Diuretics
Objectives
• Compare the action and uses of thiazide, loop, and potassium-sparing diuretics.
• Apply the nursing process for the patient taking thiazide, loop, and potassium-sparing diuretics.
Key Terms
antihypertensive, p. 621
diuresis, p. 620
diuretics, p. 620
hypercalcemia, p. 622
hyperglycemia, p. 623
hyperkalemia, p. 629
hypertension, p. 620
hyperuricemia, p. 623
hypokalemia, p. 624
natriuresis, p. 621
natriuretic, p. 625
oliguria, p. 623
osmolality, p. 626
potassium-sparing diuretics, p. 621
potassium-wasting diuretics, p. 621
saluretic, p. 625
Diuretics are used for two main purposes: to decrease hypertension (lower blood pressure) and to decrease edema (peripheral and pulmonary) in heart failure (HF) and renal or liver disorders. Hypertension is an elevated blood pressure. Diuretics discussed in this chapter are used either alone or in combination to decrease blood pressure and edema.
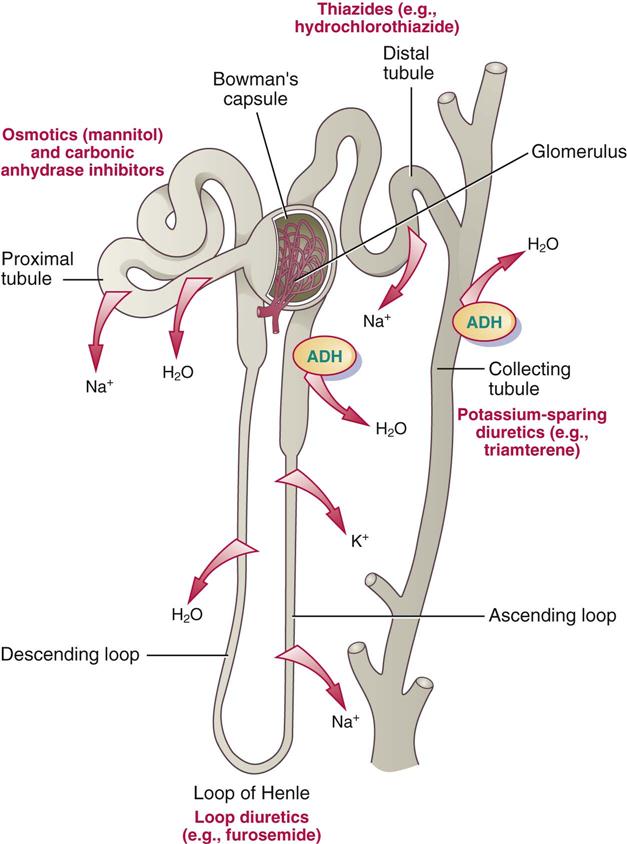
Diuretics produce increased urine flow, or diuresis, by inhibiting sodium and water reabsorption from the kidney tubules. Most sodium and water reabsorption occurs throughout the renal tubular segments (proximal, loop of Henle [descending loop and ascending loop], and collecting tubule). Diuretics can affect one or more segments of the renal tubules. Figure 43-1 illustrates the renal tubule along with the normal process of water and electrolyte reabsorption and diuretic effects on the tubules.
Every 1.5 hours, the total volume of the body’s extracellular fluid (ECF) goes through the kidneys (glomeruli) for cleansing; this is the first process for urine formation. Small particles such as electrolytes, drugs, glucose, and waste products from protein metabolism are filtered in the glomeruli. Larger products such as protein and blood cells are not filtered with normal renal function, and they remain in the circulation. Sodium and water are the largest filtrate substances.
Normally 99% of the filtered sodium that passes through the glomeruli is reabsorbed; 50% to 55% of sodium reabsorption occurs in the proximal tubules, 35% to 40% in the loop of Henle, 5% to 10% in the distal tubules, and <3% in the collecting tubules. Diuretics that act on the tubules closest to the glomeruli have the greatest effect in causing natriuresis (sodium loss in the urine). A classic example is the osmotic diuretic mannitol. The diuretic effect depends on the drug reaching the kidneys and its concentration in the renal tubules.
Diuretics have an antihypertensive effect because they promote sodium and water loss by blocking sodium and chloride reabsorption. This causes a decrease in fluid volume, lowering blood pressure. With fluid loss, edema (fluid retention in body tissues) should decrease, but if sodium is retained, water is also retained, and blood pressure increases.
Many diuretics cause the loss of other electrolytes, including potassium, magnesium, chloride, and bicarbonate. The diuretics that promote potassium excretion are classified as potassium-wasting diuretics, and those that promote potassium retention are called potassium-sparing diuretics.
The following five categories of diuretics are effective in removing water and sodium:
Thiazide, loop, and potassium-sparing diuretics are most frequently prescribed for hypertension and for edema associated with HF. Except for those in the potassium-sparing group, all diuretics are potassium-wasting.
Combination diuretics that contain both potassium-wasting and potassium-sparing drugs have been marketed primarily for the treatment of hypertension. Combinations have an additive effect in reducing blood pressure and are discussed in more detail in the Potassium-Sparing Diuretics section later in this chapter. Chapter 44 takes a closer look at the combinations of antihypertensive agents with hydrochlorothiazide (HCTZ).
Thiazides and Thiazide-Like Diuretics
The first thiazide, chlorothiazide (Diuril), was marketed in 1957 and followed a year later by hydrochlorothiazide. There are numerous thiazide and thiazide-like preparations. Thiazides act on the distal convoluted renal tubule, beyond the loop of Henle, to promote sodium, chloride, and water excretion. Thiazides are used to treat hypertension and peripheral edema. They are not effective for immediate diuresis and should not be used to promote fluid loss in patients with severe renal dysfunction. Table 43-1 lists thiazide and thiazide-like diuretics and their dosages, uses, and considerations. Drug dosages for hypertension and edema are similar.
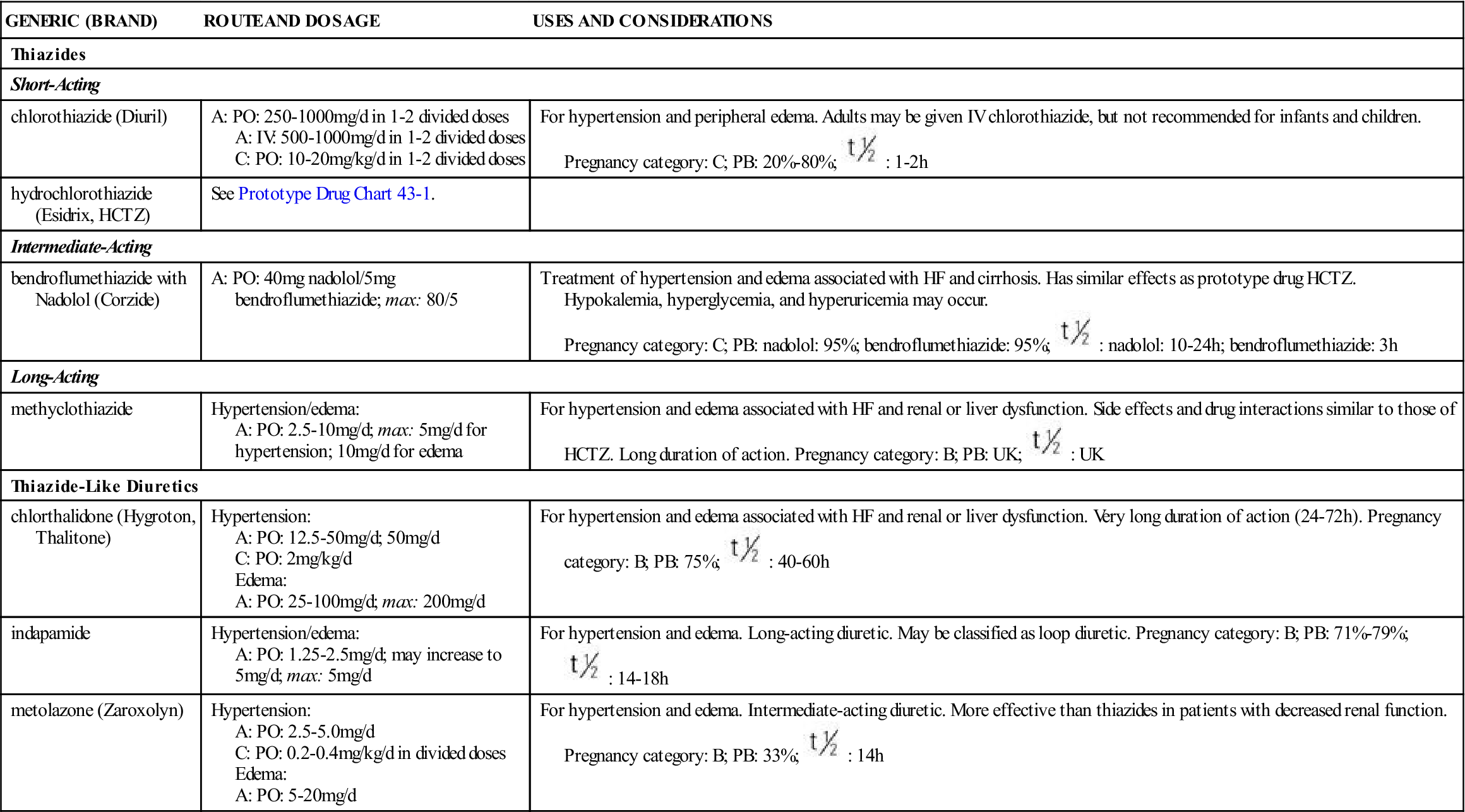
TABLE 43-1
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Thiazides | ||
| Short-Acting | ||
| chlorothiazide (Diuril) | A: PO: 250-1000 mg/d in 1-2 divided doses A: IV: 500-1000 mg/d in 1-2 divided doses C: PO: 10-20 mg/kg/d in 1-2 divided doses | For hypertension and peripheral edema. Adults may be given IV chlorothiazide, but not recommended for infants and children. Pregnancy category: C; PB: 20%-80%;  : 1-2 h : 1-2 h |
| hydrochlorothiazide (Esidrix, HCTZ) | See Prototype Drug Chart 43-1. | |
| Intermediate-Acting | ||
| bendroflumethiazide with Nadolol (Corzide) | A: PO: 40 mg nadolol/5 mg bendroflumethiazide; max: 80/5 | Treatment of hypertension and edema associated with HF and cirrhosis. Has similar effects as prototype drug HCTZ. Hypokalemia, hyperglycemia, and hyperuricemia may occur. Pregnancy category: C; PB: nadolol: 95%; bendroflumethiazide: 95%;  : nadolol: 10-24 h; bendroflumethiazide: 3 h : nadolol: 10-24 h; bendroflumethiazide: 3 h |
| Long-Acting | ||
| methyclothiazide | Hypertension/edema: A: PO: 2.5-10 mg/d; max: 5 mg/d for hypertension; 10 mg/d for edema | For hypertension and edema associated with HF and renal or liver dysfunction. Side effects and drug interactions similar to those of HCTZ. Long duration of action. Pregnancy category: B; PB: UK;  : UK : UK |
| Thiazide-Like Diuretics | ||
| chlorthalidone (Hygroton, Thalitone) | Hypertension: A: PO: 12.5-50 mg/d; 50 mg/d C: PO: 2 mg/kg/d Edema: A: PO: 25-100 mg/d; max: 200 mg/d | For hypertension and edema associated with HF and renal or liver dysfunction. Very long duration of action (24-72 h). Pregnancy category: B; PB: 75%;  : 40-60 h : 40-60 h |
| indapamide | Hypertension/edema: A: PO: 1.25-2.5 mg/d; may increase to 5 mg/d; max: 5 mg/d | For hypertension and edema. Long-acting diuretic. May be classified as loop diuretic. Pregnancy category: B; PB: 71%-79%;  : 14-18 h : 14-18 h |
| metolazone (Zaroxolyn) | Hypertension: A: PO: 2.5-5.0 mg/d C: PO: 0.2-0.4 mg/kg/d in divided doses Edema: A: PO: 5-20 mg/d | For hypertension and edema. Intermediate-acting diuretic. More effective than thiazides in patients with decreased renal function. Pregnancy category: B; PB: 33%;  : 14 h : 14 h |
Thiazide diuretics are used primarily for patients with normal renal function. If the patient has a renal disorder and creatinine clearance is less than 30 mL/min, the effectiveness of the thiazide diuretic is greatly decreased. Thiazides cause a loss of sodium, potassium, and magnesium, but they promote calcium reabsorption. Hypercalcemia (calcium excess) may result, and the condition can be hazardous to the patient who is digitalized or has cancer that causes hypercalcemia. Thiazides affect glucose tolerance, so hyperglycemia can also occur. Thiazides should be used cautiously in patients with diabetes mellitus. Laboratory test results (e.g., electrolytes, glucose) need to be monitored.
The thiazide drug hydrochlorothiazide has been combined with selected angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, alpha-blockers, angiotensin II blockers, and centrally acting sympatholytics to control hypertension. Prototype Drug Chart 43-1 outlines the pharmacologic data for hydrochlorothiazide.
Pharmacokinetics
Thiazides are well absorbed from the gastrointestinal (GI) tract. Hydrochlorothiazide has moderate protein-binding power. The half-life of the thiazide drugs is longer than that of the loop diuretics. For this reason, thiazides should be administered in the morning to avoid nocturia (nighttime urination) and sleep interruption.
Pharmacodynamics
Thiazides act directly on arterioles to cause vasodilation, which can lower blood pressure. Other action includes the promotion of sodium chloride and water excretion, resulting in a decrease in vascular fluid volume and a concomitant decrease in cardiac output and blood pressure. The onset of action of hydrochlorothiazide occurs within 2 hours. Peak concentration times are long (3 to 6 hours). Thiazides are divided into three groups, according to their duration of action: short-acting (duration less than 12 hours), intermediate-acting (duration 12 to 24 hours), and long-acting (duration more than 24 hours).
Side Effects and Adverse Reactions.
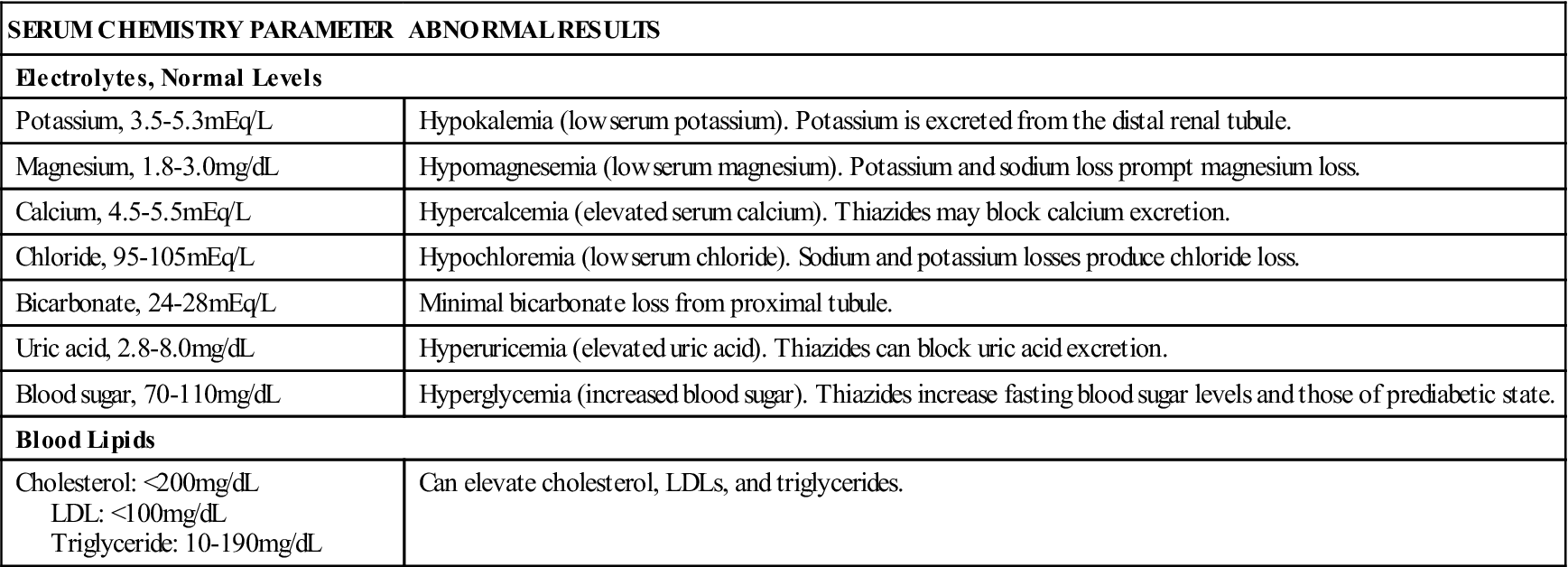
Side effects and adverse reactions of thiazides include electrolyte imbalances (hypokalemia, hypercalcemia, hypomagnesemia, and bicarbonate loss), hyperglycemia (elevated blood sugar), hyperuricemia (elevated serum uric acid level), and hyperlipidemia (elevated blood lipid level). Signs and symptoms of hypokalemia should be assessed, and serum potassium levels must be closely monitored. Potassium supplements are frequently needed. Serum calcium and uric acid levels should be checked, because thiazides block calcium and uric acid excretion. Thiazides affect the metabolism of carbohydrates, and hyperglycemia can result, especially in patients with high to high-normal blood sugar levels. Thiazides can increase serum cholesterol, low-density lipoprotein, and triglyceride levels. A drug may be ordered to lower blood lipids. Other side effects include dizziness, headache, nausea, vomiting, constipation, urticaria, or hives (rare), and blood dyscrasias (rare). Table 43-2 summarizes the serum chemistry abnormalities that can occur with thiazide use.
TABLE 43-2
SERUM CHEMISTRY ABNORMALITIES ASSOCIATED WITH THIAZIDES
| SERUM CHEMISTRY PARAMETER | ABNORMAL RESULTS |
| Electrolytes, Normal Levels | |
| Potassium, 3.5-5.3 mEq/L | Hypokalemia (low serum potassium). Potassium is excreted from the distal renal tubule. |
| Magnesium, 1.8-3.0 mg/dL | Hypomagnesemia (low serum magnesium). Potassium and sodium loss prompt magnesium loss. |
| Calcium, 4.5-5.5 mEq/L | Hypercalcemia (elevated serum calcium). Thiazides may block calcium excretion. |
| Chloride, 95-105 mEq/L | Hypochloremia (low serum chloride). Sodium and potassium losses produce chloride loss. |
| Bicarbonate, 24-28 mEq/L | Minimal bicarbonate loss from proximal tubule. |
| Uric acid, 2.8-8.0 mg/dL | Hyperuricemia (elevated uric acid). Thiazides can block uric acid excretion. |
| Blood sugar, 70-110 mg/dL | Hyperglycemia (increased blood sugar). Thiazides increase fasting blood sugar levels and those of prediabetic state. |
| Blood Lipids | |
| Cholesterol: <200 mg/dL LDL: <100 mg/dL Triglyceride: 10-190 mg/dL | Can elevate cholesterol, LDLs, and triglycerides. |
Contraindications.
Thiazides are contraindicated for use in renal failure. Symptoms of severe kidney impairment or shutdown include oliguria (marked decrease in urine output), elevated blood urea nitrogen (BUN), and elevated serum creatinine.
Drug Interactions.
Of the numerous thiazide drug interactions, the most serious occurs with digoxin. Thiazides can cause hypokalemia, which enhances the action of digoxin, and digitalis toxicity can occur. Potassium supplements are frequently prescribed, and serum potassium levels are monitored. Thiazides also induce hypercalcemia, which enhances the action of digoxin, resulting in possible digitalis toxicity. Signs and symptoms of digitalis toxicity (bradycardia, nausea, vomiting, visual changes) should be reported. Thiazides enhance the action of lithium, and lithium toxicity can occur. Thiazides potentiate the action of other antihypertensive drugs, which may be used to advantage in combination drug therapy for hypertension.
Loop (High Ceiling) Diuretics
The loop, or high-ceiling, diuretics act on the thick ascending loop of Henle to inhibit chloride transport of sodium into the circulation (inhibit passive reabsorption of sodium). Sodium and water are lost, together with potassium, calcium, and magnesium. Loop diuretics can affect blood sugar and increase uric acid levels. Drugs in this group are extremely potent and cause marked depletion of water and electrolytes. This high diuretic potential is the reason they are often called high-ceiling diuretics or potassium-wasting diuretics. The effects of loop diuretics are dose-related (i.e., increasing the dose increases the effect and response of the drug). More potent than thiazides for promoting diuresis (inhibiting reabsorption of sodium two to three times more effectively), loop diuretics are less effective as antihypertensive agents.
Loop diuretics should not be prescribed if a thiazide could alleviate body fluid excess. If furosemide (Lasix) alone is not effective in removing body fluid, a thiazide may be added, but furosemide should never be combined with another loop diuretic. Furosemide is usually administered as an oral dose in the morning or intravenously when the patient’s condition warrants immediate removal of body fluid, for example, in cases of acute heart failure or pulmonary edema.
 , half-life; UK, unknown; wk, week; y, year; >, greater than; <, less than.
, half-life; UK, unknown; wk, week; y, year; >, greater than; <, less than. : 6-15 h
: 6-15 h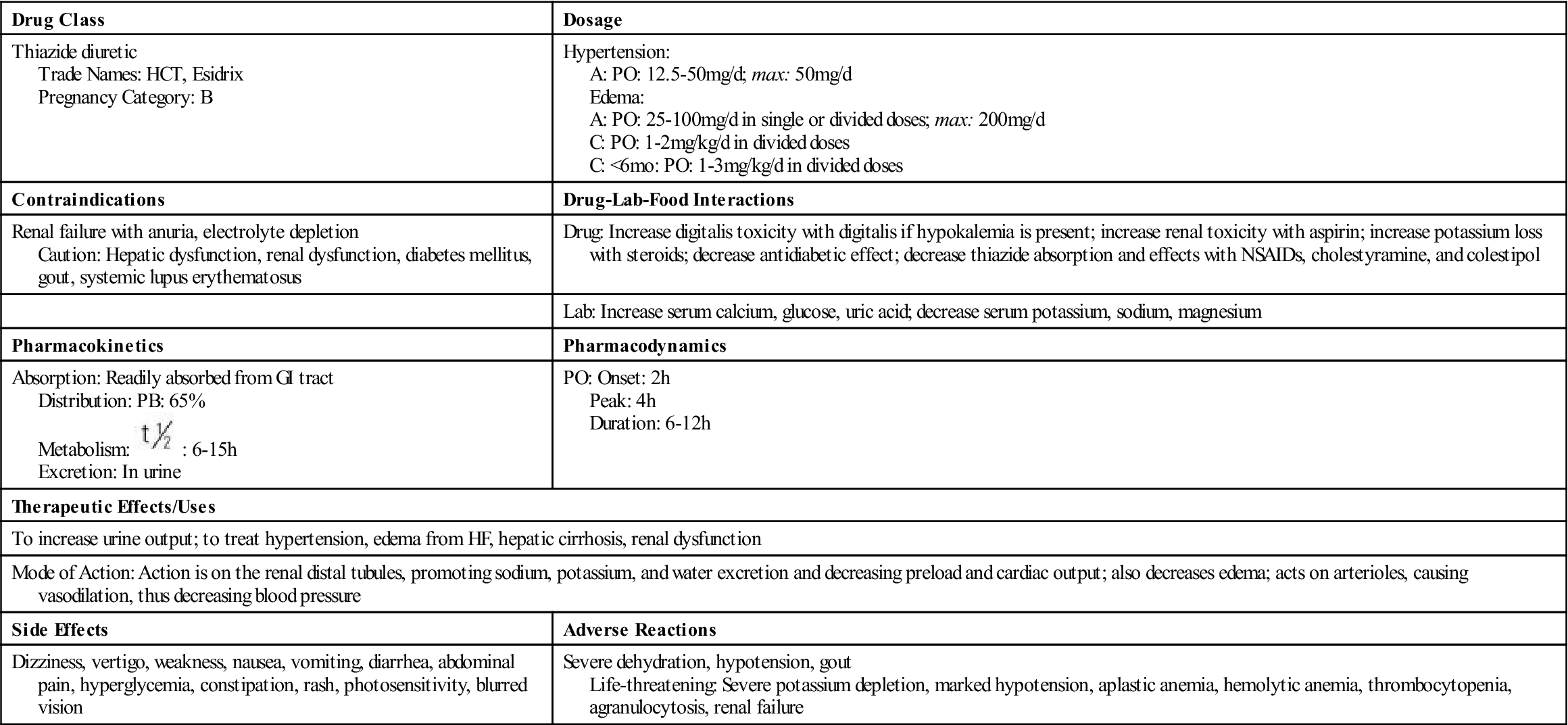
 , half-life.
, half-life.











