Wound Care
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe skin tears, circulatory ulcers, and diabetic foot ulcers and the persons at risk.
• Explain how to help prevent skin tears, circulatory ulcers, and diabetic foot ulcers.
• Describe the process and complications of wound healing.
• Describe what to observe about wounds.
• Explain how to secure dressings.
• Explain the rules for applying dressings.
• Explain the purpose of binders and compression garments and how to apply them.
• Describe how to meet the basic needs of persons with wounds.
• Perform the procedure described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
A wound is a break in the skin or mucous membrane. Wounds commonly result from:
• Surgery.
• Trauma—an accident or violent act that injures the skin, mucous membranes, bones, and organs. Falls, vehicle crashes, gunshots, stabbings, bites, burns, and frostbite are examples.
• Unrelieved pressure or friction (Chapter 37).
• Decreased blood flow through the arteries or veins.
Wounds are portals of entry for microbes. Infection is a major threat. Wound care includes preventing infection and further injury to the wound and nearby tissues. Blood loss and pain also are prevented. Box 36-1 describes wound types and causes.
The nurse uses the nursing process to keep the person’s skin healthy. Some agencies have wound therapists or skin care teams to manage all skin problems. The team includes an RN (registered nurse), physical therapist, and dietitian.
See Promoting Safety and Comfort: Wound Care.
Skin Tears
A skin tear is a break or rip in the outer layers of the skin (Fig. 36-8). The epidermis (top skin layer) separates from the underlying tissues (Chapter 10). The skin is “peeled back.” The hands, arms, and lower legs are common sites for skin tears. Very thin and fragile skin is common in older persons. Slight pressure can cause a skin tear.

Causes
Skin tears are caused by:
• Friction, shearing (Chapter 18), pulling, or pressure on the skin.
• Holding an arm or leg too tight.
• Bathing, dressing, and other tasks.
• Pulling buttons and zippers across fragile skin.
• Jewelry—yours or the person’s. Rings, watches, and bracelets are examples.
• Long or jagged fingernails (yours or the person’s) and long or jagged toenails.
Skin tears are painful. They are portals of entry for microbes. Infection is a risk. Tell the nurse at once if you cause or find a skin tear.
Persons at Risk
Persons at risk for skin tears:
See Focus on Children and Older Persons: Persons at Risk (Skin Tears).
Prevention and Treatment
Careful and safe care helps prevent skin tears and further injury. Follow the measures in Box 36-2. Also follow the care plan and the nurse’s directions. They may include dressings (p. 614) and elastic bandages (Chapter 35) to protect the skin and promote healing.
Circulatory Ulcers
Some diseases affect blood flow to and from the legs and feet. Poor circulation can cause pain, open wounds, and edema. Edema is swelling caused by fluid collecting in tissues. Open wounds and poor circulation can lead to infection and gangrene. Gangrene is a condition in which there is death of tissue (Chapter 44).
Circulatory ulcers (vascular ulcers) are open sores on the lower legs or feet. They are caused by decreased blood flow through the arteries or veins. These wounds are painful and hard to heal. Persons with diseases affecting the blood vessels are at risk.
Drugs and treatments are ordered. The nurse uses the nursing process to meet the person’s needs (Box 36-3). You must help prevent skin breakdown on the legs and feet.
Venous Ulcers
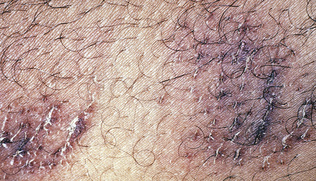
Venous ulcers (stasis ulcers) are open sores on the lower legs or feet caused by poor venous blood flow (Fig. 36-10). Stasis means stopped or slowed fluid flow.

Venous ulcers can develop when valves in the leg veins do not close well. The veins do not pump blood back to the heart in a normal way. Blood and fluid collect in the legs and feet. Small skin veins rupture. This allows hemoglobin to enter the tissues, causing the skin to turn brown. (Hemoglobin gives blood its red color). The skin is dry, leathery, and hard. Itching is common.
The heels and inner part of the ankles are common sites for venous ulcers. They can occur from skin injury. Scratching and trauma are examples.
Venous ulcers are painful and walking is difficult. Fluid may seep from the wound. Infection is a risk. Healing is slow.
Risk Factors.
Risk factors for venous ulcers include:
• History of blood clots (Chapter 35)
• History of varicose veins (Fig. 36-11)
• Obesity
• Surgery: leg, foot, bones, joints
• Phlebitis (inflammation [itis] of a vein [phleb])
Prevention and Treatment.
To prevent venous ulcers:
• Prevent skin breakdown. Follow the measures in Box 36-3.
• Prevent injury. Do not bump the legs and feet.
Persons at risk need professional foot care. Attention is given to toenails, corns, calluses, and other toe and foot problems. You do not cut the toenails of persons with diseases affecting circulation.
Venous ulcers are hard to heal. The doctor may order:
Arterial Ulcers
Arterial ulcers are open wounds on the lower legs or feet caused by poor arterial blood flow. They are found between the toes, on top of the toes, and on the outer side of the ankle (Fig. 36-12). The leg and foot may feel cold and look blue or shiny. The ulcer is very painful.