Endocrine Drugs
Pituitary, Thyroid, Parathyroid, and Adrenal Disorders
Objectives
• Compare the hormones secreted from the adenohypophysis and the neurohypophysis.
• Differentiate the side effects of thyroxine (T4) and triiodothyronine (T3).
Key Terms
acromegaly, p. 743
Addison’s disease, p. 751
adenohypophysis, p. 743
adrenal glands, p. 751
adrenocorticotropic hormone, p. 743
antidiuretic hormone, p. 745
corticosteroids, p. 751
cretinism, p. 747
Cushing’s syndrome, p. 751
diabetes insipidus, p. 745
endocrine, p. 743
gigantism, p. 743
glucocorticoids, p. 752
Graves’ disease, p. 748
hyperthyroidism, p. 748
hypophysis, p. 743
hypothyroidism, p. 747
mineralocorticoids, p. 755
myxedema, p. 747
neurohypophysis, p. 745
parathyroid hormone, p. 749
thyroid-stimulating hormone, p. 743
thyrotoxicosis, p. 748
thyroxine, p. 746
triiodothyronine, p. 746
![]() http://evolve.elsevier.com/KeeHayes/pharmacology/
http://evolve.elsevier.com/KeeHayes/pharmacology/
This chapter describes drugs used for hormonal replacement and for inhibition of hormonal secretion from the pituitary, thyroid, parathyroid, and adrenal glands. Before reading Chapters 51 and 52, review the introduction to Unit XVII, which describes the locations of the endocrine glands and the hormones they secrete. Knowledge of the various endocrine (ductless glands that produce internal secretions that flow to all parts of the body) hormones and their functions facilitates an understanding of the drugs that act on the endocrine glands.
Pituitary Gland
Anterior Lobe
The pituitary gland, or hypophysis, has an anterior and a posterior lobe. The anterior pituitary gland, called the adenohypophysis, secretes the following hormones that target glands and tissues:
• Growth hormone (GH), which stimulates growth in tissue and bone
• Thyroid-stimulating hormone (TSH), which acts on the thyroid gland
• Adrenocorticotropic hormone (ACTH), which stimulates the adrenal gland
Drugs with adenohypophyseal properties used to stimulate or inhibit glandular activity are discussed according to their therapeutic use. The negative feedback system that controls the amount of hormonal secretion from the pituitary gland and the target gland is discussed in the introduction to Unit XVII.
Growth Hormone
Two hypothalamic hormones regulate GH: (1) growth hormone–releasing hormone (GH-RH) and (2) growth hormone–inhibiting hormone (GH-IH; somatostatin). Growth hormone does not have a specific target gland. It affects body tissues and bone; GH replacement stimulates linear growth when there is a GH deficiency. Growth hormone drugs cannot be given orally, because they are inactivated by gastrointestinal enzymes. Subcutaneous (subQ) or intramuscular (IM) administration of GH is necessary.
If a child’s height is well below the standard for a specified age, GH deficiency may be diagnosed, and dwarfism can result. Growth hormone replacement is very expensive; therefore, various tests are performed to determine if this therapy is essential. Because GH acts on newly forming bone, it must be administered before the epiphyses are fused. Administration of GH over several years can increase height by a foot. Prolonged GH therapy can antagonize insulin secretion and eventually cause diabetes mellitus. Athletes should be advised not to take GH to build muscle and physique because of its effects on blood sugar and other side effects.
Drug Therapy: Growth Hormone Deficiency
Somatropin (Genotropin) is a growth hormone used to treat growth failure in children because of pituitary GH deficiency. Somatropin is a product that has the identical amino acid sequence as human growth hormone. Somatropin is contraindicated in pediatric patients who have growth deficiency due to Prader-Willi syndrome and are severely obese or who have severe respiratory impairment, because fatalities associated with these risk factors have been reported.
Drug Therapy: Growth Hormone Excess
Gigantism (excessive growth during childhood) and acromegaly (excessive growth after puberty) can occur with GH hypersecretion and are frequently caused by a pituitary tumor. If the tumor cannot be destroyed by radiation, the prolactin-release inhibitor bromocriptine can inhibit the release of GH from the pituitary gland.
Octreotide (Sandostatin) is a potent synthetic somatostatin used to suppress GH release. It can be used alone or with surgery or radiation. This drug is expensive. GI side effects are common. This drug can also be used for severe diarrhea resulting from carcinoid tumors.
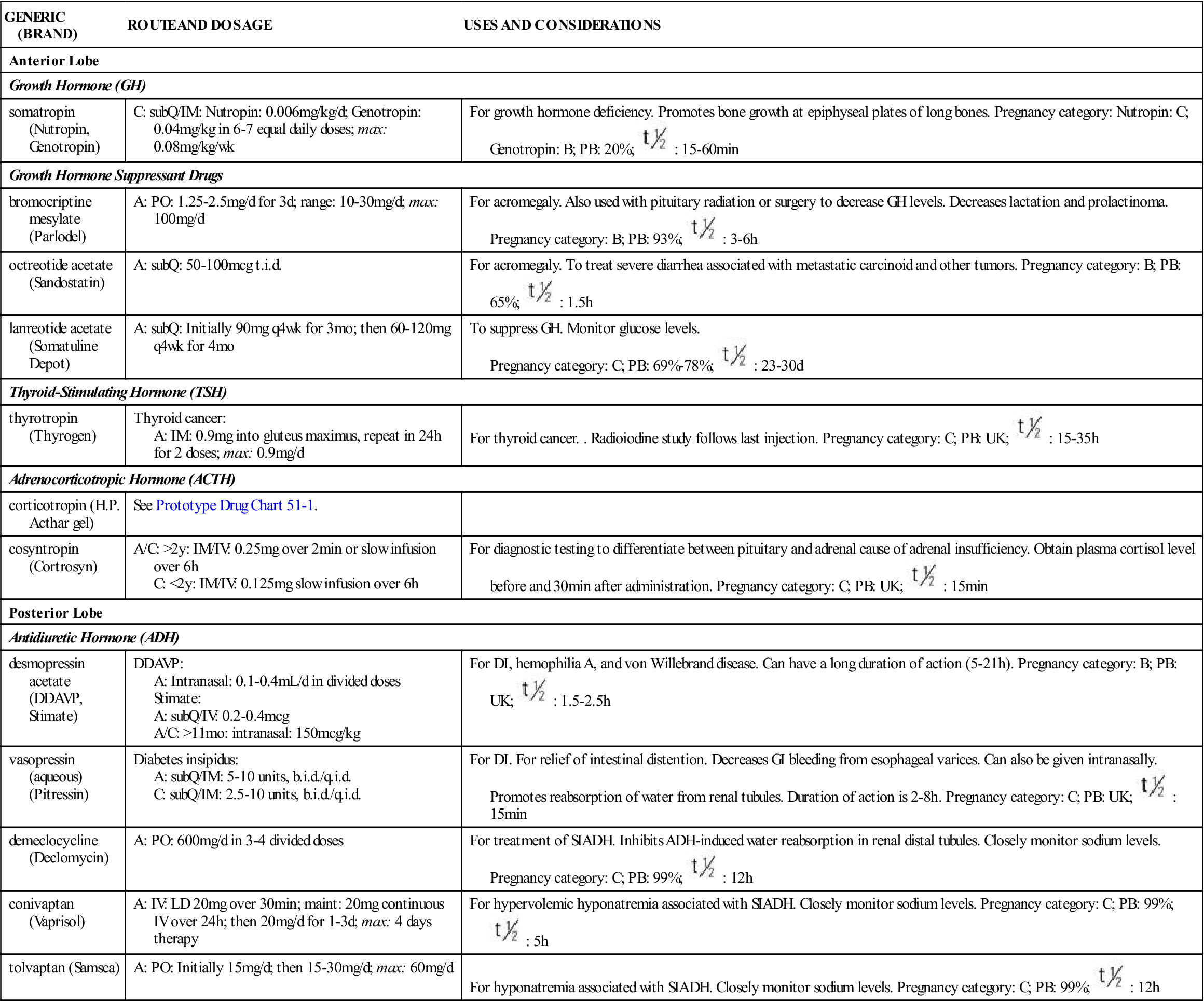
Table 51-1 lists the drugs used to replace or inhibit GH and their dosages, uses, and considerations.
TABLE 51-1
ANTERIOR AND POSTERIOR PITUITARY HORMONES
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Anterior Lobe | ||
| Growth Hormone (GH) | ||
| somatropin (Nutropin, Genotropin) | C: subQ/IM: Nutropin: 0.006 mg/kg/d; Genotropin: 0.04 mg/kg in 6-7 equal daily doses; max: 0.08 mg/kg/wk | For growth hormone deficiency. Promotes bone growth at epiphyseal plates of long bones. Pregnancy category: Nutropin: C; Genotropin: B; PB: 20%;  : 15-60 min : 15-60 min |
| Growth Hormone Suppressant Drugs | ||
| bromocriptine mesylate (Parlodel) | A: PO: 1.25-2.5 mg/d for 3 d; range: 10-30 mg/d; max: 100 mg/d | For acromegaly. Also used with pituitary radiation or surgery to decrease GH levels. Decreases lactation and prolactinoma. Pregnancy category: B; PB: 93%;  : 3-6 h : 3-6 h |
| octreotide acetate (Sandostatin) | A: subQ: 50-100 mcg t.i.d. | For acromegaly. To treat severe diarrhea associated with metastatic carcinoid and other tumors. Pregnancy category: B; PB: 65%;  : 1.5 h : 1.5 h |
| lanreotide acetate (Somatuline Depot) | A: subQ: Initially 90 mg q4wk for 3 mo; then 60-120 mg q4wk for 4 mo | To suppress GH. Monitor glucose levels. Pregnancy category: C; PB: 69%-78%;  : 23-30 d : 23-30 d |
| Thyroid-Stimulating Hormone (TSH) | ||
| thyrotropin (Thyrogen) | Thyroid cancer: A: IM: 0.9 mg into gluteus maximus, repeat in 24 h for 2 doses; max: 0.9 mg/d | For thyroid cancer. . Radioiodine study follows last injection. Pregnancy category: C; PB: UK;  : 15-35 h : 15-35 h |
| Adrenocorticotropic Hormone (ACTH) | ||
| corticotropin (H.P. Acthar gel) | See Prototype Drug Chart 51-1. | |
| cosyntropin (Cortrosyn) | A/C: >2 y: IM/IV: 0.25 mg over 2 min or slow infusion over 6 h C: <2 y: IM/IV: 0.125 mg slow infusion over 6 h | For diagnostic testing to differentiate between pituitary and adrenal cause of adrenal insufficiency. Obtain plasma cortisol level before and 30 min after administration. Pregnancy category: C; PB: UK;  : 15 min : 15 min |
| Posterior Lobe | ||
| Antidiuretic Hormone (ADH) | ||
| desmopressin acetate (DDAVP, Stimate) | DDAVP: A: Intranasal: 0.1-0.4 mL/d in divided doses Stimate: A: subQ/IV: 0.2-0.4 mcg A/C: >11 mo: intranasal: 150 mcg/kg | For DI, hemophilia A, and von Willebrand disease. Can have a long duration of action (5-21 h). Pregnancy category: B; PB: UK;  : 1.5-2.5 h : 1.5-2.5 h |
| vasopressin (aqueous) (Pitressin) | Diabetes insipidus: A: subQ/IM: 5-10 units, b.i.d./q.i.d. C: subQ/IM: 2.5-10 units, b.i.d./q.i.d. | For DI. For relief of intestinal distention. Decreases GI bleeding from esophageal varices. Can also be given intranasally. Promotes reabsorption of water from renal tubules. Duration of action is 2-8 h. Pregnancy category: C; PB: UK;  : 15 min : 15 min |
| demeclocycline (Declomycin) | A: PO: 600 mg/d in 3-4 divided doses | For treatment of SIADH. Inhibits ADH-induced water reabsorption in renal distal tubules. Closely monitor sodium levels. Pregnancy category: C; PB: 99%;  : 12 h : 12 h |
| conivaptan (Vaprisol) | A: IV: LD 20 mg over 30 min; maint: 20 mg continuous IV over 24 h; then 20 mg/d for 1-3 d; max: 4 days therapy | For hypervolemic hyponatremia associated with SIADH. Closely monitor sodium levels. Pregnancy category: C; PB: 99%;  : 5 h : 5 h |
| tolvaptan (Samsca) | A: PO: Initially 15 mg/d; then 15-30 mg/d; max: 60 mg/d | For hyponatremia associated with SIADH. Closely monitor sodium levels. Pregnancy category: C; PB: 99%;  : 12 h : 12 h |
Thyroid-Stimulating Hormone
The adenohypophysis secretes thyroid-stimulating hormone (TSH) in response to thyroid-releasing hormone (TRH) from the hypothalamus, and TSH stimulates the thyroid gland to release thyroxine (T4) and triiodothyronine (T3, or liothyronine). Excess TSH secretion can cause hyperthyroidism, and a TSH deficit can cause hypothyroidism. Hypothyroidism may be caused by a thyroid gland disorder (primary cause) or a decrease in TSH secretion (secondary cause). Thyrotropin (Thytropar), a purified extract of TSH, is used as a diagnostic agent to differentiate between primary and secondary hypothyroidism (see Table 51-1).
Adrenocorticotropic Hormone
The hypothalamus releases corticotropin-releasing factor (CRF), which stimulates the pituitary corticotrophs to secrete adrenocorticotropic hormone (ACTH). ACTH secretion stimulates the release of glucocorticoids (cortisol), mineralocorticoids (aldosterone), and androgen from the adrenal cortex. Usually ACTH and cortisol secretions follow a diurnal rhythm in which the ACTH and cortisol secretion is higher in the early morning and then decreases throughout the day. Stresses such as surgery, sepsis, and trauma override the diurnal rhythm, causing an increase in secretions of ACTH and cortisol.
The ACTH drug corticotropin (Acthar) is used to diagnose adrenal gland disorders, to treat adrenal gland insufficiency, and as an antiinflammatory drug in the treatment of allergic response. Administration of ACTH intravenously (IV) should increase the serum cortisol level in 30 to 60 minutes if the adrenal gland is functioning. If steroid deficiency is caused by pituitary insufficiency, ACTH should eventually stimulate cortisol production. ACTH decreases the symptoms of multiple sclerosis during its exacerbation phase. Prototype Drug Chart 51-1 lists the pharmacologic data for repository corticotropin.
Pharmacokinetics
Corticotropin stimulates the adrenal gland to secrete corticosteroids. The aqueous and gel preparations are well absorbed into the circulation. Zinc is added to some formulations to slow the absorption rate. A portion of the drug is bound to protein; however, the percentage is unknown. The half-life of the drug is 15 to 20 minutes. It is excreted in the urine.
Pharmacodynamics
Corticotropin suppresses the inflammatory and immune responses. It is also prescribed to treat adrenal insufficiency secondary to inadequate corticotropin secretion. The drug is administered IM and IV. Its onset of action, peak concentration time, and duration of action are prolonged when it is injected IM. The IV preparation is in aqueous form; therefore its actions are faster than those of the gel and zinc-additive preparations.
Drug Interactions.
Corticotropin has numerous drug interactions. Diuretics and anti-Pseudomonas penicillins such as piperacillin can decrease the serum potassium level (hypokalemia). If the patient is taking a digitalis preparation and hypokalemia is present, digitalis toxicity can result. Phenytoin, rifampin, and barbiturates increase the metabolic rate, which can decrease the effect of the ACTH drug. Persons with diabetes may need increased insulin and oral antidiabetic (hypoglycemic) drugs because ACTH stimulates cortisol secretion, which increases the blood sugar level.
Posterior Lobe
The posterior pituitary gland, known as the neurohypophysis, secretes antidiuretic hormone (ADH) (vasopressin) and oxytocin. (Oxytocin is discussed in Chapter 54.)
ADH promotes water reabsorption from the renal tubules to maintain water balance in the body fluids. When there is a deficiency of ADH, large amounts of water are excreted by the kidneys. This condition, called diabetes insipidus (DI), can lead to severe fluid volume deficit and electrolyte imbalances. Head injury and brain tumors resulting in trauma to the hypothalamus and pituitary gland can also cause DI. Fluid and electrolyte balance must be closely monitored in these patients, and ADH replacement may be needed. The ADH preparations vasopressin (Pitressin) and desmopressin acetate (DDAVP) can be administered intranasally or by injection.
When there is excess secretion of ADH from the posterior pituitary gland, the most common cause is small cell carcinoma of the lung. Medications, other malignancies, and stressors (e.g., pain, infection, anxiety, trauma) may also be causative factors. These conditions lead to an excessive amount of water retention expanding the intracellular volume. This increased fluid volume causes enhanced glomerular filtration and decreased tubular sodium reabsorption. Natriuresis (excretion of urinary sodium) results, leading to hyponatremia.
SIADH can be treated by fluid restriction, demeclocycline, conivaptan, and tolvaptan. Serum sodium levels must be monitored closely. Table 51-1 lists the drugs used for pituitary disorders and their dosages, uses, and considerations.
Thyroid Gland
Thyroxine (T4) and triiodothyronine (T3) are secreted by the thyroid gland. The functions of T4 and T3 are to regulate protein synthesis and enzyme activity and to stimulate mitochondrial oxidation. Approximately 20% of circulating T3 is secreted from the thyroid gland, and 80% of T3 comes from the degradation of about 40% of T4, which occurs in the periphery. T4 and T3 are carried in the blood by thyroxine-binding globulin (TBG) and albumin, which protect the hormones from being degraded. T3 is more potent than T4, and only unbound free T3 and T4 are active and produce a hormonal response.
Feedback mechanisms regulate T4 and T3 secretion from the thyroid gland. The hypothalamus releases thyrotropin-releasing hormone (TRH), which stimulates the release of TSH from the pituitary gland. TSH stimulates the synthesis and release of T4 and T3 from the thyroid gland. Excess free T4 and T3 inhibit the hypothalamus-pituitary-thyroid (HPT) axis, which results in decreased TRH and TSH secretion. Likewise, too low an amount of T4 and T3 increases the function of the HPT axis.
For thyroid deficiency (hypothyroidism), synthetic T4 and T3 may be prescribed, either alone or in combination. When the thyroid gland secretes an overabundance of thyroid hormones (hyperthyroidism), antithyroid drugs are usually indicated.
Hypothyroidism
Hypothyroidism, a decrease in thyroid hormone secretion, can have either a primary cause (thyroid gland disorder) or a secondary cause (lack of TSH secretion). Primary hypothyroidism occurs more frequently. Decreased T4 and elevated TSH levels indicate primary hypothyroidism, the causes of which are acute or chronic inflammation of the thyroid gland, radioiodine therapy, excess intake of antithyroid drugs, and surgery. Myxedema is severe hypothyroidism in the adult; symptoms include lethargy, apathy, memory impairment, emotional changes, slow speech, deep coarse voice, edema of the eyelids and face, dry skin, cold intolerance, slow pulse, constipation, weight gain, and abnormal menses. In children, hypothyroidism can have a congenital (cretinism) or prepubertal (juvenile hypothyroidism) onset. Drugs containing T4 and T3, alone or in combination, are used to treat hypothyroidism.
Drug Therapy: Hypothyroidism
Levothyroxine sodium (Synthroid) is the drug of choice for replacement therapy for the treatment of hypothyroidism. It increases the levels of T3 and T4. Levothyroxine is also used to treat simple goiter and chronic lymphocytic (Hashimoto) thyroiditis.
Liothyronine (Cytomel) is a synthetic T3 that has a short half-life and duration of action; it is not recommended for maintenance therapy. Liothyronine is better absorbed from the GI tract than levothyroxine, and because of its rapid onset of action and short half-life, it is frequently used as initial therapy for treating myxedema.
Liotrix (Thyrolar) is a mixture of levothyroxine sodium and liothyronine sodium in a 4 : 1 ratio. For treating hypothyroidism, there is no significant advantage to using liotrix over levothyroxine sodium alone, because levothyroxine converts T4 to T3 in the peripheral tissues.
Prototype Drug Chart 51-2 lists the pharmacologic data for levothyroxine.

 , half-life; t.i.d., three times a day; UK, unknown; wk, week; y, year; >, greater than; <, less than.
, half-life; t.i.d., three times a day; UK, unknown; wk, week; y, year; >, greater than; <, less than. : 15-20 min
: 15-20 min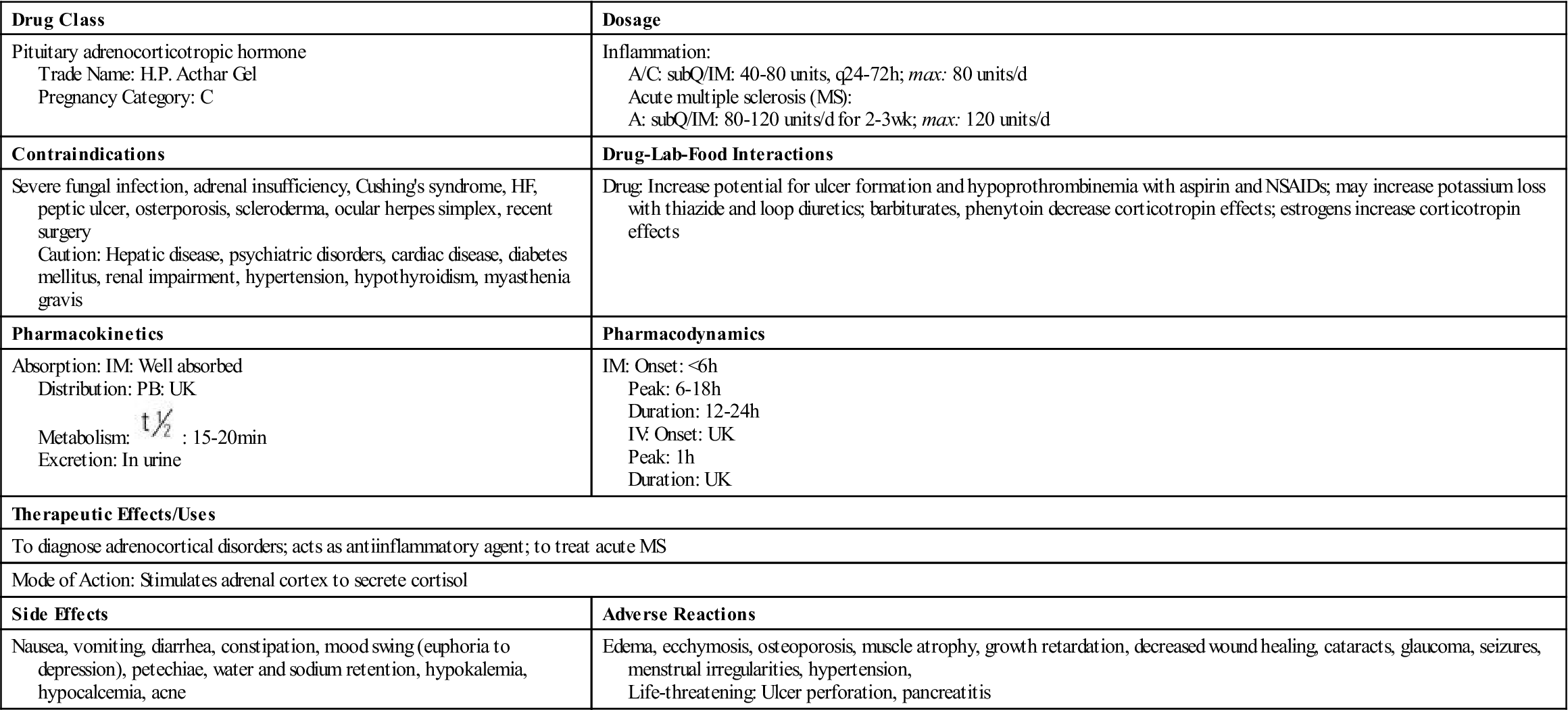
 , half-life; UK, unknown; wk, week; <, less than.
, half-life; UK, unknown; wk, week; <, less than.























 -1 h before eating
-1 h before eating : 6-7 days
: 6-7 days

