Antihypertensives
Objectives
• Differentiate the pharmacologic action of the various categories of antihypertensive drugs.
• Apply the nursing process related to antihypertensives including nursing interventions and teaching.
• Describe the blood pressure guidelines for determining hypertension.
Key Terms
antihypertensive, p. 635
essential hypertension, p. 633
hypertension, p. 633
secondary hypertension, p. 633
sympatholytics, p. 635
Hypertension
Hypertension is an increase in blood pressure such that the systolic pressure is greater than 140 mm Hg and the diastolic pressure is greater than 90 mm Hg. Essential hypertension is the most common type, affecting 90% of persons with high blood pressure. The exact origin of essential hypertension is unknown; however, contributing factors may include family history of hypertension, hyperlipidemia, African-American background, diabetes, aging, stress, excessive alcohol ingestion, smoking, and obesity. Ten percent of hypertension cases are related to renal and endocrine disorders and are classified as secondary hypertension.
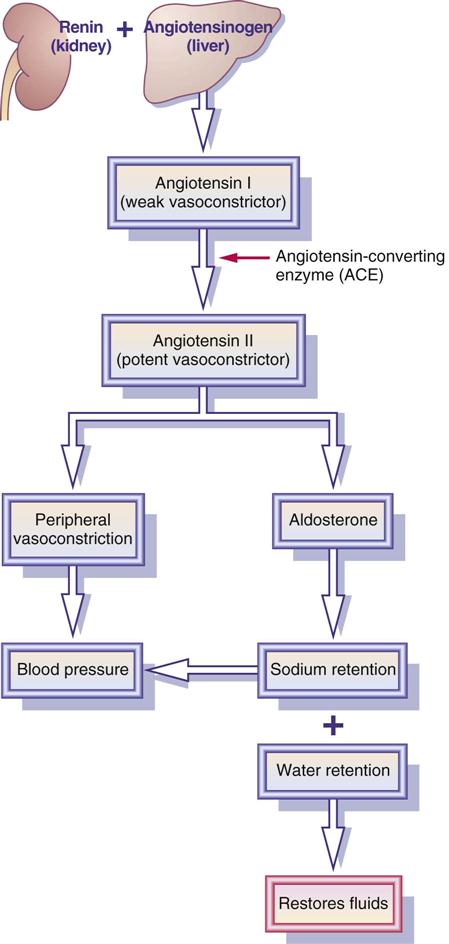
Selected Regulators of Blood Pressure
The kidneys and blood vessels strive to regulate and maintain a “normal” blood pressure. The kidneys regulate blood pressure by control of fluid volume and the renin-angiotensin-aldosterone system. Kidneys control sodium and water elimination/retention, which affects cardiac output and systemic arterial blood pressure. Figure 44-1 illustrates the renin-angiotensin-aldosterone system (RAAS). Renin (from the renal cells) stimulates production of angiotensin II (a potent vasoconstrictor), which causes the release of aldosterone (adrenal hormone that promotes sodium retention and thereby water retention). Retention of sodium and water causes fluid volume to increase, elevating blood pressure.
The baroreceptors in the aorta and carotid sinus and the vasomotor center in the medulla also assist in the regulation of blood pressure. Catecholamines such as norepinephrine, released from the sympathetic nerve terminals, and epinephrine, released from the adrenal medulla, increase blood pressure through vasoconstriction activity.
Other hormones that contribute to blood pressure regulation are antidiuretic hormone (ADH), atrial natriuretic peptide (ANP) hormone, and brain natriuretic peptide (BNP) hormone. ADH is produced by the hypothalamus and is stored and released by the posterior pituitary gland (neurohypophysis). This hormone stimulates the kidneys to conserve and retain water when there is a fluid volume deficit. When there is fluid overload, ADH secretion is inhibited, and the kidneys then excrete more water.
Physiologic Risk Factors
Certain physiologic risk factors contribute to hypertension. A diet high in saturated fat and simple carbohydrates can increase blood pressure. Carbohydrate intake can affect sympathetic nervous activity. Alcohol increases renin secretions, causing the production of angiotensin II. Obesity affects the sympathetic and cardiovascular systems by increasing cardiac output, stroke volume, and left ventricular filling. Two-thirds of hypertensive persons are obese. Normally weight loss can decrease hypertension, as can mild to moderate sodium restriction.
Cultural Responses to Antihypertensive Agents
African Americans are more likely to develop hypertension at an earlier age than white Americans. They also have a higher mortality rate from hypertension than the white population. The use of beta-adrenergic blockers (beta blockers) and angiotensin-converting enzyme (ACE) inhibitors is less effective for the control of hypertension in African Americans unless the drug is combined or given with a diuretic. This group is susceptible to low-renin hypertension; therefore, they do not respond well to beta blockers and ACE inhibitors. The antihypertensive drugs that are effective for African Americans are alpha1 blockers and calcium channel blockers (calcium blockers). African-American patients do respond to diuretics as the initial monotherapy for controlling hypertension. White patients usually have high-renin hypertension and respond well to all antihypertensive agents.
Asian Americans are twice as sensitive as whites to beta blockers and other antihypertensives. A reduction in antihypertensive dosing is frequently needed. Native Americans have a reduced or lower response to beta blockers compared with whites. Monitoring blood pressure and drug dosing should be an ongoing assessment for patients in these cultural groups.
Hypertension in Older Adults
By 65 years of age, 26% of men and 30% of women are hypertensive. Between 65 and 75 years of age, 30% of men and 45% of women are hypertensive. Both systolic and diastolic hypertension are associated with increased cardiovascular morbidity and mortality. With antihypertensive therapy, the greatest decrease in cardiovascular disorders is 34% for stroke and 19% for coronary heart disease.
One of the troublesome side effects of the use of antihypertensive agents in older adults, especially frail or institutionalized persons, is orthostatic (postural) hypotension. This episode of sudden low blood pressure presents dizziness due to blood pooling in lower extremities when an individual changes to an upright position. In older adults, the sympathetic nervous system does not respond as quickly to correct the situation, especially when potentiated by antihypertensive drug administration. If orthostatic hypotension occurs, the antihypertensive drug dose may need to be decreased or another antihypertensive drug used. Older adults with hypertension should be instructed to modify their lifestyle activities. This includes restricting dietary sodium to 2400 mg daily, avoiding tobacco, modifying diet, exercising, and decreasing stress.
Nonpharmacologic Control of Hypertension
A sufficient decrease in blood pressure can be accomplished by nonpharmacologic methods. There are many nonpharmacologic ways to decrease blood pressure, but if the systolic pressure is greater than 140 mm Hg, antihypertensive drugs are generally ordered. Nondrug methods to decrease blood pressure include stress-reduction techniques, exercise, salt restriction, decreased alcohol ingestion, and smoking cessation.
When hypertension cannot be controlled by nonpharmacologic means, antihypertensive drugs are prescribed. However, nonpharmacologic methods should be combined with antihypertensive drugs to control hypertension.
Guidelines for Hypertension
Blood pressure guidelines for determining hypertension have been revised and are contained in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, or JNC 7. The purpose of these guidelines is to decrease the risk of cardiovascular disease (CVD) in the American population. The guideline for normal blood pressure is less than 120/80 mm Hg. Prehypertension is defined as systolic blood pressure (SBP) of 120 to 139 and diastolic blood pressure (DBP) of 80 to 89. Stage 1 hypertension falls between 140/90 and 159/99, and stage 2 hypertension is 160/100 or greater.
Two out of three patients with hypertension have uncontrolled blood pressure or are not optimally treated. SBP is more important than DBP as a CVD risk for patients 50 years of age or older. According to the JNC 7, if the blood pressure is greater than 20/10 mm Hg above goal, a drug regimen should be started. CVD risk doubles with each increase of 20/10 mm Hg, starting at 115/75 mm Hg.
Pharmacologic Control of Hypertension
An individualized approach to the treatment of hypertension is used by many health care providers. All drugs are considered initial agents when first prescribed for hypertension. Reduction of other cardiovascular risk factors and the use of fewer drugs (i.e., substituting instead of adding drugs) at the lowest effective doses are emphasized. Often more than one antihypertensive is used to control blood pressure, which also may lead to less adverse effects.
Antihypertensive drugs, used either singly or in combination with other drugs, are classified into six categories: (1) diuretics, (2) sympatholytics (sympathetic depressants), (3) direct-acting arteriolar vasodilators, (4) ACE inhibitors, (5) angiotensin II receptor blockers (ARBs), and (6) calcium channel blockers.
Diuretics
Diuretics promote sodium depletion, which decreases extracellular fluid volume (ECFV). Diuretics are effective as first-line drugs for treating mild hypertension. Hydrochlorothiazide (HCTZ) is the most frequently prescribed diuretic for controlling mild hypertension by decreasing excess fluid volume. It can be used alone for recently diagnosed or mild hypertension or with other antihypertensive drugs. Many antihypertensive drugs can cause fluid retention; therefore diuretics are often administered together with antihypertensive agents. The various types of diuretics are discussed in Chapter 43.
Thiazide diuretics are not recommended for patients with renal insufficiency (creatinine clearance <30 mL/min). The loop (high-ceiling) diuretics such as furosemide (Lasix) are usually recommended, because they do not depress renal blood flow. Loop diuretics are not used if hypertension is the result of renin-angiotensin-aldosterone system involvement because they tend to elevate serum renin level immediately. Instead of a single thiazide drug, a combination of potassium-wasting and potassium-sparing diuretics may be useful; less potassium excretion would occur. In addition, thiazides can be combined with other antihypertensive drugs to increase their effectiveness. Box 44-1 lists the combinations of thiazides with other drugs. Many drug products on the market include combinations of thiazide diuretics and potassium-sparing diuretics, beta blockers, ACE inhibitors, or angiotensin II receptor blockers. ACE inhibitors tend to increase serum potassium (K) levels, so when they are combined with a thiazide diuretic, serum potassium loss is minimized.
Sympatholytics (Sympathetic Depressants)
The sympatholytics comprise five groups of drugs: (1) beta-adrenergic blockers, (2) centrally acting alpha2 agonists, (3) alpha-adrenergic blockers, (4) adrenergic neuron blockers (peripherally acting sympatholytics), and (5) alpha1– and beta1-adrenergic blockers. Beta-adrenergic blockers block the beta receptors, and alpha-adrenergic blockers block the alpha receptors.
Beta-Adrenergic Blockers
Beta-adrenergic blockers, frequently called beta blockers, are used as antihypertensive drugs or in combination with a diuretic. Beta blockers are also used as antianginals and antidysrhythmics and are discussed in this context in Chapter 42.
Beta (β+ and β−)-adrenergic blockers reduce cardiac output by diminishing the sympathetic nervous system response to decrease basal sympathetic tone. With continued use of beta blockers, vascular resistance is diminished, and blood pressure is lowered. Beta blockers reduce heart rate, contractility, and renin release. There is a greater hypotensive response in patients with higher renin levels.
African-American hypertensive patients do not respond well to beta blockers alone for the control of hypertension. Instead, hypertension can be controlled by combining beta blockers with diuretics.
There are many types of beta blockers. Nonselective beta blockers, such as propranolol (Inderal) and carvedilol (Coreg) inhibit beta1 (heart) and beta2 (bronchial) receptors. Heart rate slows (blood pressure decreases secondary to the decrease in heart rate), and bronchoconstriction occurs because of unopposed parasympathetic tone. Cardioselective beta blockers are preferred, because they act mainly on the beta1 rather than the beta2 receptors and bronchoconstriction is less likely to occur. Acebutolol (Sectral), atenolol (Tenormin), betaxolol (Kerlone), bisoprolol (Zebeta), and metoprolol (Lopressor) are cardioselective beta blockers that block beta1 receptors.
Cardioselectivity does not confer absolute protection from bronchoconstriction. In tests measuring forced expiratory volume in 1 second (FEV1) as a measure of β− reactivity, only atenolol demonstrated true protection. Other cardioselective beta blockers were only partially effective. Studies also show that at the upper end of the dosage range, cardioselectivity is less effective. In patients with preexisting bronchospasm or other pulmonary disease, beta blockers, even those considered cardioselective, should be used with caution. Some experts regard this as a relative contraindication. The real value of beta selectivity is in maintaining renal blood flow and minimizing the hypoglycemic effects of beta blockade.
The combination of beta blockers with hydrochlorothiazides is packaged together in tablet form (see Box 44-1). Usually the hydrochlorothiazide dose is 12.5 to 25 mg, approximately half the average dose.
Beta blockers tend to be more effective in lowering blood pressure in patients who have an elevated serum renin level. The cardioselective prototype drug metoprolol (Lopressor) is presented in Prototype Drug Chart 44-1.
Beta blockers should not be used by patients with second- or third-degree atrioventricular (AV) block or sinus bradycardia. A noncardioselective beta blocker such as propranolol (Inderal) should not be given to a patient with chronic obstructive pulmonary disease (COPD).
Pharmacokinetics
Metoprolol is well absorbed from the gastrointestinal tract. Its half-life is short and its protein-binding power is low.
Pharmacodynamics
Cardioselective beta-adrenergic blockers block beta1 receptors, thereby decreasing heart rate and blood pressure. The nonselective beta blockers block beta1 and beta2 receptors, which can result in bronchial constriction. Beta blockers cross the placental barrier and are excreted in breast milk.
The onset of action of oral beta blockers is usually 30 minutes or less, and the duration of action is 6 to 12 hours. When beta blockers are administered intravenously, the onset of action is immediate, peak time is 20 minutes (compared with 1.5 hours orally), and duration of action is 4 to 10 hours.
Side Effects and Adverse Reactions.
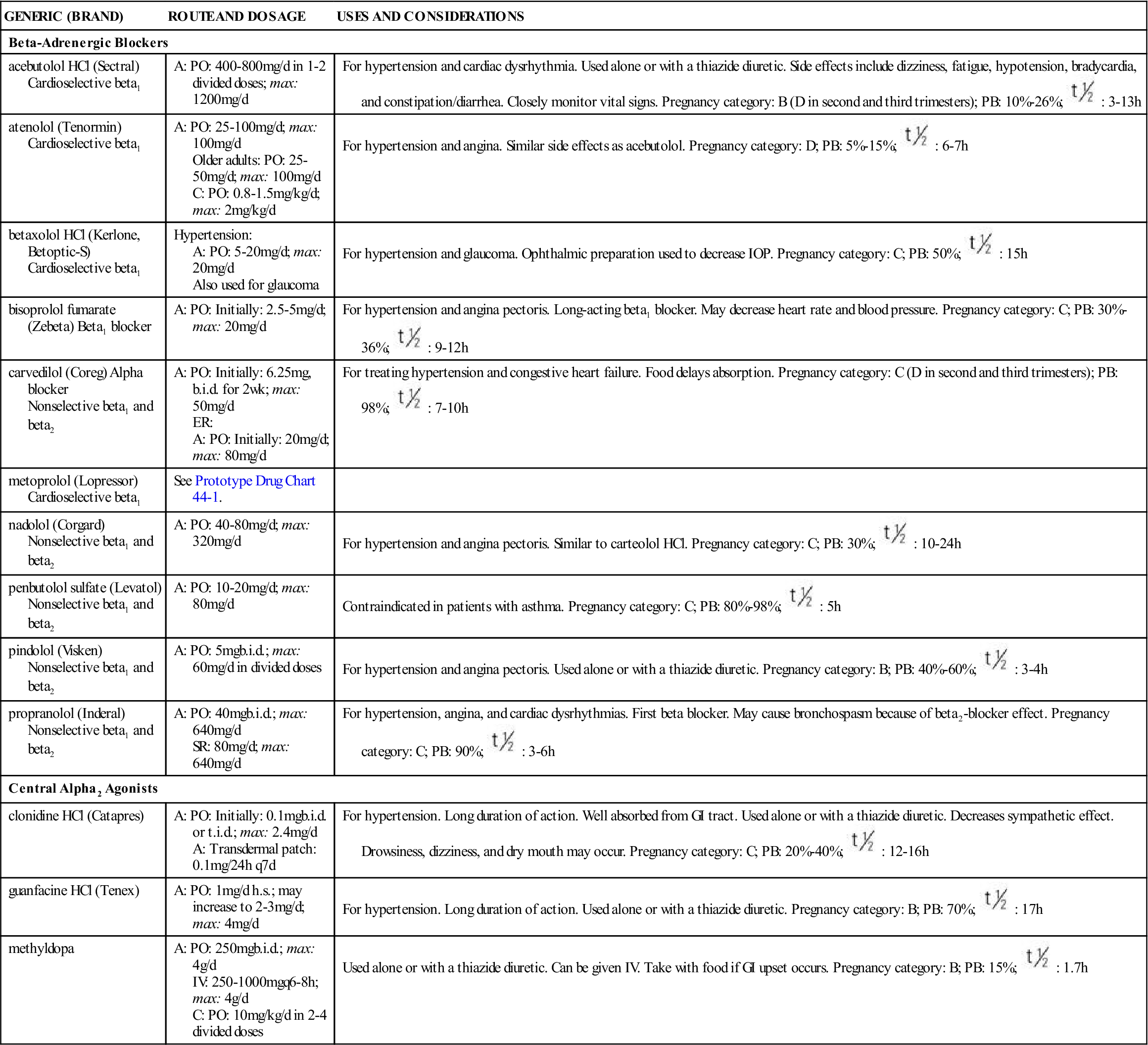
Side effects and adverse reactions include decreased pulse rate, markedly decreased blood pressure, and (with noncardioselective beta1 and beta2 blockers) bronchospasm. Beta blockers should not be abruptly discontinued, because rebound hypertension, angina, dysrhythmias, and myocardial infarction can result. Beta blockers can cause dizziness, insomnia, depression, fatigue, nightmares, and sexual dysfunction. Other side effects are discussed in Chapter 42. Table 44-1 lists the beta blockers used to treat hypertension and their dosages, uses and considerations.
![]() TABLE 44-1
TABLE 44-1
ANTIHYPERTENSIVES: BETA BLOCKERS AND CENTRAL ALPHA2 AGONISTS
| GENERIC (BRAND) | ROUTE AND DOSAGE | USES AND CONSIDERATIONS |
| Beta-Adrenergic Blockers | ||
| acebutolol HCl (Sectral) Cardioselective beta1 | A: PO: 400-800 mg/d in 1-2 divided doses; max: 1200 mg/d | For hypertension and cardiac dysrhythmia. Used alone or with a thiazide diuretic. Side effects include dizziness, fatigue, hypotension, bradycardia, and constipation/diarrhea. Closely monitor vital signs. Pregnancy category: B (D in second and third trimesters); PB: 10%-26%;  : 3-13 h : 3-13 h |
| atenolol (Tenormin) Cardioselective beta1 | A: PO: 25-100 mg/d; max: 100 mg/d Older adults: PO: 25-50 mg/d; max: 100 mg/d C: PO: 0.8-1.5 mg/kg/d; max: 2 mg/kg/d | For hypertension and angina. Similar side effects as acebutolol. Pregnancy category: D; PB: 5%-15%;  : 6-7 h : 6-7 h |
| betaxolol HCl (Kerlone, Betoptic-S) Cardioselective beta1 | Hypertension: A: PO: 5-20 mg/d; max: 20 mg/d Also used for glaucoma | For hypertension and glaucoma. Ophthalmic preparation used to decrease IOP. Pregnancy category: C; PB: 50%;  : 15 h : 15 h |
| bisoprolol fumarate (Zebeta) Beta1 blocker | A: PO: Initially: 2.5-5 mg/d; max: 20 mg/d | For hypertension and angina pectoris. Long-acting beta1 blocker. May decrease heart rate and blood pressure. Pregnancy category: C; PB: 30%-36%;  : 9-12 h : 9-12 h |
| carvedilol (Coreg) Alpha blocker Nonselective beta1 and beta2 | A: PO: Initially: 6.25 mg, b.i.d. for 2 wk; max: 50 mg/d ER: A: PO: Initially: 20 mg/d; max: 80 mg/d | For treating hypertension and congestive heart failure. Food delays absorption. Pregnancy category: C (D in second and third trimesters); PB: 98%;  : 7-10 h : 7-10 h |
| metoprolol (Lopressor) Cardioselective beta1 | See Prototype Drug Chart 44-1. | |
| nadolol (Corgard) Nonselective beta1 and beta2 | A: PO: 40-80 mg/d; max: 320 mg/d | For hypertension and angina pectoris. Similar to carteolol HCl. Pregnancy category: C; PB: 30%;  : 10-24 h : 10-24 h |
| penbutolol sulfate (Levatol) Nonselective beta1 and beta2 | A: PO: 10-20 mg/d; max: 80 mg/d | Contraindicated in patients with asthma. Pregnancy category: C; PB: 80%-98%;  : 5 h : 5 h |
| pindolol (Visken) Nonselective beta1 and beta2 | A: PO: 5 mg b.i.d.; max: 60 mg/d in divided doses | For hypertension and angina pectoris. Used alone or with a thiazide diuretic. Pregnancy category: B; PB: 40%-60%;  : 3-4 h : 3-4 h |
| propranolol (Inderal) Nonselective beta1 and beta2 | A: PO: 40 mg b.i.d.; max: 640 mg/d SR: 80 mg/d; max: 640 mg/d | For hypertension, angina, and cardiac dysrhythmias. First beta blocker. May cause bronchospasm because of beta2-blocker effect. Pregnancy category: C; PB: 90%;  : 3-6 h : 3-6 h |
| Central Alpha2 Agonists | ||
| clonidine HCl (Catapres) | A: PO: Initially: 0.1 mg b.i.d. or t.i.d.; max: 2.4 mg/d A: Transdermal patch: 0.1 mg/24 h q7d | For hypertension. Long duration of action. Well absorbed from GI tract. Used alone or with a thiazide diuretic. Decreases sympathetic effect. Drowsiness, dizziness, and dry mouth may occur. Pregnancy category: C; PB: 20%-40%;  : 12-16 h : 12-16 h |
| guanfacine HCl (Tenex) | A: PO: 1 mg/d h.s.; may increase to 2-3 mg/d; max: 4 mg/d | For hypertension. Long duration of action. Used alone or with a thiazide diuretic. Pregnancy category: B; PB: 70%;  : 17 h : 17 h |
| methyldopa | A: PO: 250 mg b.i.d.; max: 4 g/d IV: 250-1000 mg q6-8h; max: 4 g/d C: PO: 10 mg/kg/d in 2-4 divided doses | Used alone or with a thiazide diuretic. Can be given IV. Take with food if GI upset occurs. Pregnancy category: B; PB: 15%;  : 1.7 h : 1.7 h |
Noncardioselective beta blockers inhibit the liver’s ability to convert glycogen to glucose in response to hypoglycemia. Because of this side effect, beta blockers should be used with caution in patients with diabetes mellitus. In addition, the depression of heart rate masks the symptom (tachycardia) of hypotension.
 : 3-7 h
: 3-7 h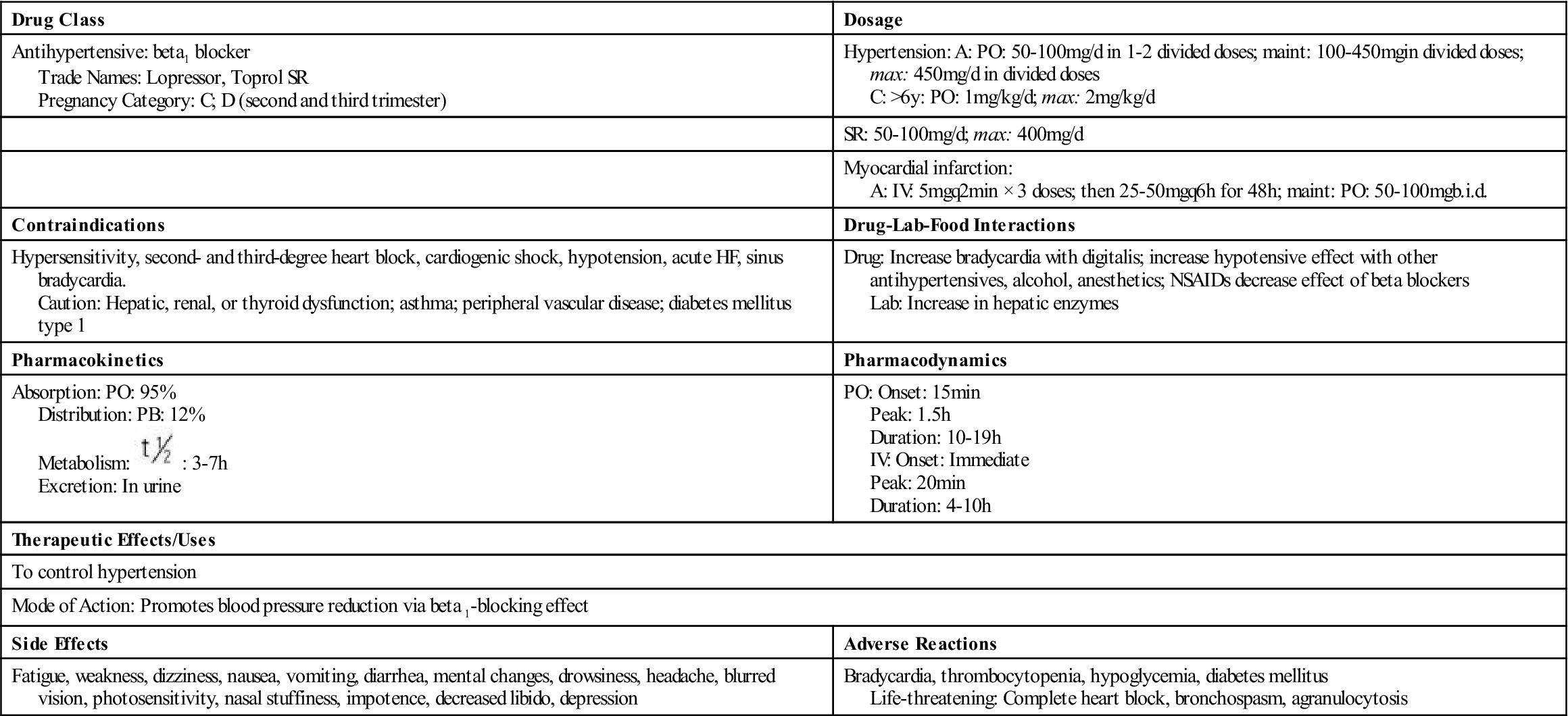
 , half-life.
, half-life. , half-life; t.i.d., three times a day; UK, unknown; wk, week; >, greater than; <, less than.
, half-life; t.i.d., three times a day; UK, unknown; wk, week; >, greater than; <, less than.



















