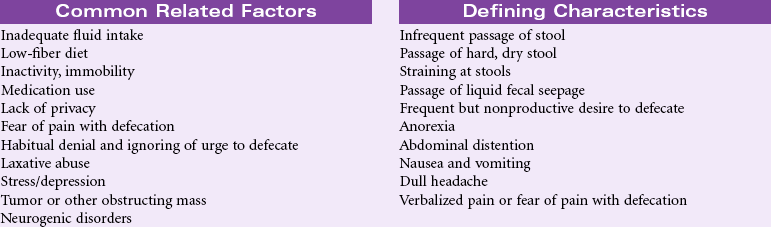
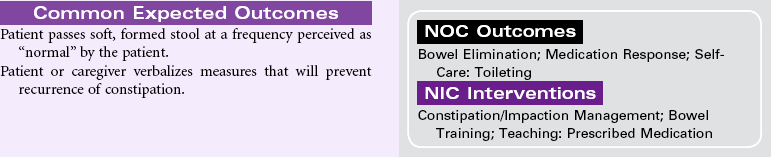
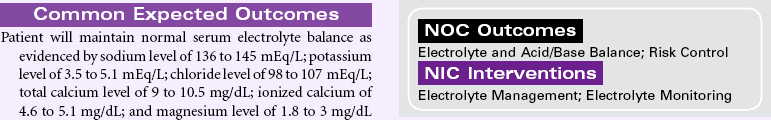
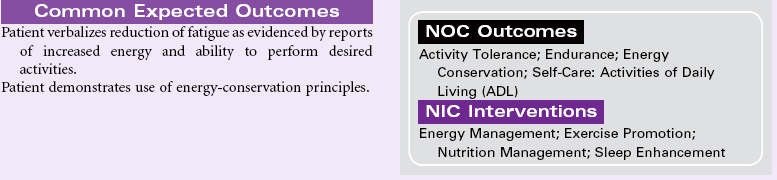
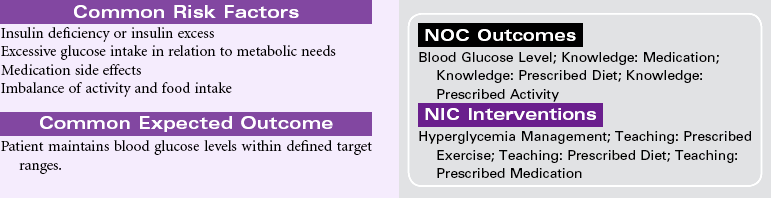
Chapter 2 For additional care plans and an Online Care Plan Constructor, go to Definition: Risk for variation of blood glucose/sugar levels from the normal range Definition: Change in normal bowel habits characterized by involuntary passage of stool Definition: Inspiration and/or expiration that does not provide adequate ventilation Definition: Inadequate blood pumped by the heart to meet the metabolic demands of the body Definition: At risk for change in serum electrolyte levels that may compromise health
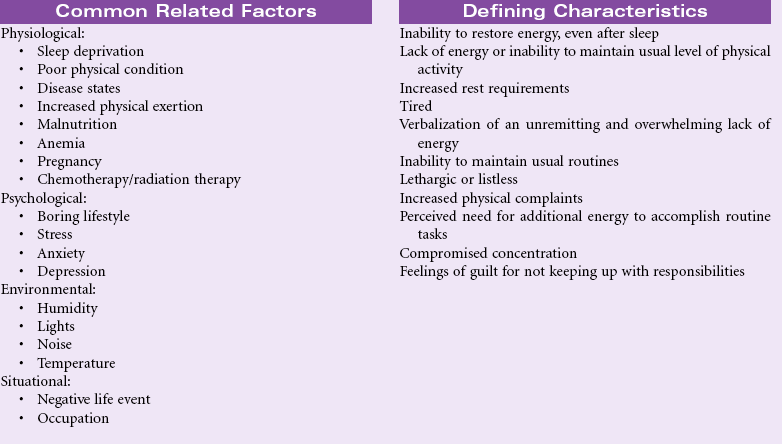
Nursing Diagnosis Care Plans
![]() at http://evolve.elsevier.com/Gulanick
at http://evolve.elsevier.com/Gulanick
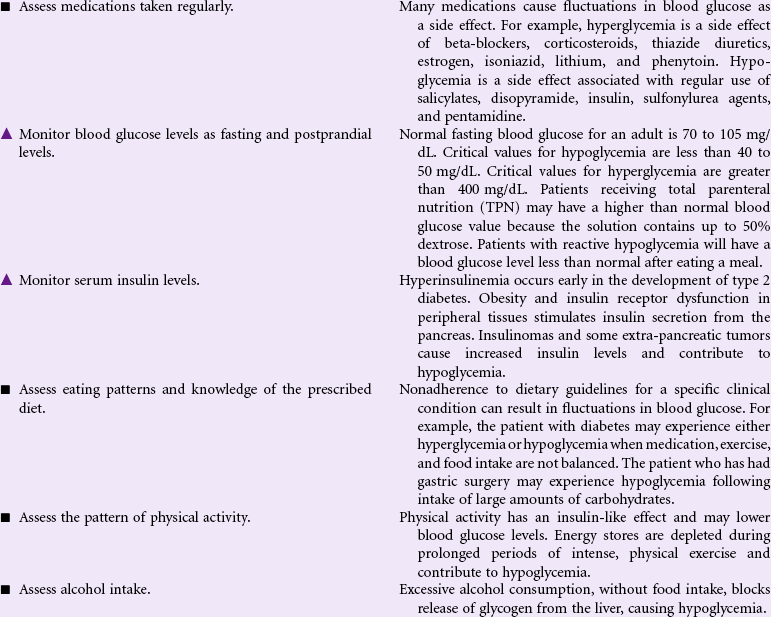
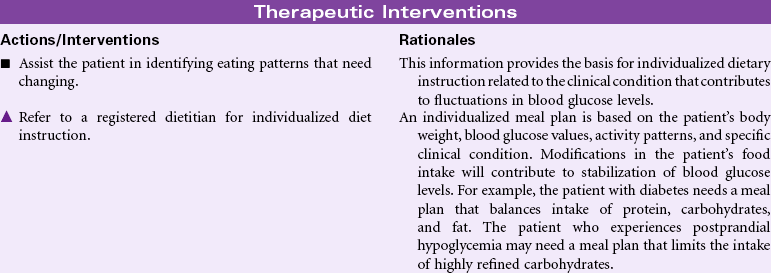
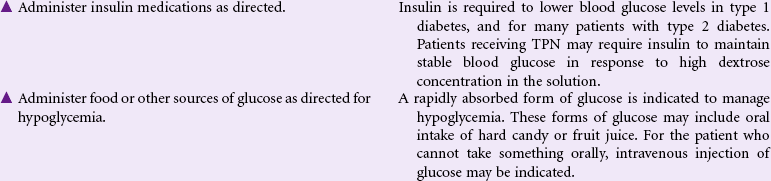
![]() Risk for Unstable Blood Glucose Level
Risk for Unstable Blood Glucose Level
![]() Bowel Incontinence
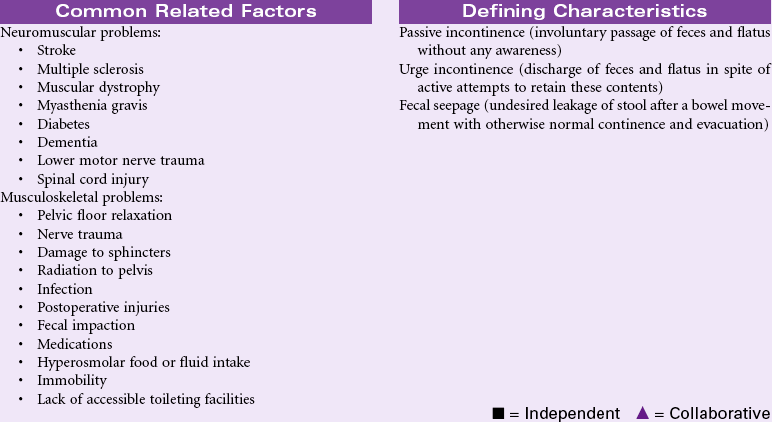
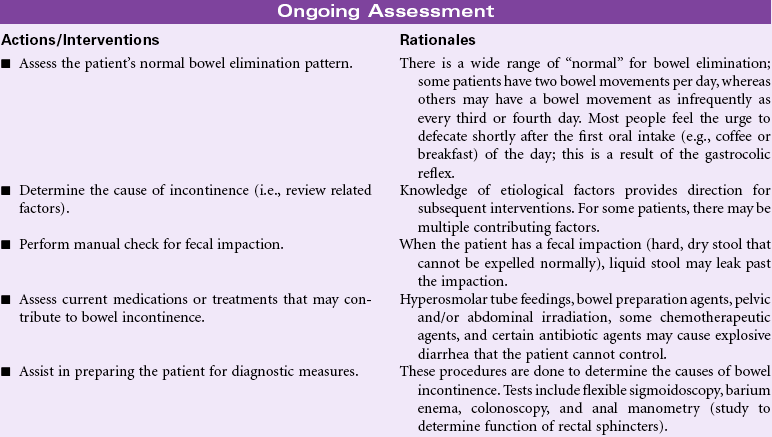
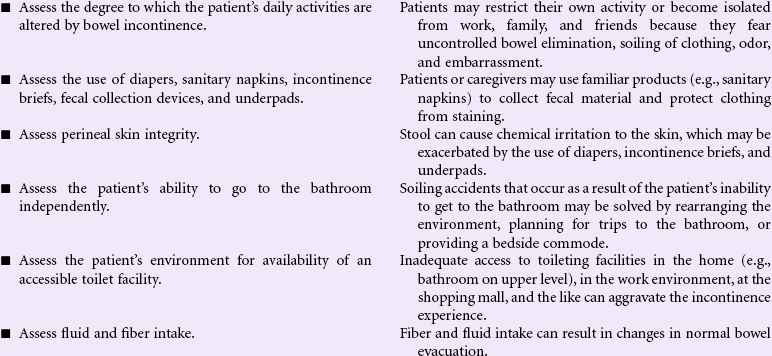
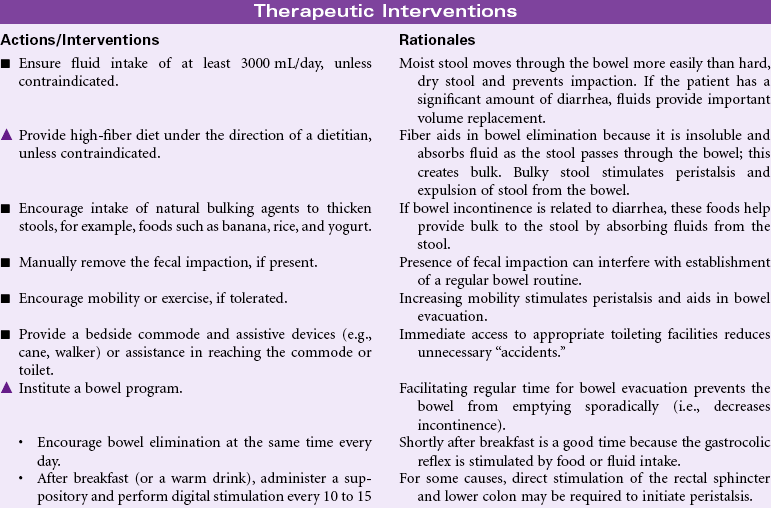
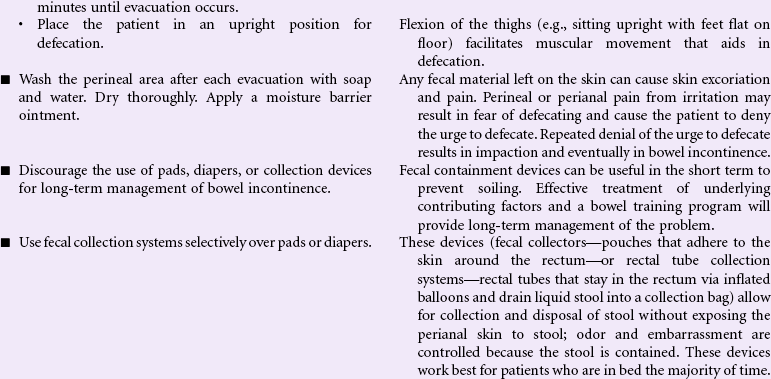
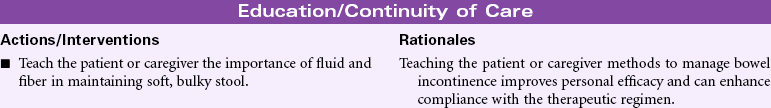
Bowel Incontinence
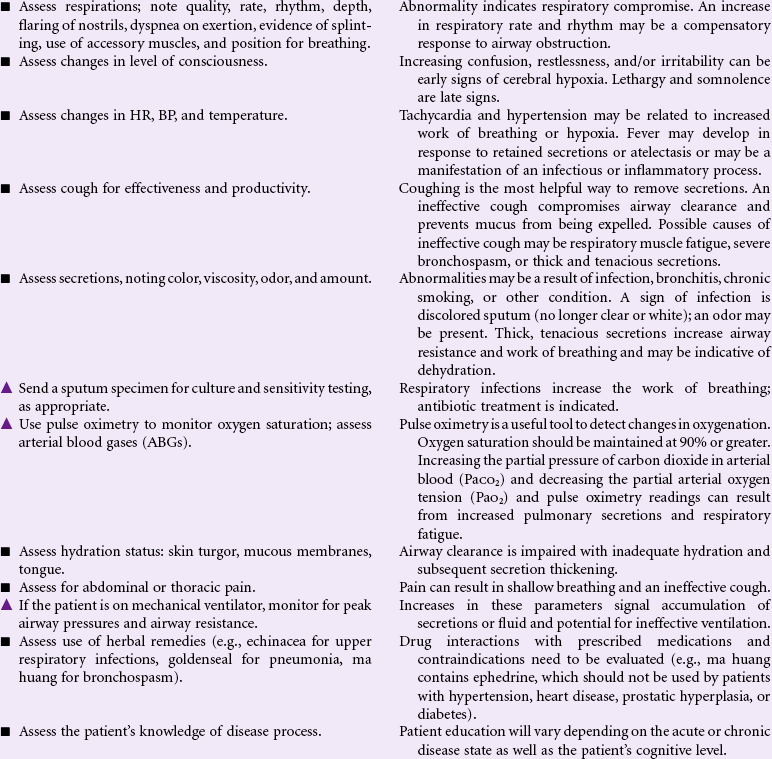
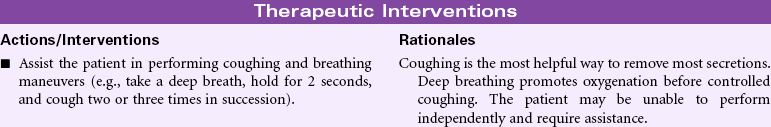
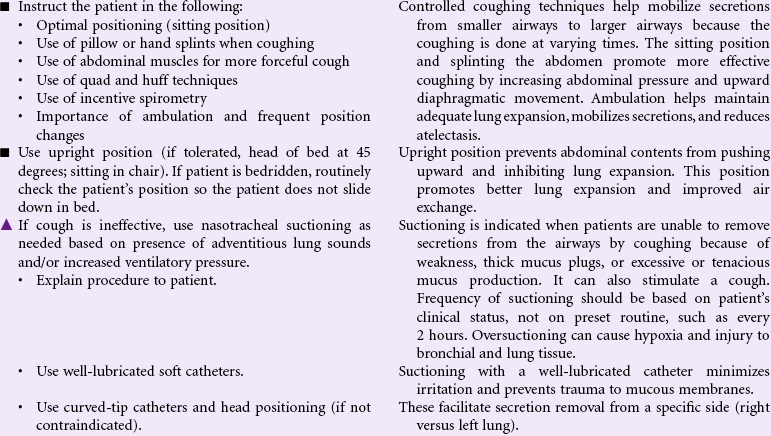
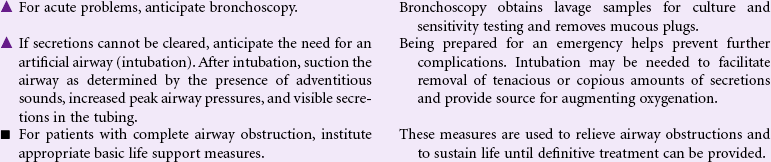
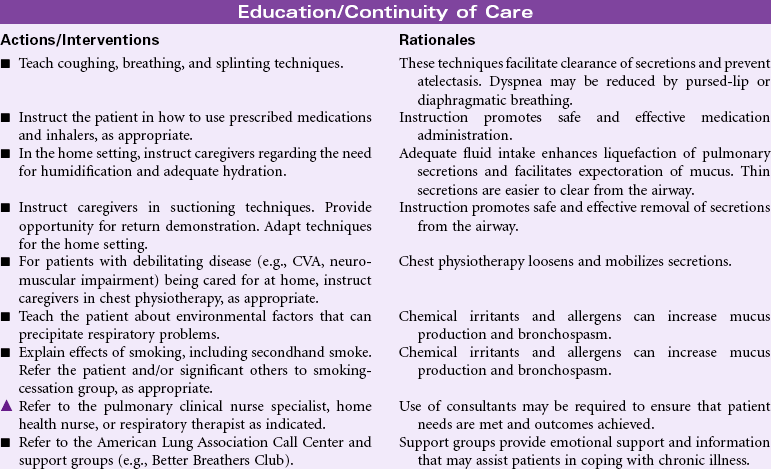
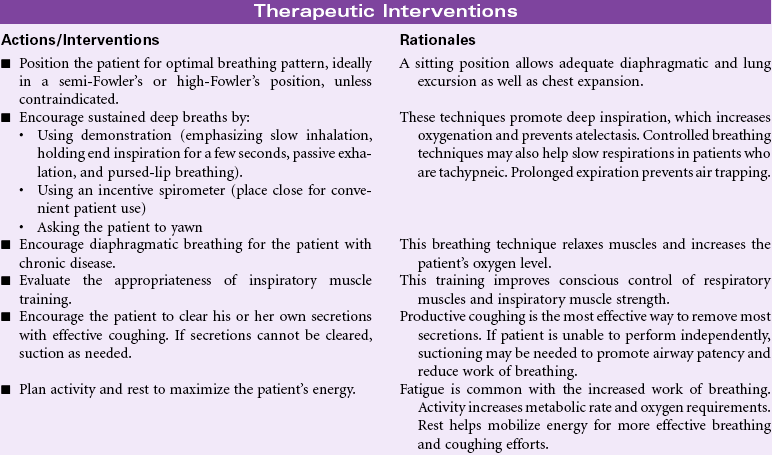
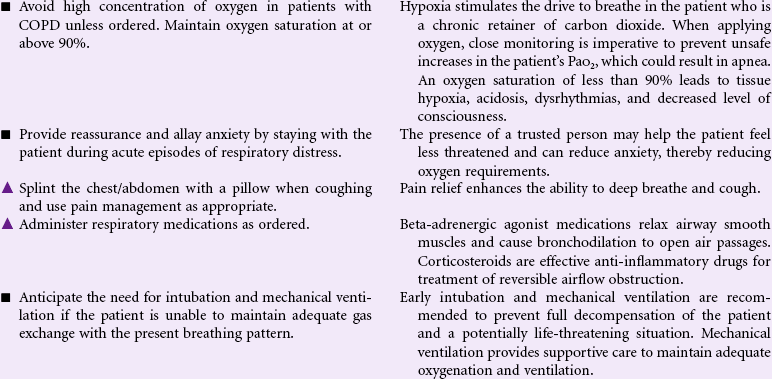
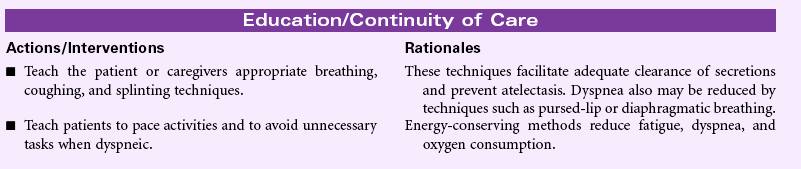
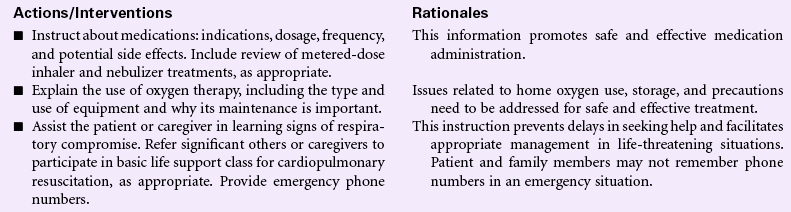
![]() Ineffective Breathing Pattern
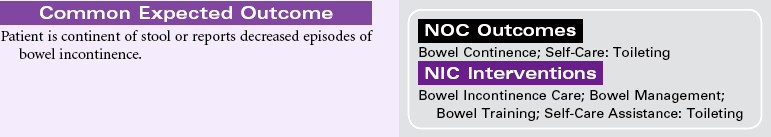
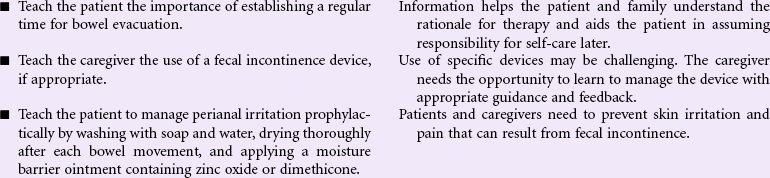
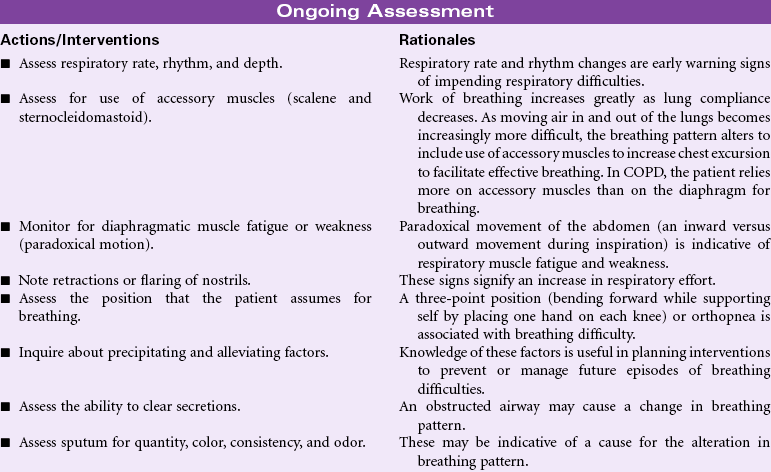
Ineffective Breathing Pattern
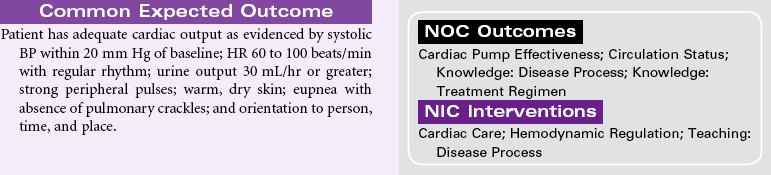
![]() Decreased Cardiac Output
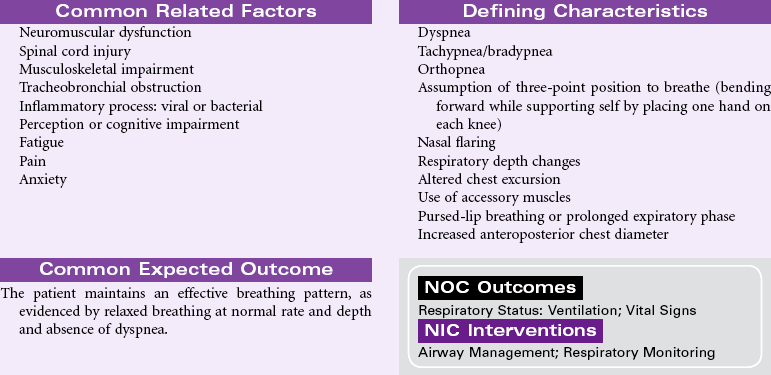
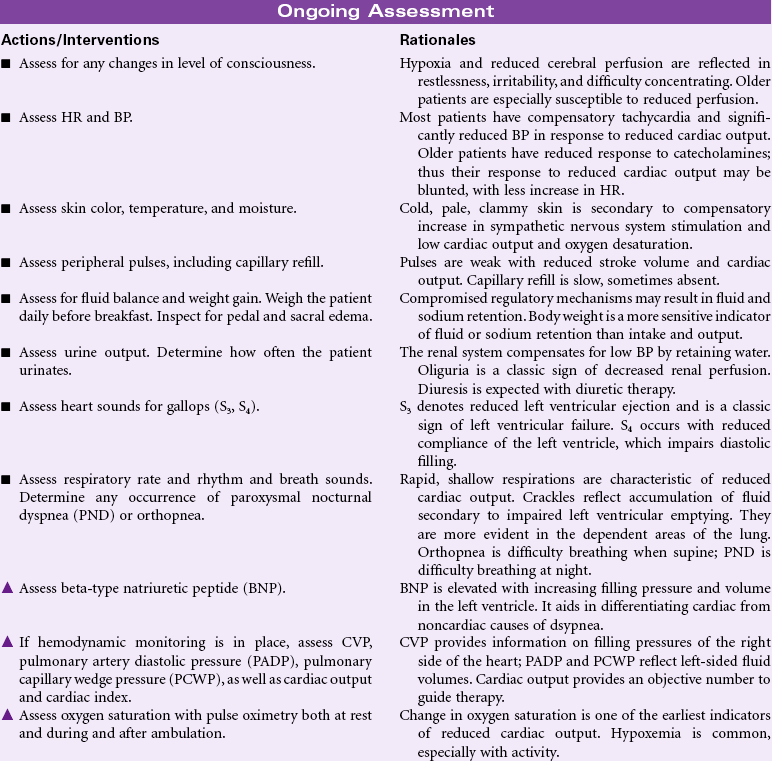
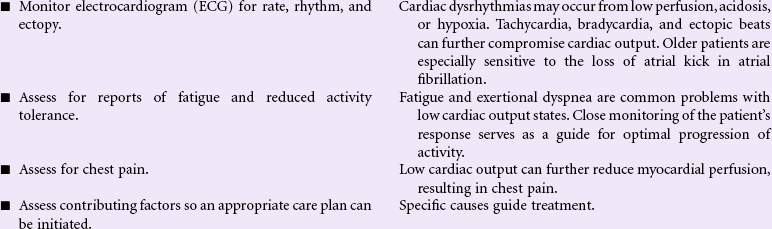
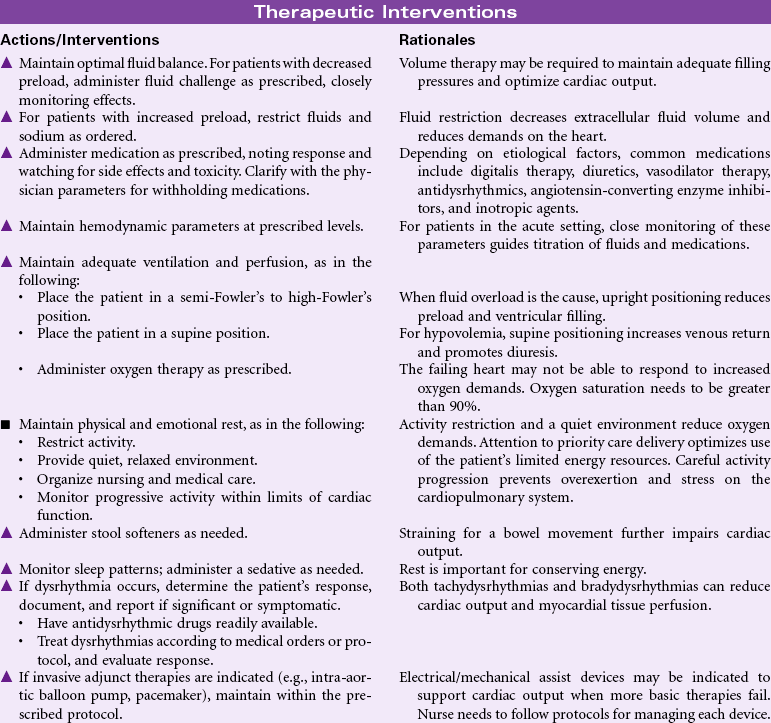
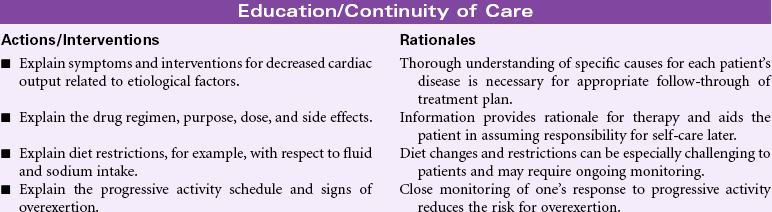
Decreased Cardiac Output
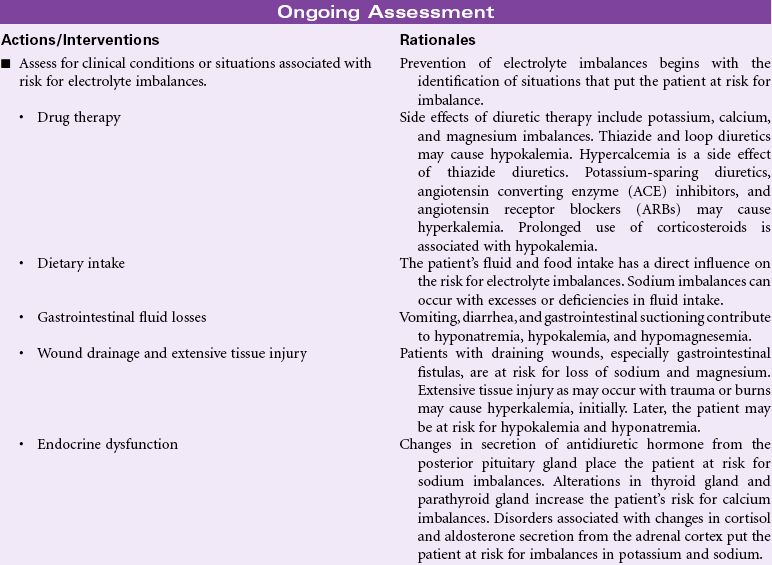
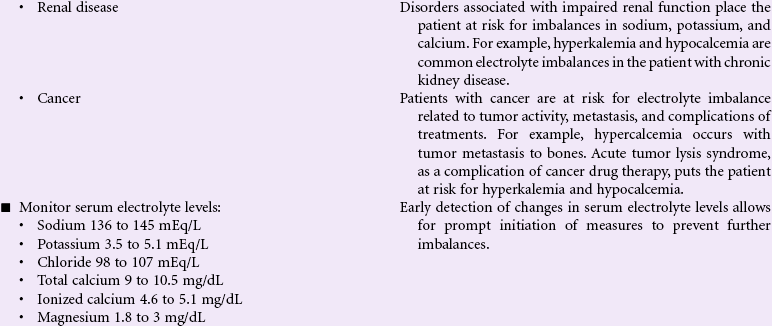
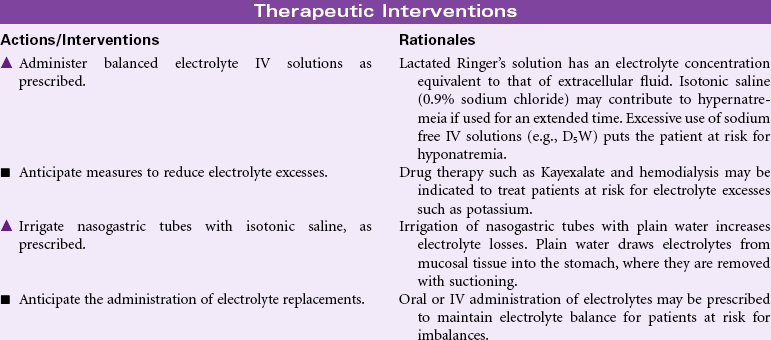
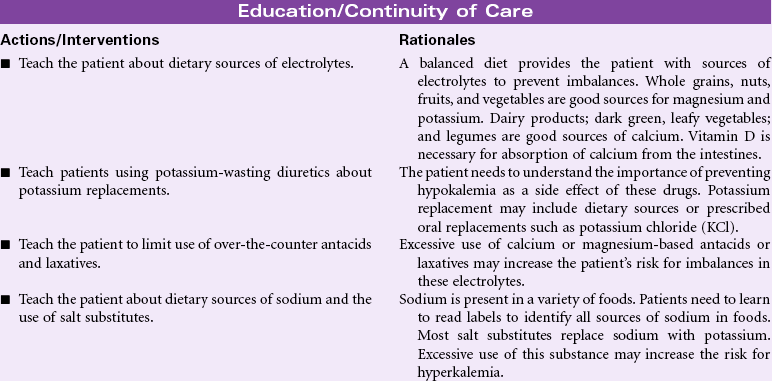
![]() Risk for Electrolyte Imbalance
Risk for Electrolyte Imbalance
Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access