Chapter 11 Acute Tubular Necrosis (ATN); Renal Insufficiency; Acute Kidney Injury Internal Arteriovenous Fistula; Graft; Central Venous Catheter; Renal Replacement Therapy
Renal and Urinary Tract Care Plans
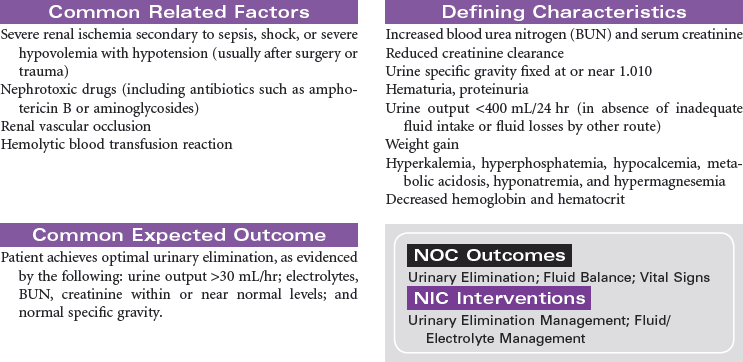
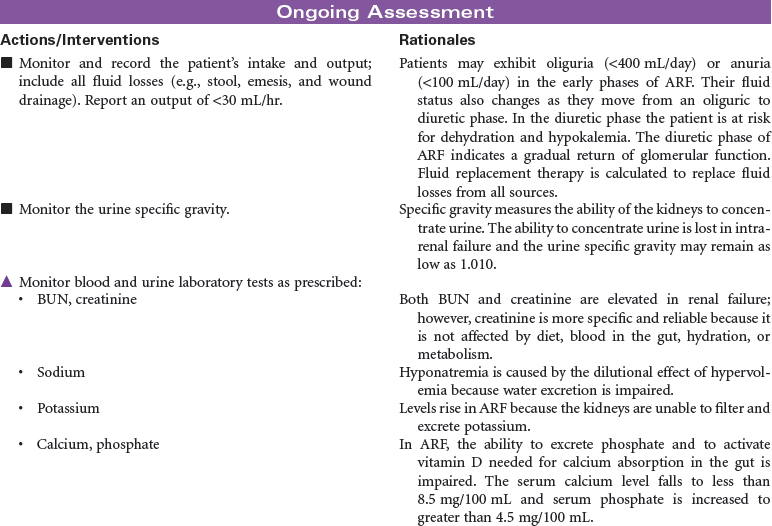
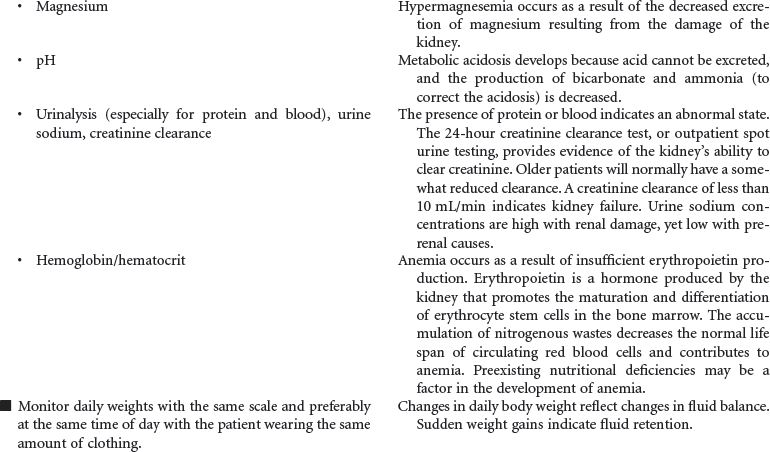
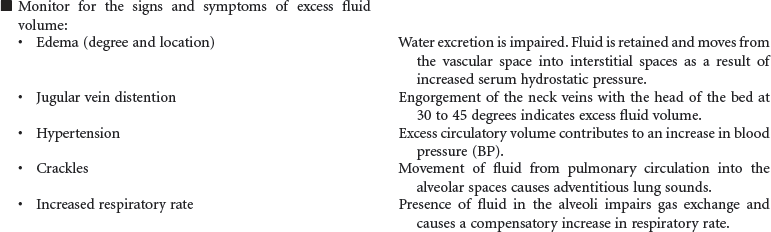
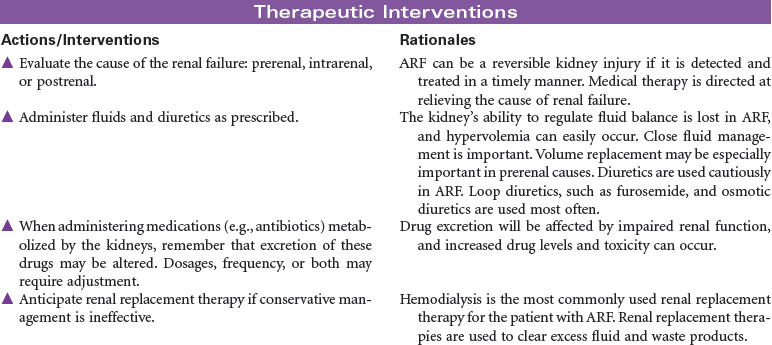
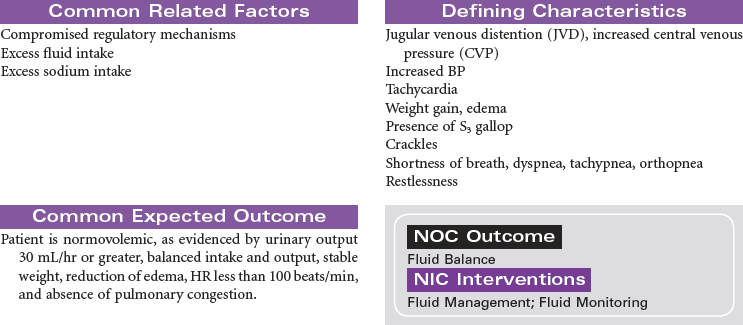
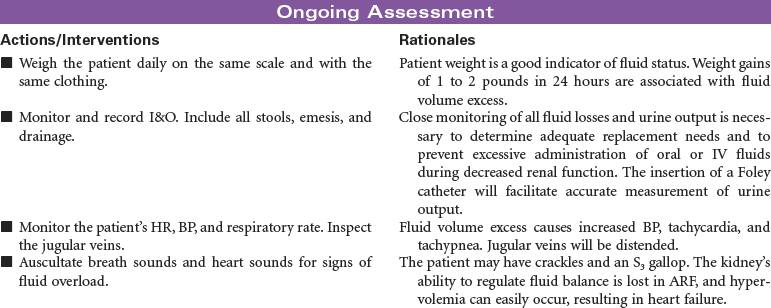
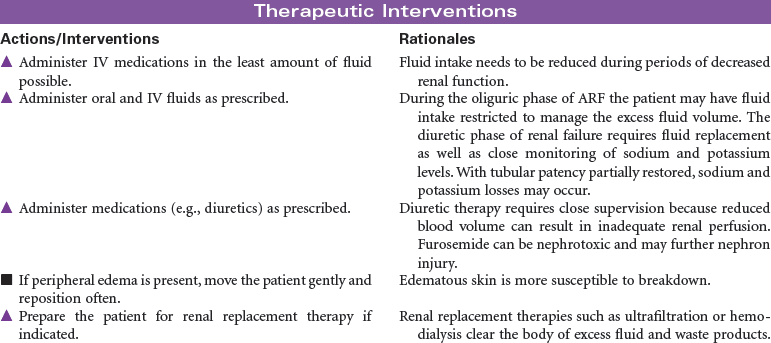
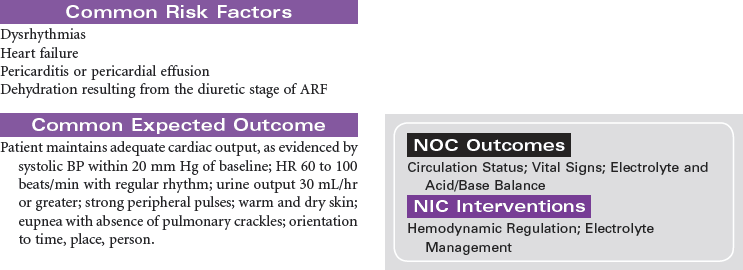
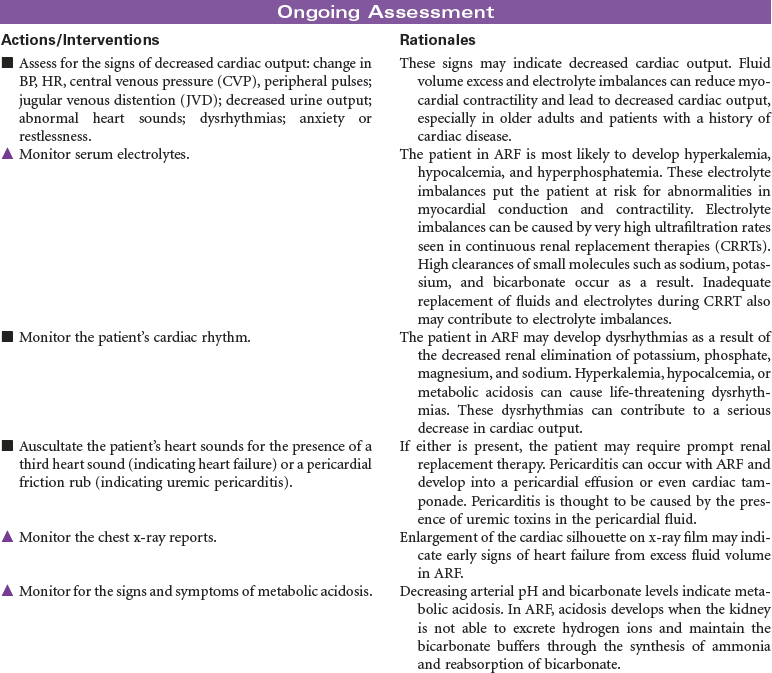
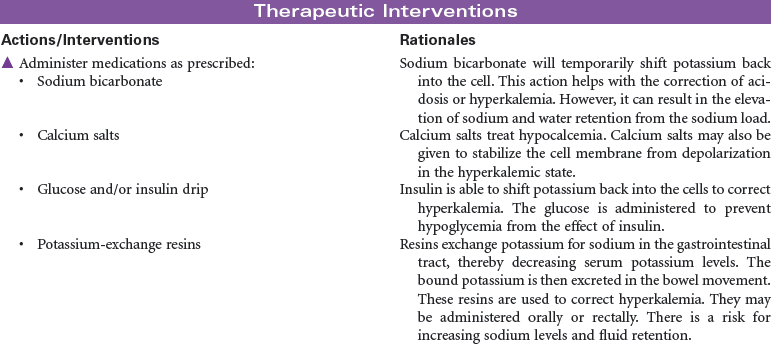
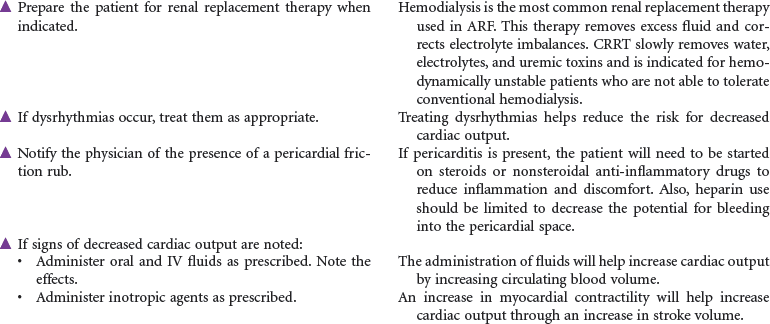
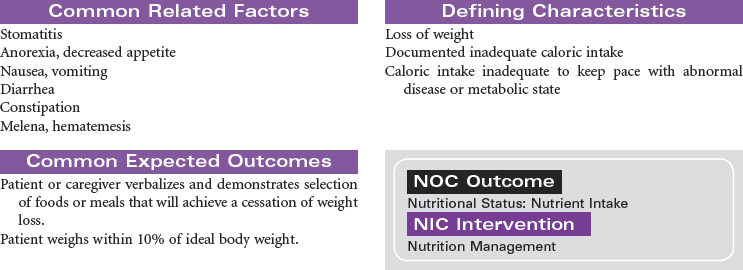
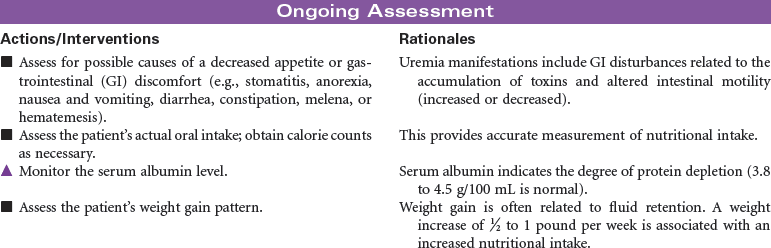
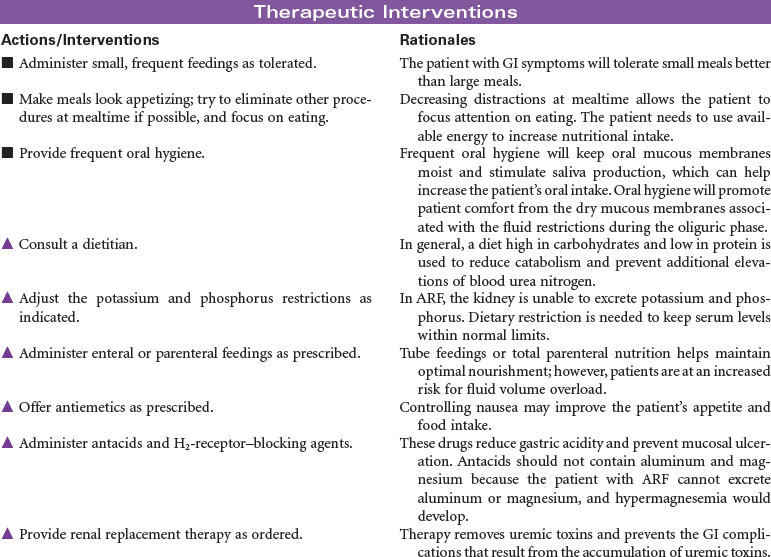
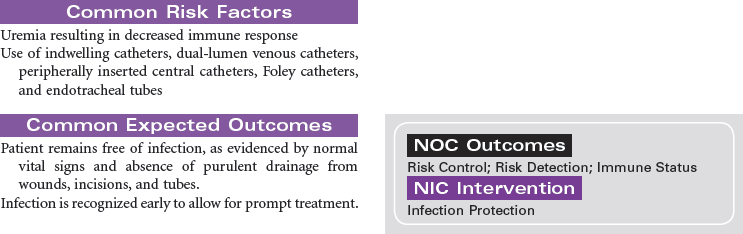
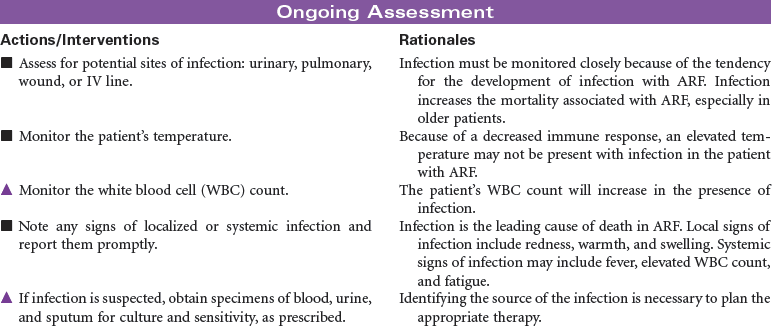
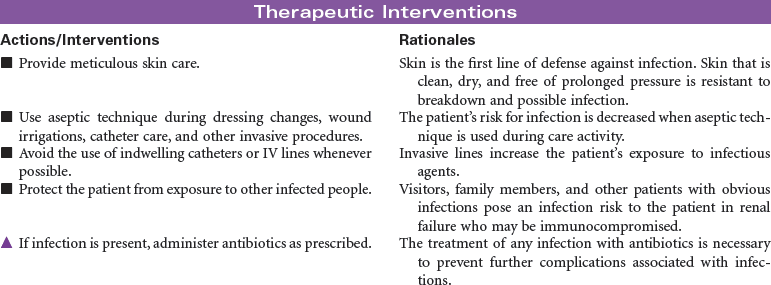
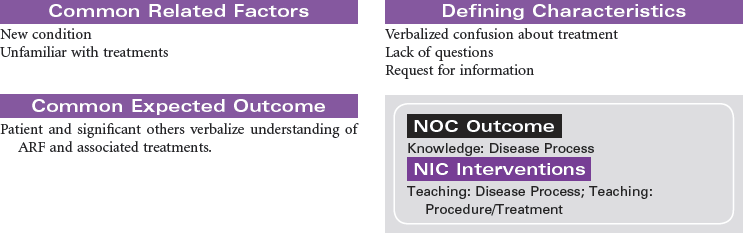
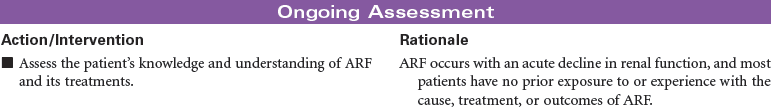
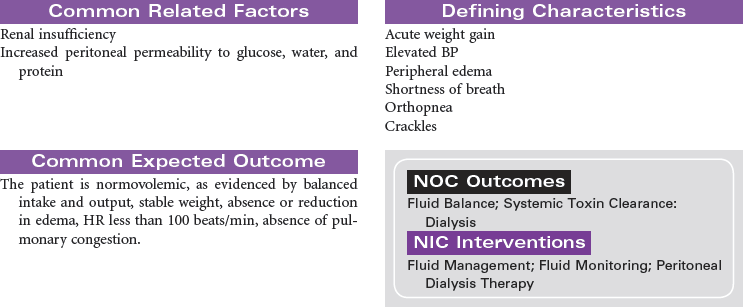
Acute Renal Failure
![]() For additional care plans, go to http://evolve.elsevier.com/Gulanick/.
For additional care plans, go to http://evolve.elsevier.com/Gulanick/.
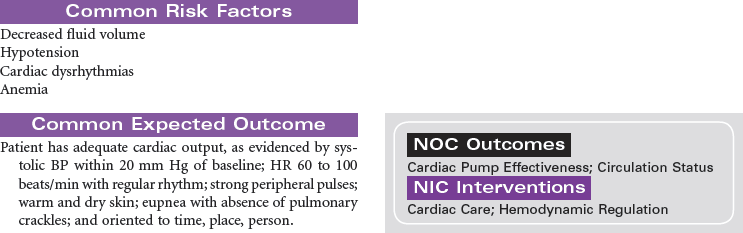
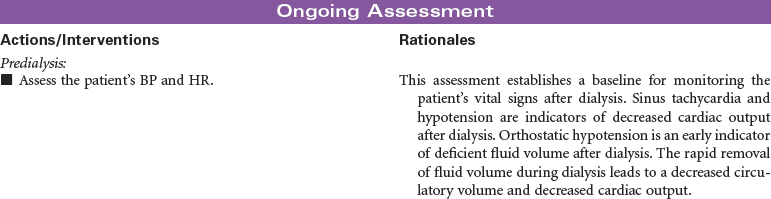
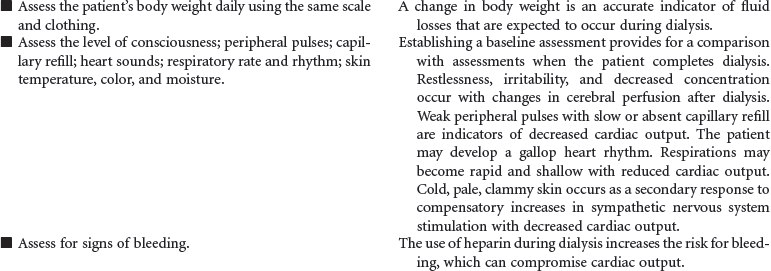
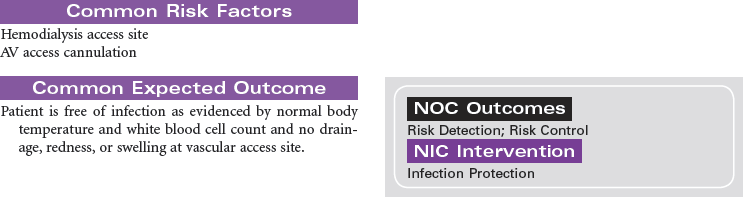
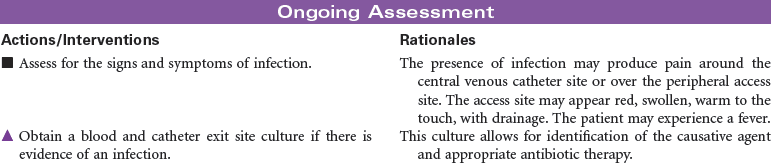
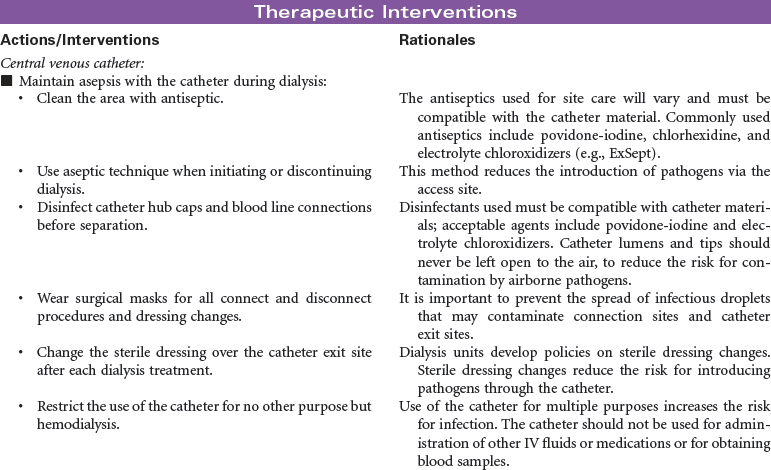
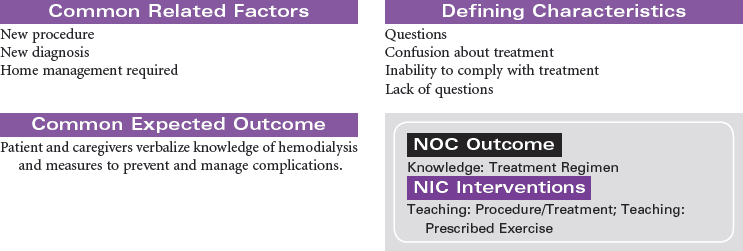
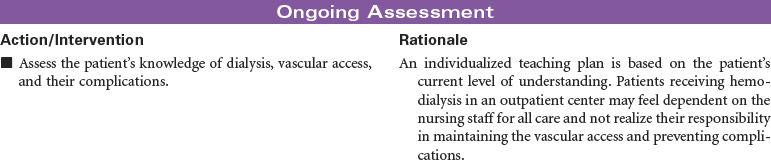
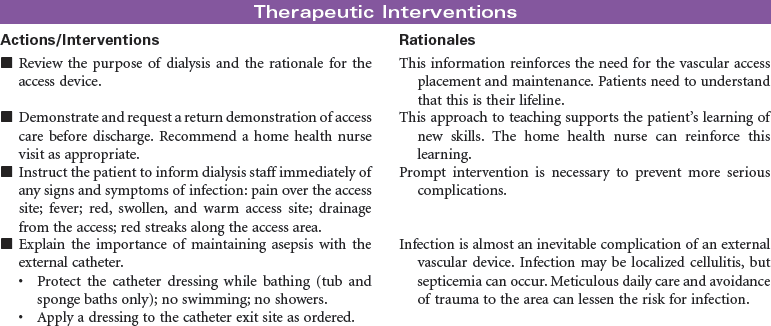
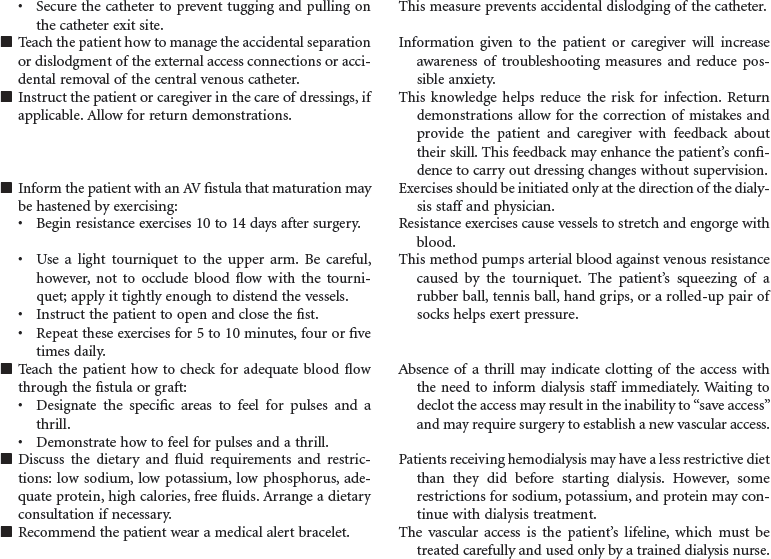
Hemodialysis
Renal and Urinary Tract Care Plans
Get Clinical Tree app for offline access

 = Independent
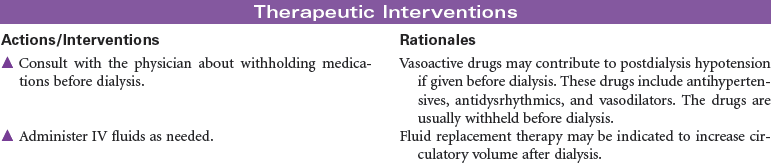
= Independent  = Collaborative
= Collaborative