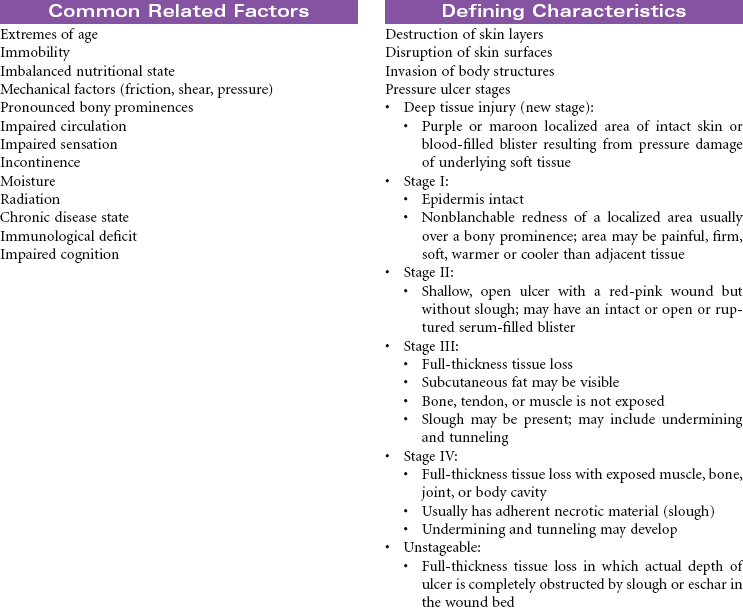
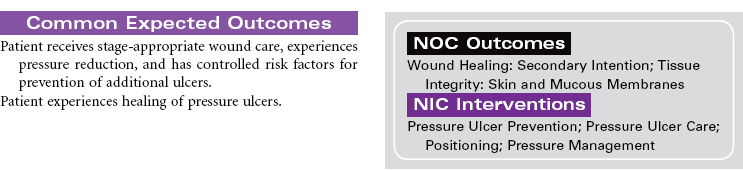
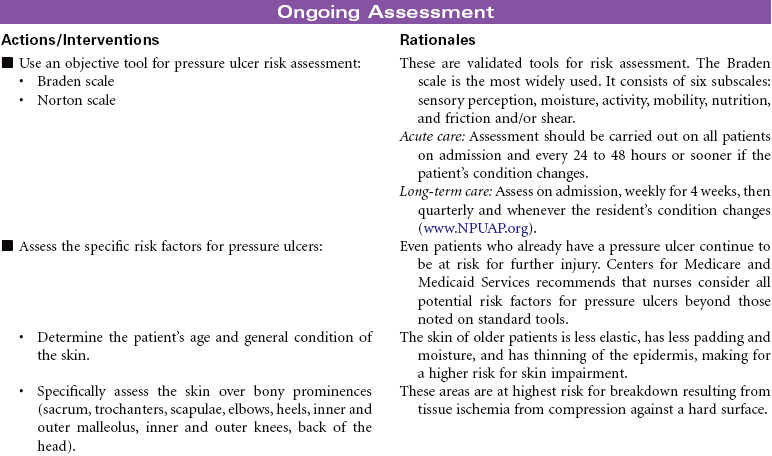
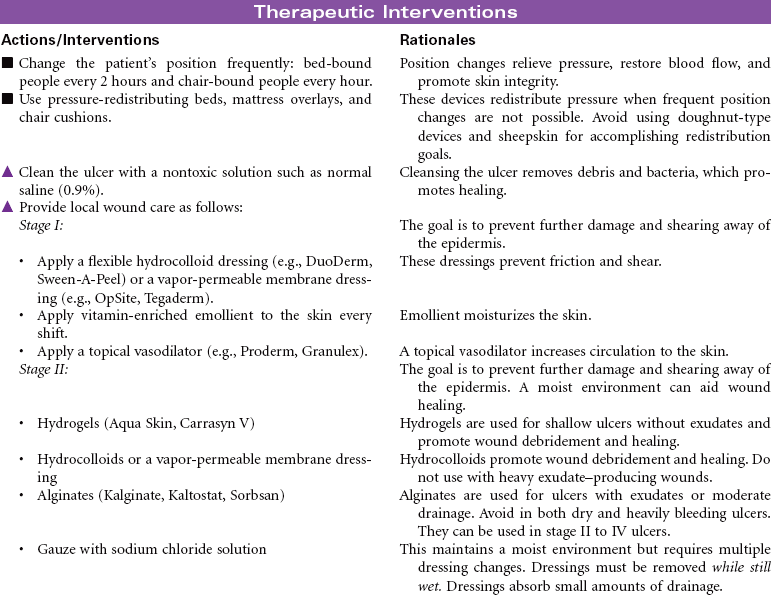
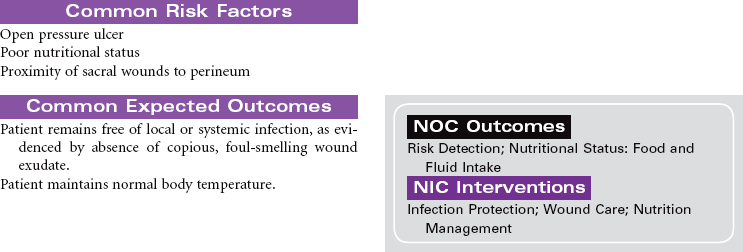
Chapter 15 Pressure Sores; Decubitus Ulcers; Bedsores Pressure ulcers are a major health problem. Nurses play a key role in prevention and successful treatment. The National Pressure Ulcer Advisory Panel defines pressure ulcer as “a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure or pressure in combination with shear and/or friction.” Prolonged pressure occurs when tissue is between a bony prominence and a hard surface such as a mattress. The pressure compresses small blood vessels and leads to ineffective tissue perfusion. Loss of perfusion causes tissue hypoxia and eventually cellular death. In addition to prolonged pressure, friction and shearing force contribute to the development of pressure ulcers. These forces are present when a patient slides down in bed and is pulled up against the surface of the mattress. Pressure ulcers are usually staged to classify the degree of tissue damage observed.* Pressure ulcers stage I through III can heal with aggressive local wound treatment and proper nutritional support; stage IV pressure ulcers often require surgical intervention (e.g., flap closure, plastic surgery). Pressure ulcers affect persons, regardless of age, who are immobile, are malnourished, or have contributing conditions (e.g., incontinence, decreased level of consciousness). Wound care remains a challenge for nurses and the health care team. More research in wound healing is needed. This care plan is based on recommendations from the National Pressure Ulcer Advisory Panel, the National Guideline Clearinghouse, and the Agency for Healthcare Research and Quality Pressure Ulcer Prevention Guidelines. This care plan addresses care issues in hospital, long-term care, or home settings.
Integumentary Care Plans
Pressure Ulcers (Impaired Skin Integrity)
Integumentary Care Plans
Get Clinical Tree app for offline access