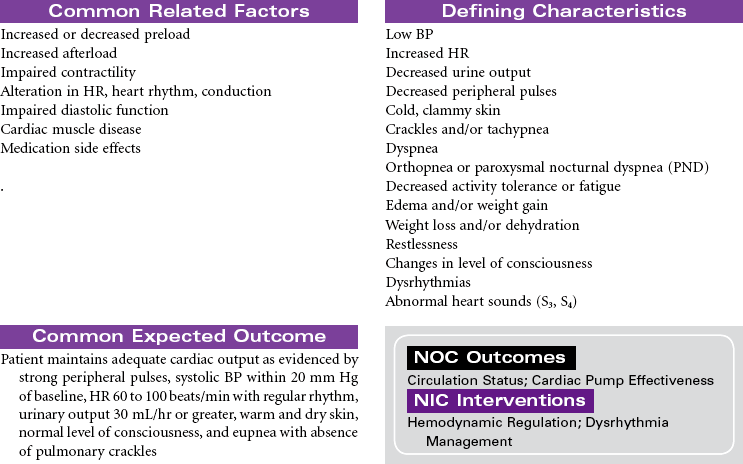
Chapter 5
Cardiac and Vascular Care Plans
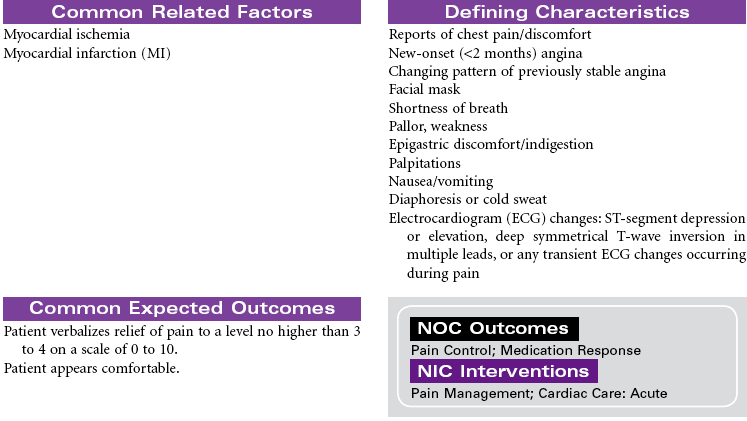
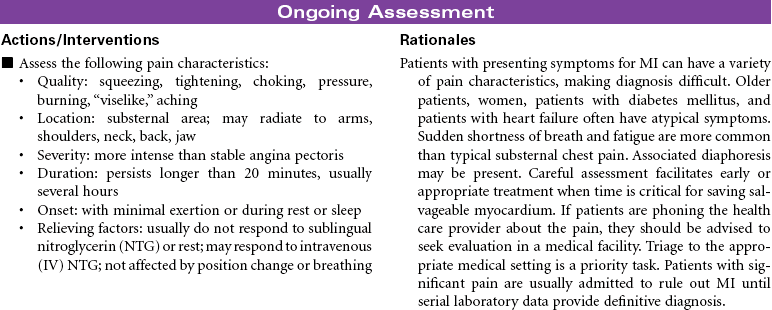
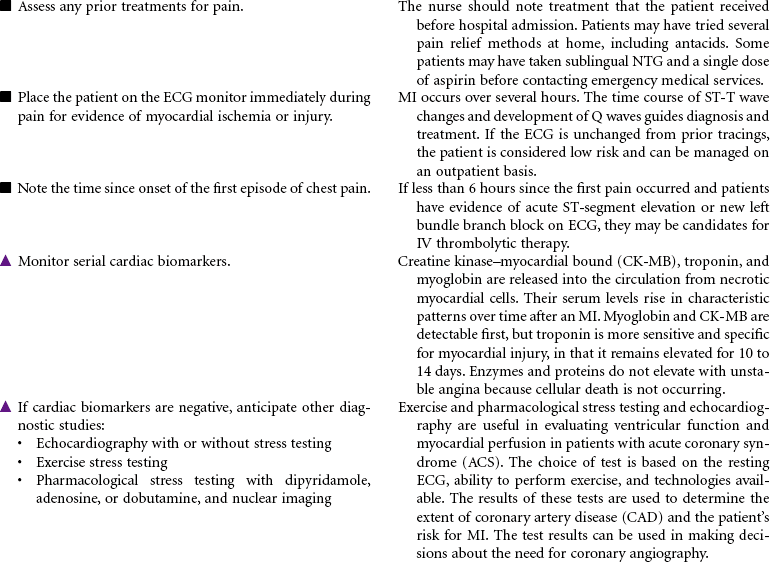
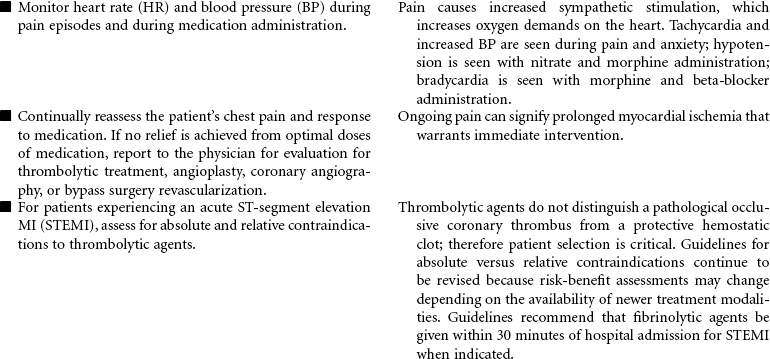
Acute Coronary Syndromes/Myocardial Infarction
![]() For additional care plans and an Online Care Plan Constructor, go to http://evolve.elsevier.com/Gulanick/.
For additional care plans and an Online Care Plan Constructor, go to http://evolve.elsevier.com/Gulanick/.
Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access

 = Independent
= Independent  = Collaborative
= Collaborative