [ALT], alkaline phosphatase [ALP]) and serum bilirubin should also be monitored. Large doses of acetaminophen with regular alcohol intake may lead to liver injury. When acetaminophen toxicity occurs, acetylcysteine (Mucomyst) is the antidote, which reduces liver injury by converting toxic metabolites to a nontoxic form.
Pharmacodynamics
Acetaminophen weakly inhibits prostaglandin synthesis, which decreases pain sensation. It is effective in eliminating mild to moderate pain and headaches and is useful for its antipyretic effect. Acetaminophen does not possess antiinflammatory action. Its onset of action is rapid, and the duration of action is 5 hours or less. Severe adverse reactions may occur with an overdose, so acetaminophen in liquid or chewable form should be kept out of children’s reach.
Side Effects and Adverse Reactions
An overdose of acetaminophen can be extremely toxic to liver cells, causing hepatotoxicity. Death could occur in 1 to 4 days from hepatic necrosis. If a child or adult ingests excessive amounts of acetaminophen tablets or liquid, a poison control center should be contacted immediately and the child or adult should be taken to the emergency department. Early symptoms of hepatic damage include nausea, vomiting, diarrhea, and abdominal pain.
Table 26-2 lists the commonly used nonopioid analgesics and their dosages, uses, and considerations.
TABLE 26-2
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Paraaminophenol | ||
| acetaminophen | See Prototype Drug Chart 26-1. | |
| NSAIDs | ||
| aspirin (Bayer, Ecotrin) | Analgesic: A: PO/PR: 325 to 650 mg, q4h; max: 4 g/d C: PO/PR: 10-15 mg/kg/d q4-6h; max: 4 g/d | Effective in relieving headaches, muscle pain, inflammation and pain from arthritis; mild anticoagulant. Can displace other highly protein-bound drugs. If taken with acetaminophen, GI bleeding could result. Side effects: gastric discomfort, tinnitus, vertigo, deafness (reversible), increased bleeding. Should be taken with foods or at mealtime. Should not be taken with alcohol. Pregnancy category: D; PB: 80%-90%;  : 15-20 min : 15-20 min |
| diflunisal (Dolobid) | A: PO: Initially 1000 mg; maint: 500 mg q12h; max: 1500 mg/d Older adults: PO: Initially 500 mg; maint: 250 q8-12h; max: 1500 mg/d | Used for mild to moderate pain. Considered to be less toxic than aspirin. Pregnancy category: C; PB: 99%,  : 8-12 h : 8-12 h |
| Propionic Acid | ||
| ibuprofen (Motrin, Advil) ibuprofen: IV injection (Caldolor) | Pain: A: PO: 400 mg q4-6h; max: 3200 mg/d A: IV: 400-800 mg over 30 min q6h Fever: A: IV: 400 mg over 30 min q4-6h PRN | For mild to moderate muscle aches and pains. Causes some gastric distress but less than aspirin. Should be taken with food, at mealtime, or with plenty of fluids. Pregnancy category: C (D, third trimester); PB: 90%-99%;  : 2-4 h : 2-4 h |
| naproxen (Naprosyn) | Mild to moderate pain: A: PO: initially 500 mg, then 250 mg q6-8h; max: 1250 mg/d | Treatment of inflammation and pain from osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, gout, and dysmenorrhea. Pregnancy category: C; PB: 99%;  : 12-17 h : 12-17 h |
| ketorolac (Toradol) | A: PO: 10 mg q6h PRN; max: 40 mg/d Older adults: PO: 10 mg q4-6h PRN; max: 40 mg/d A: IM/IV: 30-60 mg q6h PRN; max: 120 mg/d Older adults: IM/IV: 15 mg q6h PRN; max: 60 mg/d | For short-term pain management (5 days or less). Pregnancy category: C; PB: 99%;  : 2.5-9 h : 2.5-9 h |
| Oxicams | ||
| meloxicam (Mobic) | A: PO: Initially 7.5-15 mg/d; max: 15 mg/d | Treatment of pain from osteoarthritis. Pregnancy category: C (first and second trimester), D (third trimester); PB: 99%;  : 15-20 h : 15-20 h |
| Naphthylalkanones | ||
| nabumetone (Relafen) | A: PO: 1000 mg/d or 500 mg b.i.d.; max: 2000 mg/d | Treatment of pain from osteoarthritis, rheumatoid arthritis. Pregnancy category: C (D, third trimester); PB: 99%;  : 24 h : 24 h |
| COX-2 Inhibitors | ||
| celecoxib (Celebrex) | A: PO: 100-400 mg b.i.d.; max: 800 mg/d Older adults: 100-200 mg b.i.d.; max: 400 mg/d | Treatment of osteoarthritis and rheumatoid arthritis. Not indicated for patients <18 y. Use caution for patients with severe renal or liver disorders and for those allergic to sulfonamides. Pregnancy category: C (D, third trimester); PB: 97%;  : 11.2 h : 11.2 h |
| Miscellaneous | ||
| tramadol (Ultram) tramadol ER (Ultram ER, Ryzolt) | A: PO: Initially: 25 mg/d, maint: 50-100 mg q4-6h PRN; max: 400 mg/d A >75 y: max: 300 mg/d A: PO: ER: 100 mg/d; max: 300 mg/d | Used for moderate to severe pain. Contraindicated in severe alcoholism or with use of opioids. Nausea, vomiting, dizziness, constipation, headache, anxiety, and seizures may occur. Pregnancy category: C; PB: 20%;  : 6.3 h for immediate release, 7.9 h for ER : 6.3 h for immediate release, 7.9 h for ER |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 : 2-4 h
: 2-4 h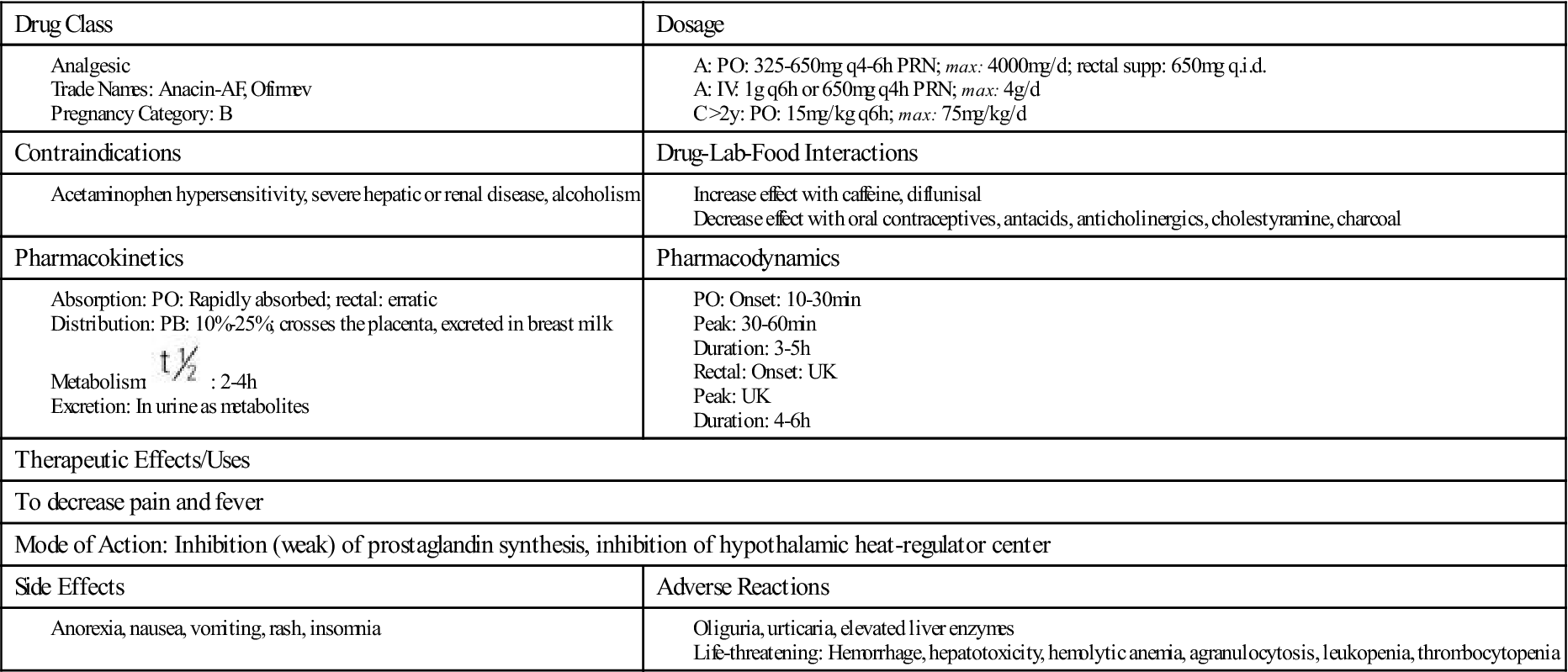
 , half-life; UK, unknown; y, year; <, less than; >, greater than.
, half-life; UK, unknown; y, year; <, less than; >, greater than.















