Drugs for Lower Respiratory Disorders
Objectives
• Compare chronic obstructive pulmonary disease (COPD) and restrictive lung disease.
• Differentiate the drug groups used to treat COPD and asthma and the desired effects of each.
• Compare the side effects of beta2-adrenergic agonists and methylxanthines.
• Describe the therapeutic serum or plasma theophylline level and the toxic level.
Key Terms
asthma, p. 584
bronchial asthma, p. 585
bronchiectasis, p. 584
bronchodilators, p. 584
bronchospasm, p. 585
chronic bronchitis, p. 584
chronic obstructive pulmonary disease, p. 584
emphysema, p. 584
glucocorticoids, p. 595
mucolytics, p. 597
restrictive lung disease, p. 584
![]() http://evolve.elsevier.com/KeeHayes/pharmacology/
http://evolve.elsevier.com/KeeHayes/pharmacology/
Chronic obstructive pulmonary disease (COPD) and restrictive pulmonary disease are the two major categories of lower respiratory tract disorders. COPD is caused by airway obstruction with increased airway resistance of air flow to lung tissues. Four major pulmonary disorders cause COPD: chronic bronchitis, bronchiectasis, emphysema, and asthma. Chronic bronchitis, bronchiectasis, and emphysema frequently result in irreversible lung tissue damage. The lung tissue changes resulting from an acute asthmatic attack are normally reversible; however, if the attacks are frequent and asthma becomes chronic, irreversible changes in the lung tissue may result. Patients with COPD usually have a decrease in forced expiratory volume in 1 second (FEV1) as measured by pulmonary function tests.
Restrictive lung disease is a decrease in total lung capacity as a result of fluid accumulation or loss of elasticity of the lung. Pulmonary edema, pulmonary fibrosis, pneumonitis, lung tumors, thoracic deformities (scoliosis), and disorders affecting the thoracic muscular wall (e.g., myasthenia gravis) are among the types and causes of restrictive pulmonary disease.
Drugs discussed in this chapter are primarily used to treat COPD, particularly asthma. These drugs include bronchodilators (sympathomimetics [primarily beta2-adrenergic agonists], methylxanthines [xanthines]), leukotriene antagonists, glucocorticoids, cromolyn, anticholinergics, and mucolytics. Some of these drugs may also be used to treat restrictive pulmonary diseases.
Chronic Obstructive Pulmonary Disease
Asthma is an inflammatory disorder of the airway walls associated with a varying amount of airway obstruction. This disorder is triggered by stimuli such as stress, allergens, and pollutants. When activated by stimuli, the bronchial airways become inflamed and edematous, leading to constriction of air passages. Inflammation aggravates airway hyperresponsiveness to stimuli, causing bronchial cells to produce more mucous, which obstructs air passages. This obstruction contributes to wheezing, coughing, dyspnea (breathlessness), and tightness in the chest, particularly at night or in the early morning.
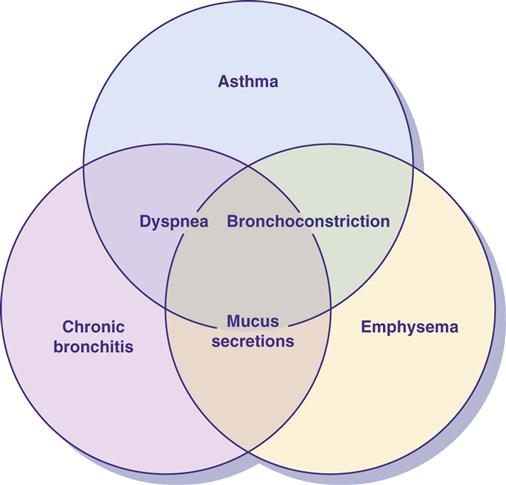
Bronchial asthma, one of the COPD lung diseases, is characterized by bronchospasm (constricted bronchioles), wheezing, mucus secretions, and dyspnea. There is resistance to air flow caused by obstruction of the airway. In acute and chronic asthma, minimal to no changes are seen in the structure and function of lung tissues when the disease process is in remission. In chronic bronchitis, emphysema, and bronchiectasis, there is permanent, irreversible damage to the physical structure of lung tissue. Symptoms are similar to those of asthma in these three pulmonary disorders, except wheezing does not occur. Figure 41-1 shows the overlapping symptoms of COPD conditions. Frequently, there is a steady deterioration over a period of years.
Chronic bronchitis is a progressive lung disease caused by smoking or chronic lung infections. Bronchial inflammation and excessive mucous secretion result in airway obstruction. Productive coughing is a response to excess mucus production and chronic bronchial irritation. Inspiratory and expiratory rhonchi may be heard on auscultation. Hypercapnia (increased carbon dioxide retention) and hypoxemia (decreased blood oxygen) lead to respiratory acidosis.
In bronchiectasis, there is abnormal dilation of the bronchi and bronchioles secondary to frequent infection and inflammation. The bronchioles become obstructed by the breakdown of the epithelium of the bronchial mucosa. Tissue fibrosis may result.
Emphysema is a progressive lung disease caused by cigarette smoking, atmospheric contaminants, or lack of the alpha1-antitrypsin protein that inhibits proteolytic enzymes that destroy alveoli (air sacs). Proteolytic enzymes are released in the lung by bacteria or phagocytic cells. The terminal bronchioles become plugged with mucus, causing a loss in the fiber and elastin network in the alveoli. Alveoli enlarge as many of the alveolar walls are destroyed. Air becomes trapped in the overexpanded alveoli, leading to inadequate gas (oxygen and carbon dioxide) exchange.
Cigarette smoking is the most common risk factor for COPD, especially with chronic bronchitis and emphysema. There is no cure for COPD at this time; however, it remains preventable in most cases. Because cigarette smoking is the most directly related cause, not smoking significantly prevents COPD from developing. Quitting smoking will slow the disease process.
Medications frequently prescribed for COPD include the following:
• Glucocorticoids (steroids) are used to decrease inflammation.
• Expectorants are used to assist in loosening mucus from the airways.
• Antibiotics may be prescribed to prevent serious complications from bacterial infections.
See the Key Websites at the end of the chapter for recommended methods for smoking cessation.
Bronchial Asthma
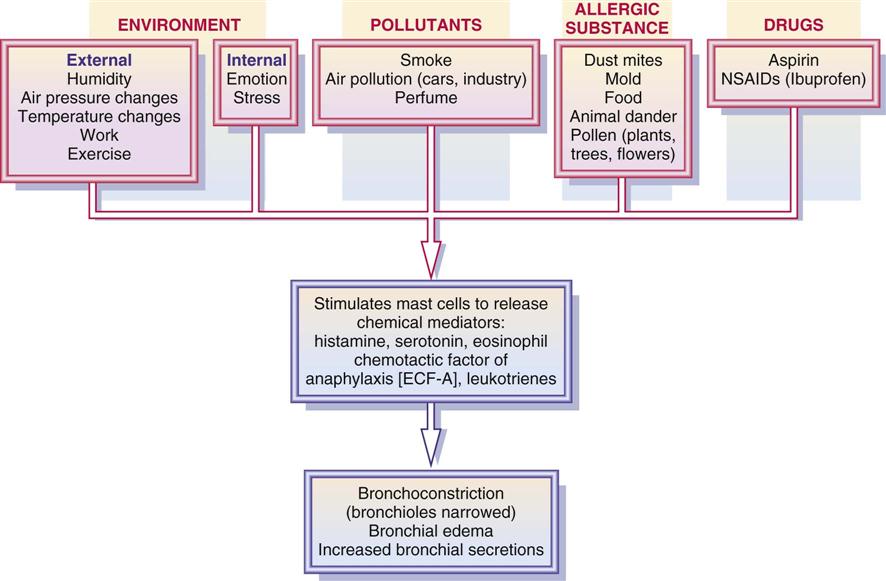
Bronchial asthma is a COPD characterized by periods of bronchospasm resulting in wheezing and difficulty breathing. Bronchospasm, or bronchoconstriction, results when the lung tissue is exposed to extrinsic or intrinsic factors that stimulate a bronchoconstrictive response. Factors that can trigger an asthmatic attack (bronchospasm) include humidity; air pressure changes; temperature changes; smoke; fumes (exhaust, perfume); stress; emotional upset; exercise; and allergies to animal dander, dust mites, food, and drugs (e.g., aspirin, ibuprofen, beta-adrenergic blockers). Reactive airway disease (RAD) is a cause of asthma resulting from sensitivity stimulation from allergens, dust, temperature changes, and cigarette smoking.
Pathophysiology
Mast cells, found in connective tissue throughout the body, are directly involved in the asthmatic response, particularly to extrinsic factors. Allergens attach themselves to mast cells and basophils, resulting in an antigen-antibody reaction on the mast cells in the lung; thus the mast cells stimulate the release of chemical mediators such as histamines, cytokines, serotonin, eosinophil chemotactic factor of anaphylaxis (ECF-A), and leukotrienes. Eosinophil counts are usually elevated during an allergic reaction, which indicates that an inflammatory process is occurring. These chemical mediators stimulate bronchial constriction, mucous secretions, inflammation, and pulmonary congestion. Histamine and ECF-A are strong bronchoconstrictors. Bronchial smooth muscles are wrapped spirally around the bronchioles and contract as they are stimulated by these mediators. Exposure to an allergen results in bronchial hyperresponsiveness, epithelial shedding of the bronchial wall, mucous gland hyperplasia and hypersecretion, leakage of plasma leading to swelling, and bronchoconstriction.
Figure 41-2 shows factors contributing to bronchoconstriction. Cyclic adenosine monophosphate (cyclic AMP, or cAMP), a cellular signaling molecule, is involved in many cellular activities and is responsible for maintaining bronchodilation. When histamine, ECF-A, and leukotrienes inhibit the action of cAMP, bronchoconstriction results. The sympathomimetic (adrenergic) bronchodilators and methylxanthines increase the amount of cAMP in bronchial tissue cells.
In an acute asthmatic attack, the short-acting sympathomimetics (beta2-adrenergic agonists) are the first line of defense. They promote cAMP production and enhance bronchodilation. Long-acting sympathomimetics are used for maintenance. Sympathomimetics (adrenergics) are also discussed in Chapter 18.
Sympathomimetics: Alpha- and Beta2-Adrenergic Agonists
Sympathomimetics increase cAMP, causing dilation of the bronchioles. In an acute bronchospasm caused by anaphylaxis from an allergic reaction, the nonselective sympathomimetic epinephrine (Adrenalin), which is an alpha1, beta1, and beta2 agonist, is given subcutaneously to promote bronchodilation and elevate blood pressure. Epinephrine is administered in emergency situations to restore circulation and increase airway patency (see Chapter 59).
For bronchospasm associated with chronic asthma or COPD, selective beta2-adrenergic agonists are given by aerosol or as a tablet. These drugs act primarily on the beta2 receptors; therefore side effects are less severe than those of epinephrine, which acts on alpha1, beta1, and beta2 receptors.
Albuterol
The newer beta-adrenergic drugs for asthma are more selective for beta2 receptors. High doses or overuse of the beta2-adrenergic agents for asthma may cause some degree of beta1 response such as nervousness, tremor, and increased pulse rate. The ideal beta2 agonist is one that has a rapid onset of action, longer duration of action, and few side effects. Albuterol (Proventil, Ventolin) is a selective beta2 drug that is effective for treatment and control of asthma by causing bronchodilation with long duration of action. (See Prototype Drug Chart 18-2 for drug data related to albuterol.)
Metaproterenol
The second beta-adrenergic agent is metaproterenol (Alupent), which was first marketed in 1961. It has some beta1 effect but is primarily used as a beta2 agent. It can be administered orally or by inhalation with a metered-dose inhaler or a nebulizer.
For long-term asthma treatment, beta2-adrenergic agonists are frequently administered by inhalation. This route of administration usually delivers more of the drug directly to the constricted bronchial site. The effective inhalation drug dose is less than it would be by the oral route, and there are also fewer side effects using this route. The onset of action of the drug is more rapid by inhalation (1 minute) than orally (15 minutes).
Isoproterenol
The first beta-adrenergic agent used for bronchospasm was isoproterenol (Isuprel), introduced in 1941. It has no alpha-agonist properties, but it is considered a nonselective beta agonist because it stimulates both beta1 and beta2 receptors. Beta1 stimulation causes heart rate increases, and tachycardia may result. Beta2 stimulation promotes bronchodilation. Isoproterenol is administered by inhalation, using an aerosol inhaler or nebulizer, or intravenously (IV) for severe asthmatic attacks. Its duration of action is short. Because of its severe side effects from beta1 response, it is seldom prescribed.
Use of an Aerosol Inhaler
If the beta2 agonist is given by metered-dose inhaler (MDI) or dry-powder inhaler (DPI), correct use of the inhaler and dosage intervals need to be explained to the patient. If the patient does not receive effective relief from the inhaler, either the technique is faulty or the canister is empty. A spacer device may be attached to the inhaler to improve drug delivery to the lung with less deposition in the mouth. If the patient does not use the inhaler properly to deliver the drug dose, the medication may be trapped in the upper airways. Because of drug inhalation, mouth dryness and throat irritation could result.
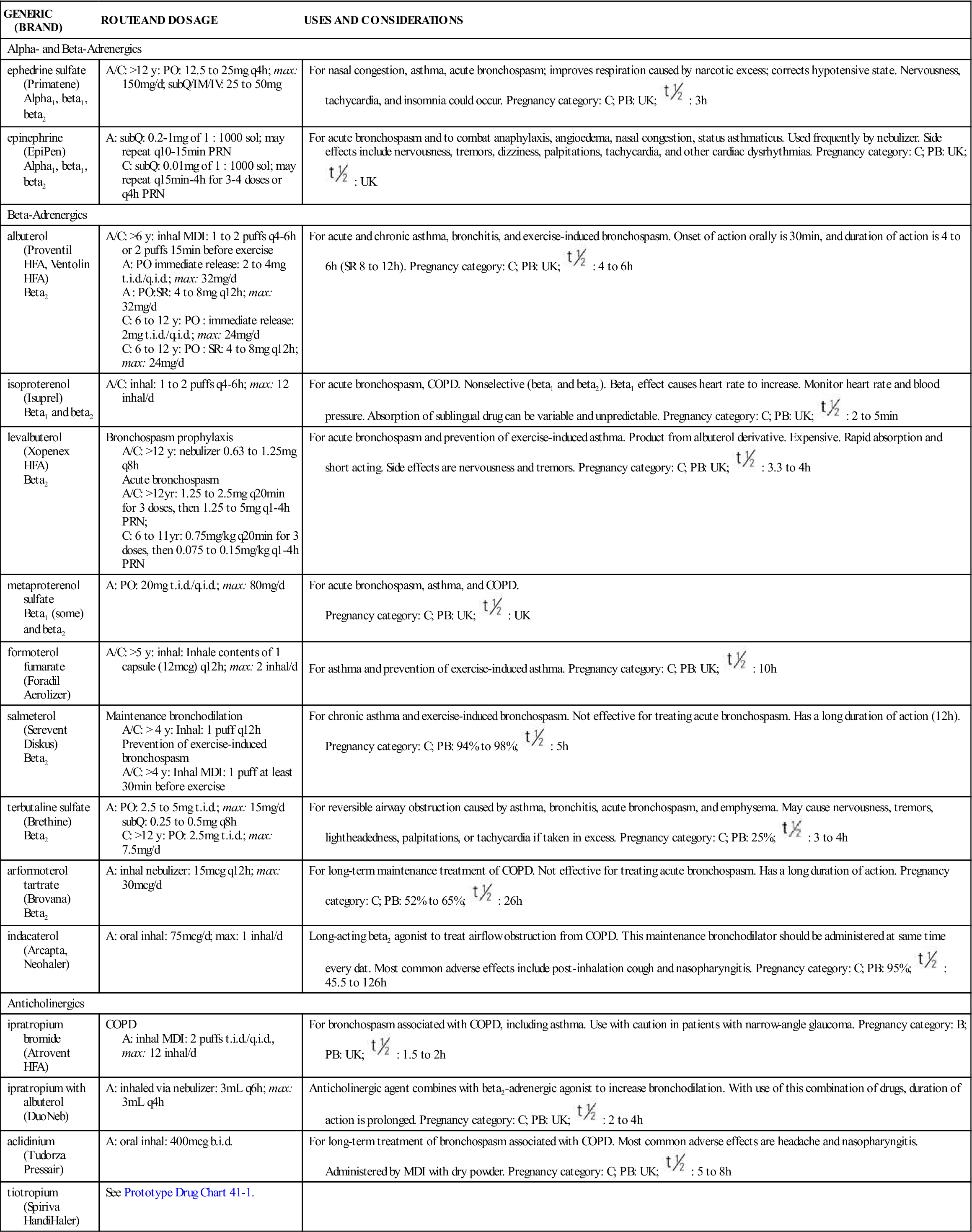
Excessive use of the aerosol drug can lead to tolerance and loss of drug effectiveness. Occasionally, severe paradoxical airway resistance (bronchoconstriction) develops with repeated, excessive use of sympathomimetic oral inhalation. Frequent dosing can cause tremors, nervousness, and increased heart rate. Table 41-1 lists the sympathomimetics used as bronchodilators.
TABLE 41-1
ADRENERGIC BRONCHODILATORS AND ANTICHOLINERGICS
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Alpha- and Beta-Adrenergics | ||
| ephedrine sulfate (Primatene) Alpha1, beta1, beta2 | A/C: >12 y: PO: 12.5 to 25 mg q4h; max: 150 mg/d; subQ/IM/IV: 25 to 50 mg | For nasal congestion, asthma, acute bronchospasm; improves respiration caused by narcotic excess; corrects hypotensive state. Nervousness, tachycardia, and insomnia could occur. Pregnancy category: C; PB: UK;  : 3 h : 3 h |
| epinephrine (EpiPen) Alpha1, beta1, beta2 | A: subQ: 0.2-1 mg of 1 : 1000 sol; may repeat q10-15min PRN C: subQ: 0.01 mg of 1 : 1000 sol; may repeat q15min-4h for 3-4 doses or q4h PRN | For acute bronchospasm and to combat anaphylaxis, angioedema, nasal congestion, status asthmaticus. Used frequently by nebulizer. Side effects include nervousness, tremors, dizziness, palpitations, tachycardia, and other cardiac dysrhythmias. Pregnancy category: C; PB: UK;  : UK : UK |
| Beta-Adrenergics | ||
| albuterol (Proventil HFA, Ventolin HFA) Beta2 | A/C: >6 y: inhal MDI: 1 to 2 puffs q4-6h or 2 puffs 15 min before exercise A: PO immediate release: 2 to 4 mg t.i.d./q.i.d.; max: 32 mg/d A : PO:SR: 4 to 8 mg q12h; max: 32 mg/d C: 6 to 12 y: PO : immediate release: 2 mg t.i.d./q.i.d.; max: 24 mg/d C: 6 to 12 y: PO : SR: 4 to 8 mg q12h; max: 24 mg/d | For acute and chronic asthma, bronchitis, and exercise-induced bronchospasm. Onset of action orally is 30 min, and duration of action is 4 to 6 h (SR 8 to 12 h). Pregnancy category: C; PB: UK;  : 4 to 6 h : 4 to 6 h |
| isoproterenol (Isuprel) Beta1 and beta2 | A/C: inhal: 1 to 2 puffs q4-6h; max: 12 inhal/d | For acute bronchospasm, COPD. Nonselective (beta1 and beta2). Beta1 effect causes heart rate to increase. Monitor heart rate and blood pressure. Absorption of sublingual drug can be variable and unpredictable. Pregnancy category: C; PB: UK;  : 2 to 5 min : 2 to 5 min |
| levalbuterol (Xopenex HFA) Beta2 | Bronchospasm prophylaxis A/C: >12 y: nebulizer 0.63 to 1.25 mg q8h Acute bronchospasm A/C: >12yr: 1.25 to 2.5 mg q20min for 3 doses, then 1.25 to 5 mg q1-4h PRN; C: 6 to 11 yr: 0.75 mg/kg q20min for 3 doses, then 0.075 to 0.15 mg/kg q1-4h PRN | For acute bronchospasm and prevention of exercise-induced asthma. Product from albuterol derivative. Expensive. Rapid absorption and short acting. Side effects are nervousness and tremors. Pregnancy category: C; PB: UK;  : 3.3 to 4 h : 3.3 to 4 h |
| metaproterenol sulfate Beta1 (some) and beta2 | A: PO: 20 mg t.i.d./q.i.d.; max: 80 mg/d | For acute bronchospasm, asthma, and COPD. Pregnancy category: C; PB: UK;  : UK : UK |
| formoterol fumarate (Foradil Aerolizer) | A/C: >5 y: inhal: Inhale contents of 1 capsule (12 mcg) q12h; max: 2 inhal/d | For asthma and prevention of exercise-induced asthma. Pregnancy category: C; PB: UK;  : 10 h : 10 h |
| salmeterol (Serevent Diskus) Beta2 | Maintenance bronchodilation A/C: > 4 y: Inhal: 1 puff q12h Prevention of exercise-induced bronchospasm A/C: >4 y: Inhal MDI: 1 puff at least 30 min before exercise | For chronic asthma and exercise-induced bronchospasm. Not effective for treating acute bronchospasm. Has a long duration of action (12 h). Pregnancy category: C; PB: 94% to 98%;  : 5 h : 5 h |
| terbutaline sulfate (Brethine) Beta2 | A: PO: 2.5 to 5 mg t.i.d.; max: 15 mg/d subQ: 0.25 to 0.5 mg q8h C: >12 y: PO: 2.5 mg t.i.d.; max: 7.5 mg/d | For reversible airway obstruction caused by asthma, bronchitis, acute bronchospasm, and emphysema. May cause nervousness, tremors, lightheadedness, palpitations, or tachycardia if taken in excess. Pregnancy category: C; PB: 25%;  : 3 to 4 h : 3 to 4 h |
| arformoterol tartrate (Brovana) Beta2 | A: inhal nebulizer: 15 mcg q12h; max: 30 mcg/d | For long-term maintenance treatment of COPD. Not effective for treating acute bronchospasm. Has a long duration of action. Pregnancy category: C; PB: 52% to 65%;  : 26 h : 26 h |
| indacaterol (Arcapta, Neohaler) | A: oral inhal: 75 mcg/d; max: 1 inhal/d | Long-acting beta2 agonist to treat airflow obstruction from COPD. This maintenance bronchodilator should be administered at same time every dat. Most common adverse effects include post-inhalation cough and nasopharyngitis. Pregnancy category: C; PB: 95%;  : 45.5 to 126 h : 45.5 to 126 h |
| Anticholinergics | ||
| ipratropium bromide (Atrovent HFA) | COPD A: inhal MDI: 2 puffs t.i.d./q.i.d., max: 12 inhal/d | For bronchospasm associated with COPD, including asthma. Use with caution in patients with narrow-angle glaucoma. Pregnancy category: B; PB: UK;  : 1.5 to 2 h : 1.5 to 2 h |
| ipratropium with albuterol (DuoNeb) | A: inhaled via nebulizer: 3 mL q6h; max: 3 mL q4h | Anticholinergic agent combines with beta2-adrenergic agonist to increase bronchodilation. With use of this combination of drugs, duration of action is prolonged. Pregnancy category: C; PB: UK;  : 2 to 4 h : 2 to 4 h |
| aclidinium (Tudorza Pressair) | A: oral inhal: 400 mcg b.i.d. | For long-term treatment of bronchospasm associated with COPD. Most common adverse effects are headache and nasopharyngitis. Administered by MDI with dry powder. Pregnancy category: C; PB: UK;  : 5 to 8 h : 5 to 8 h |
| tiotropium (Spiriva HandiHaler) | See Prototype Drug Chart 41-1. | |
Side Effects and Adverse Reactions
The side effects and adverse reactions of epinephrine include tremors, dizziness, hypertension, tachycardia, heart palpitations, cardiac dysrhythmias, and angina. The patient needs to be closely monitored when epinephrine is administered.
The side effects associated with beta2-adrenergic drugs (e.g., albuterol) include tremors, headaches, nervousness, increased pulse rate, and palpitations (high doses). The beta2 agonists may increase blood glucose levels, so patients with diabetes should be taught to closely monitor their serum glucose levels. Side effects of beta2 agonists may diminish after 1 week or longer. The bronchodilating effects may decrease with continued use. It is believed that tolerance to these drugs can develop; if this occurs, the dose may need to be increased. Failure to respond to a previously effective dose may indicate worsening asthma that requires reevaluation before increasing the dose.
Anticholinergics
Tiotropium (Spiriva) is an anticholinergic drug used for maintenance treatment of bronchospasms associated with COPD. This drug is administered by inhalation only with the HandiHaler device (dry-powder capsule inhaler). Patients should discard any capsules that are opened and not used immediately. HandiHalers should be washed with warm water and dried. The most common adverse effects of tiotropium include dry mouth, constipation, vomiting, dyspepsia, abdominal pain, depression, insomnia, headache, joint pain, and peripheral edema. Chest pain has been reported following tiotropium administration. Prototype Drug Chart 41-1 lists the drug data related to tiotropium.
 , half-life; t.i.d., three times a day; UK, unknown; y, year; >, greater than.
, half-life; t.i.d., three times a day; UK, unknown; y, year; >, greater than. : 5-6 d
: 5-6 d


