Antidepressants and Mood Stabilizers
Objectives
• Describe the side effects and adverse reactions of antidepressants.
• Apply the nursing process to the patient taking lithium, carbamazepine, and valproic acid.
Key Terms
antidepressants, p. 386
atypical antidepressants, p. 387
bipolar affective disorder, p. 387
depression, p. 386
dysphoria, p. 387
monoamine oxidase inhibitors, p. 387
reactive depression, p. 387
selective serotonin reuptake inhibitors, p. 387
serotonin norepinephrine reuptake inhibitors, p. 387
tricyclic antidepressants, p. 387
Antidepressants are used for depressive episodes that are accompanied by feelings of hopelessness and helplessness. They can be prescribed for 1 month to 12 months or perhaps longer.
Mood-stabilizer agents such as lithium are effective for bipolar affective disorder. Drug therapy for treating bipolar disorder is discussed in this chapter.
Depression
Depression is the most common psychiatric problem, affecting approximately 10% to 20% of the population. Only 33% of depressed persons receive medical or psychiatric help. Women between the ages of 25 and 45 years are two to three times more likely to experience major depression than men. Depression is characterized primarily by mood changes and loss of interest in normal activities. It is second only to hypertension as the most common chronic clinical condition.
Contributing causes of depression include genetic predisposition, social and environmental factors, and biologic conditions. Some signs of major depression include loss of interest in most activities, depressed mood, weight loss or gain, insomnia or hypersomnia, loss of energy, fatigue, feelings of despair, decreased ability to think or concentrate, and suicidal thoughts. Approximately 66% of all suicides are related to depression. Depressed men, especially older white men, are more likely to commit suicide successfully than depressed women. Antidepressants can mask suicidal tendencies.
The three types of depression are (1) reactive, (2) major, and (3) bipolar affective disorder (previously referred to as manic depression). Reactive depression usually has a sudden onset after a precipitating event (e.g., depression resulting from a loss, such as death of a loved one). The patient knows why he or she is depressed and may call this “the blues.” Usually this type of depression lasts for months. A benzodiazepine agent may be prescribed. Major depression is characterized by loss of interest in work and home, inability to complete tasks, and deep depression (dysphoria). Major depression can be either primary (i.e., not related to other health problems) or secondary to a health problem (e.g., physical or psychiatric disorder or drug use). Antidepressants have been effective in treating major depression. Bipolar affective disorder involves swings between two moods, the manic (euphoric) and the depressive (dysphoria). Lithium (Lithobid) was originally the drug of choice for treating this type of disorder. Other mood stabilizers, such as carbamazepine (Tegretol), valproic acid or divalproex (Depakote, Valproate), and lamotrigine (Lamictal) are also currently first-line drugs of choice for bipolar disorder.
Pathophysiology
There are many theories about the cause of major depression. A common one suggests an insufficient amount of brain monoamine neurotransmitters (norepinephrine, serotonin, perhaps dopamine). It is thought that decreased levels of serotonin permit depression to occur, and decreased levels of norepinephrine cause depression. However, there can be other physiologic causes of depression as well as social and environmental factors.
Herbal Supplements for Depression
St. John’s wort and gingko biloba have been suggested for the management of mild depression. St. John’s wort can decrease reuptake of the neurotransmitters serotonin, norepinephrine, and dopamine. The use of these and many herbal products should be discontinued 1 to 2 weeks before surgery. The patient should check with the health care provider regarding herbal treatments (Herbal Alert 28-1).
Antidepressant Agents
Antidepressants are divided into five groups: (1) tricyclic antidepressants (TCAs), or tricyclics; (2) selective serotonin reuptake inhibitors (SSRIs); (3) serotonin norepinephrine reuptake inhibitors (SNRIs); (4) atypical antidepressants that affect various neurotransmitters; and (5) monoamine oxidase inhibitors (MAOIs). TCAs and MAOIs were marketed in the late 1950s, and many of the SSRIs and atypical antidepressants were available in the 1980s. The SSRIs and SNRIs are popular antidepressants because they do not cause sedation, hypotension, anticholinergic effects, or cardiotoxicity as do many of the TCAs. Users of SSRIs can experience sexual dysfunction, which can be managed. With unpleasant side effects or lack of improvement, the patient is usually changed to another category.
Tricyclic Antidepressants
TCAs are used to treat major depression because they are effective and less expensive than SSRIs and other drugs. Imipramine was the first TCA marketed in the 1950s.
The action of TCAs is to block the uptake of the neurotransmitters norepinephrine and serotonin in the brain. The clinical response of TCAs occurs after 2 to 4 weeks of drug therapy. If there is no improvement after 2 to 4 weeks, the antidepressant is slowly withdrawn and another antidepressant is prescribed. Polydrug therapy, the practice of giving several antidepressants or antipsychotics together, should be avoided if possible because of potential serious side effects.
The effectiveness of TCAs in treating major depression is well documented. This group of drugs elevates mood, increases interest in daily living and activity, and decreases insomnia. For agitated depressed persons, amitriptyline (Elavil), doxepin (Silenor), or trimipramine (Surmontil) may be prescribed, because of their highly sedative effect. Frequently TCAs are given at night to minimize problems caused by their sedative action. When discontinuing TCAs, the drugs should be gradually decreased to avoid withdrawal symptoms such as nausea, vomiting, anxiety, and akathisia. Imipramine hydrochloride (Tofranil) is used for the treatment of enuresis (involuntary discharge of urine during sleep in children).
The TCA drugs include amitriptyline, imipramine, trimipramine, doxepin, desipramine, nortriptyline, and protriptyline. The TCA drugs desipramine and nortriptyline are major metabolites of imipramine and amitriptyline.
Pharmacokinetics
Amitriptyline is strongly protein-bound. The half-life is 10 to 50 hours, and a cumulative drug effect may result. Amitriptyline is primarily excreted in urine.
Pharmacodynamics
Amitriptyline is well absorbed, but antidepressant effects develop slowly over several weeks. The onset of the antidepressant effect of amitriptyline is 1 to 4 weeks, and the peak concentration is 2 to 12 hours. Drug doses are decreased for older patients to reduce side effects.
Side Effects and Adverse Reactions
The TCAs have many side effects: orthostatic hypotension, sedation, anticholinergic effects, cardiotoxicity, and seizures. Rising from a sitting position too rapidly can cause dizziness and lightheadedness, so the patient should be instructed to rise slowly to an upright position to avoid orthostatic hypotension. This group of antidepressants blocks the histamine receptors; thus, sedation is likely to occur initially but decreases with continuous use of the drug. Because TCAs block the cholinergic receptors, they can cause anticholinergic effects such as tachycardia, urinary retention, constipation, dry mouth, and blurred vision. Other side effects of TCAs include allergic reactions (skin rash, pruritus, and petechiae) and sexual dysfunction (impotence and amenorrhea). Most TCAs can cause blood dyscrasias (leukopenia, thrombocytopenia, and agranulocytosis) requiring close monitoring of blood cell counts. Amitriptyline may lead to extrapyramidal symptoms (EPS). Clomipramine may cause neuroleptic malignant syndrome (NMS). Seizure threshold is decreased by TCAs; therefore, patients with seizure disorders may need to have the TCA dose adjusted. The most serious adverse reaction to TCAs is cardiotoxicity, such as dysrhythmias that may result from high doses of the drug. The therapeutic serum range is 100 to 200 ng/mL.
Drug Interactions
Alcohol, hypnotics, sedatives, and barbiturates potentiate central nervous system (CNS) depression when taken with TCAs. Concurrent use of MAOIs with amitriptyline may lead to cardiovascular instability and toxic psychosis. Antithyroid medications taken with amitriptyline may increase the risk of dysrhythmias.
Selective Serotonin Reuptake Inhibitors
SSRIs block the reuptake of serotonin into the nerve terminal of the CNS, thereby enhancing its transmission at the serotonergic synapse. These drugs do not block the uptake of dopamine or norepinephrine, and they do not block cholinergic and alpha1-adrenergic receptors. SSRIs are more commonly used to treat depression than are TCAs. They have fewer side effects than TCAs.
The primary use of SSRIs is for major depressive disorders. They are also effective for treating anxiety disorders such as obsessive-compulsive disorder, panic, phobias, posttraumatic stress disorder, and other forms of anxiety. Fluvoxamine (Luvox) is useful for treating obsessive-compulsive disorder in children and adults. SSRIs have also been used to treat eating disorders and selected drug abuses. Miscellaneous uses for SSRIs include decreasing premenstrual tension syndrome, preventing migraine headaches, and preventing or minimizing aggressive behavior in patients with borderline personality disorder.
The SSRIs include fluoxetine (Prozac), fluvoxamine (Luvox), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), and escitalopram (Lexapro). Fluoxetine (Prozac) has been effective in 50% to 60% of patients who fail to respond to TCA therapy (TCA-refractory depression). Of all of the SSRIs, sertraline (Zoloft) is the most commonly prescribed antidepressant. The U.S. Food and Drug Administration (FDA) approved a weekly fluoxetine dose of 90 mg. However, before taking the weekly dose, the patient should respond to a daily maintenance dose of 20 mg/d without serious effects. It has been reported that there are some side effects to the weekly 90 mg fluoxetine dose.
Note: Many SSRIs have an interaction with grapefruit juice that can lead to possible toxicity. It is recommended that daily intake be limited to 8 ounces of grapefruit juice or one half of a grapefruit.
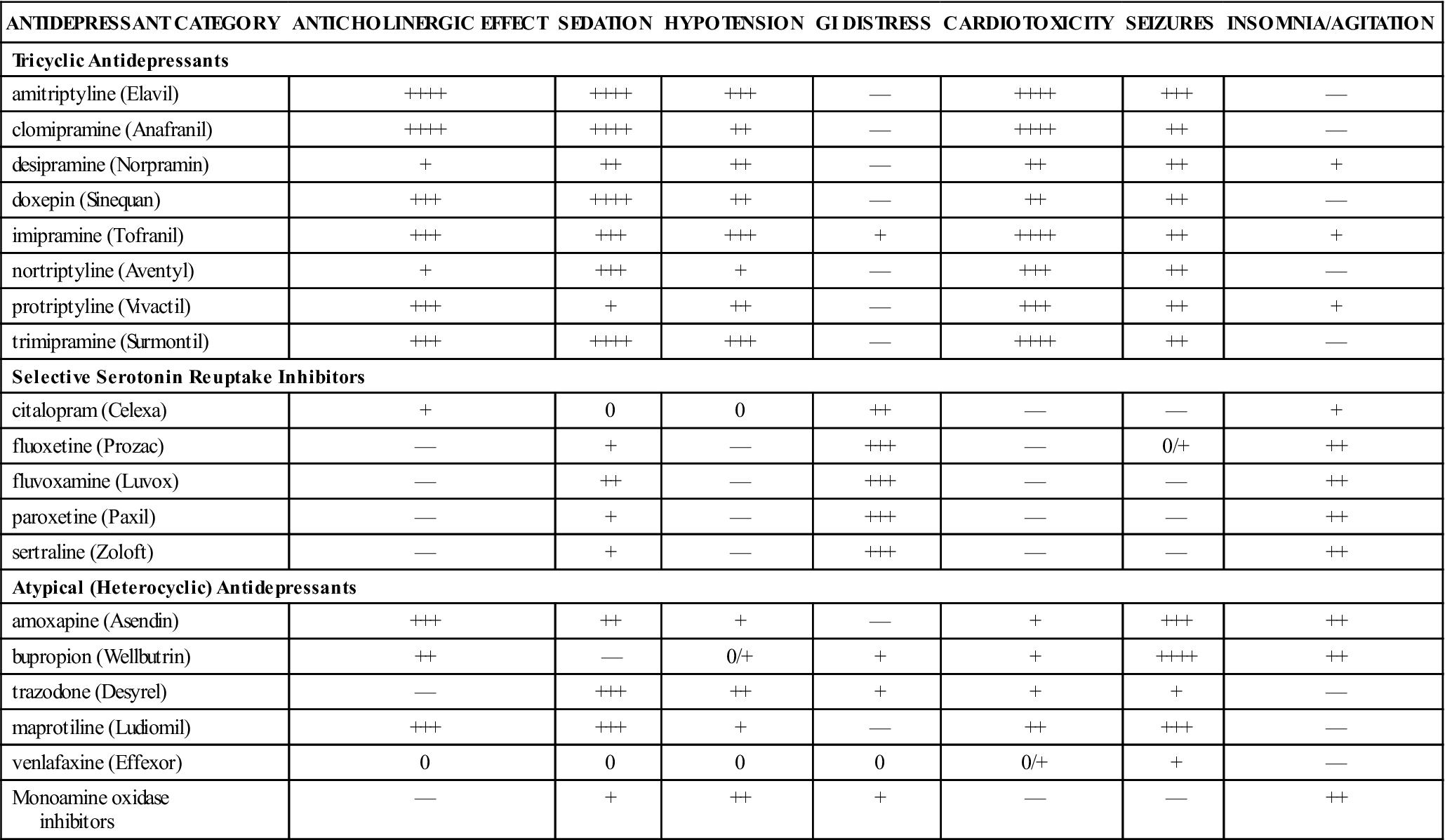
Prototype Drug Chart 28-1 describes the drug characteristics of the SSRI fluoxetine (Prozac). Table 28-1 lists the side effects of the various antidepressants.
TABLE 28-1
SIDE EFFECTS OF ANTIDEPRESSANTS
| ANTIDEPRESSANT CATEGORY | ANTICHOLINERGIC EFFECT | SEDATION | HYPOTENSION | GI DISTRESS | CARDIOTOXICITY | SEIZURES | INSOMNIA/AGITATION |
| Tricyclic Antidepressants | |||||||
| amitriptyline (Elavil) | ++++ | ++++ | +++ | — | ++++ | +++ | — |
| clomipramine (Anafranil) | ++++ | ++++ | ++ | — | ++++ | ++ | — |
| desipramine (Norpramin) | + | ++ | ++ | — | ++ | ++ | + |
| doxepin (Sinequan) | +++ | ++++ | ++ | — | ++ | ++ | — |
| imipramine (Tofranil) | +++ | +++ | +++ | + | ++++ | ++ | + |
| nortriptyline (Aventyl) | + | +++ | + | — | +++ | ++ | — |
| protriptyline (Vivactil) | +++ | + | ++ | — | +++ | ++ | + |
| trimipramine (Surmontil) | +++ | ++++ | +++ | — | ++++ | ++ | — |
| Selective Serotonin Reuptake Inhibitors | |||||||
| citalopram (Celexa) | + | 0 | 0 | ++ | — | — | + |
| fluoxetine (Prozac) | — | + | — | +++ | — | 0/+ | ++ |
| fluvoxamine (Luvox) | — | ++ | — | +++ | — | — | ++ |
| paroxetine (Paxil) | — | + | — | +++ | — | — | ++ |
| sertraline (Zoloft) | — | + | — | +++ | — | — | ++ |
| Atypical (Heterocyclic) Antidepressants | |||||||
| amoxapine (Asendin) | +++ | ++ | + | — | + | +++ | ++ |
| bupropion (Wellbutrin) | ++ | — | 0/+ | + | + | ++++ | ++ |
| trazodone (Desyrel) | — | +++ | ++ | + | + | + | — |
| maprotiline (Ludiomil) | +++ | +++ | + | — | ++ | +++ | — |
| venlafaxine (Effexor) | 0 | 0 | 0 | 0 | 0/+ | + | — |
| Monoamine oxidase inhibitors | — | + | ++ | + | — | — | ++ |
Pharmacokinetics
Fluoxetine is strongly protein-bound. The half-life is 2 to 3 days; therefore a cumulative drug effect may result from long-term use. Fluoxetine is metabolized and excreted by the kidneys.
Pharmacodynamics
Fluoxetine is well absorbed; however, its antidepressant effect develops slowly over several weeks. The onset of fluoxetine’s antidepressant effect is between 1 and 4 weeks, and peak concentration is at 6 to 8 hours after ingestion. The drug dose for older adults should be decreased to reduce side effects.
Side Effects and Adverse Reactions
Fluoxetine produces common side effects such as dry mouth, blurred vision, insomnia, headache, nervousness, anorexia, nausea, diarrhea, and suicidal ideation. Fluoxetine has fewer side effects than amitriptyline (see Table 28-1).
Some patients may experience sexual dysfunction when taking SSRIs. Men have discontinued taking fluoxetine (Prozac) after experiencing a decrease in sexual arousal. Some women have become anorgasmic when taking paroxetine HCl (Paxil). The side effects often decrease or cease over the 2- to 4-week period of waiting for the therapeutic effect to emerge.
Serotonin Norepinephrine Reuptake Inhibitors
Venlafaxine (Effexor) was the first SNRI approved for major depression in 1993. SNRIs inhibit the reuptake of serotonin and norepinephrine, increasing availability in the synapse. SNRIs are used for major depression. Other approved uses are for generalized anxiety disorder and social anxiety disorder. Other SNRIs include duloxetine (Cymbalta) and desvenlafaxine (Pristiq). The concurrent interaction of venlafaxine and St. John’s wort may increase the risk of serotonin syndrome and neuroleptic malignant syndrome. Prototype Drug Chart 28-2 describes the drug characteristics of venlafaxine.
 : 4–6 d
: 4–6 d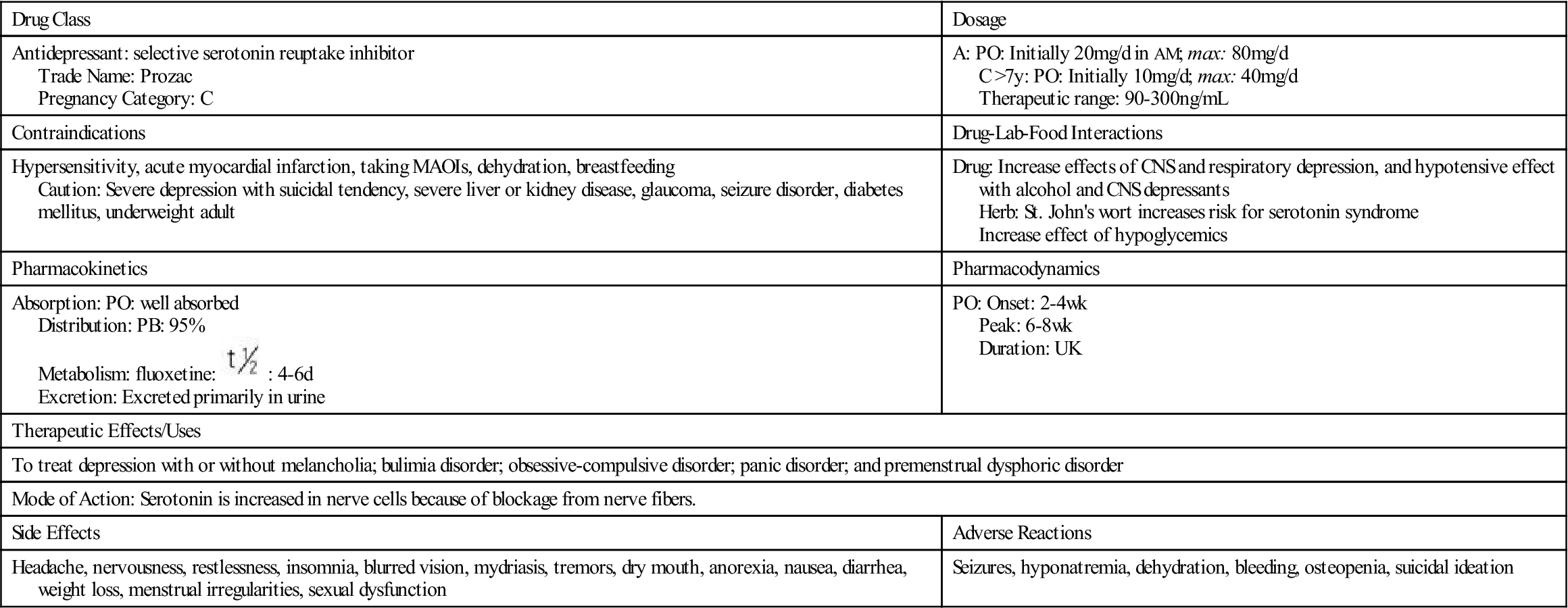
 , half-life; UK, unknown; wk, week.
, half-life; UK, unknown; wk, week. : 5 h
: 5 h


