Urinary Elimination
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe the rules for normal urination.
• Identify the observations to report to the nurse.
• Describe urinary incontinence and the care required.
• Describe bladder training methods.
• Perform the procedures described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
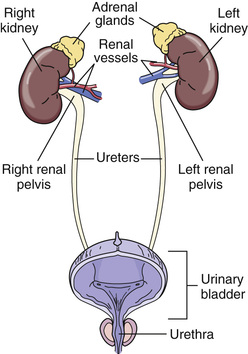
Eliminating waste is a physical need. The digestive system rids the body of solid wastes. The lungs remove carbon dioxide. Sweat contains water and other substances. Blood contains waste products from body cells burning food for energy. The urinary system removes waste products from the blood. It also maintains the body’s water and electrolyte balance.
See Body Structure and Function Review: The Urinary System.
See Promoting Safety and Comfort: Urinary Elimination.
Normal Urination
The healthy adult produces 1500 mL (milliliters) or 3 pints of urine a day. Many factors affect urine production—age, disease, the amount and kinds of fluid ingested, salt, body temperature, perspiration (sweating), and some drugs. Some substances increase urine production—coffee, tea, alcohol, and some drugs. A diet high in salt causes the body to retain water. So do some drugs. When water is retained, less urine is produced.
Urination (micturition and voiding) means the process of emptying urine from the bladder. The amount of fluid intake, habits, and available toilet facilities affect frequency. So do activity, work, and illness. People usually void at bedtime, after sleep, and before meals. Some people void every 2 to 3 hours. Voiding at night disturbs sleep.
Some persons need help getting to the bathroom. Others use bedpans, urinals, or commodes. Follow the rules in Box 24-1 and the person’s care plan.
See Focus on Communication: Normal Urination, p. 390.
See Focus on Children and Older Persons: Normal Urination, p. 390.
See Teamwork and Time Management: Normal Urination, p. 390.
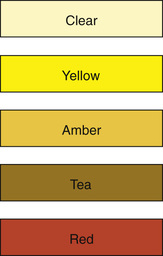
Observations
Normal urine is pale yellow, straw-colored, or amber (Fig. 24-2). It is clear with no particles. A faint odor is normal. Observe urine for color, clarity, odor, amount (output), particles, and blood.
Red food dyes, beets, blackberries, and rhubarb cause red-colored urine. Carrots and sweet potatoes cause bright yellow urine. Certain drugs change urine color. Asparagus causes a urine odor.
Ask the nurse to observe urine that looks or smells abnormal. Report the problems in Table 24-1. The nurse uses the information for the nursing process.
TABLE 24-1
Urinary Elimination Problems
| Problem | Definition | Causes |
| Dysuria | Painful or difficult (dys) urination (uria); burning on urination | Urinary tract infection (UTI), trauma, urinary tract obstruction |
| Hematuria | Blood (hemat) in the urine (uria) | Kidney disease, UTI, trauma |
| Nocturia | Frequent urination (uria) at night (noc) | Excess fluid intake, kidney disease, prostate disease |
| Oliguria | Scant amount (olig) of urine (uria); less than 500 mL in 24 hours | Poor fluid intake, shock, burns, kidney disease, heart failure |
| Polyuria | Abnormally large amounts (poly) of urine (uria) | Drugs, excess fluid intake, diabetes, hormone imbalance |
| Urinary frequency | Voiding at frequent intervals | Excess fluid intake, UTI, pressure on the bladder, drugs |
| Urinary incontinence | The involuntary loss or leakage of urine | Trauma, disease, UTI, reproductive or urinary tract surgeries, aging, fecal impaction, constipation, not getting to the bathroom in time |
| Urinary retention | The inability to void | Prostate problems, nerve damage, UTI, drugs, surgery, kidney stones, constipation, trauma |
| Urinary urgency | The need to void at once | UTI, fear of incontinence, full bladder, stress |
 Bedpans
Bedpans
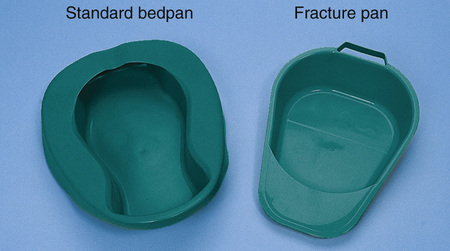
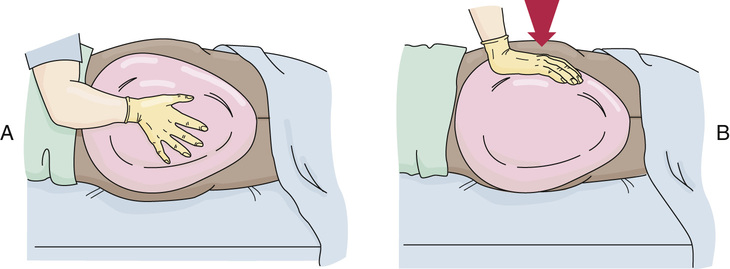
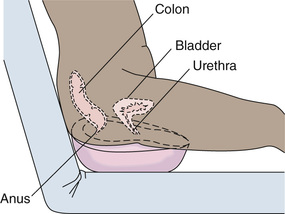
Bedpans are used by persons who cannot be out of bed. Women use bedpans for voiding and bowel movements (BMs). Men use them for BMs.
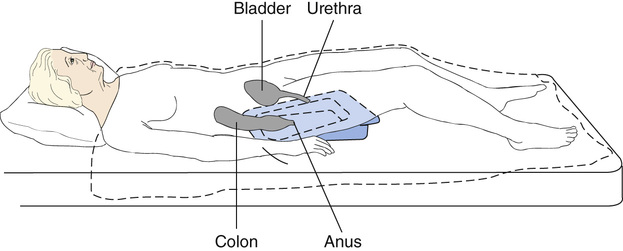
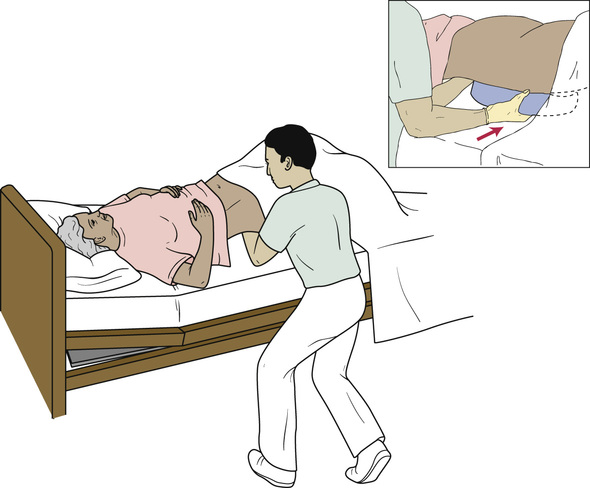
The standard bedpan is shown in Figure 24-3. The wide rim is placed under the buttocks. A fracture pan has a thin rim. It is only about  -inch deep at one end (see Fig. 24-3). The smaller end (flat end) is placed under the buttocks (Fig. 24-4). Fracture pans are used:
-inch deep at one end (see Fig. 24-3). The smaller end (flat end) is placed under the buttocks (Fig. 24-4). Fracture pans are used:
• By persons with limited back motion
• By older persons with osteoporosis (fragile bones) or arthritis (Chapter 44)
• After spinal cord injury or surgery
Like a fracture pan, the small end (flat end) of a bariatric bedpan is placed under the buttocks (Fig. 24-5). Some have a weight capacity of 1200 pounds.
See Delegation Guidelines: Bedpans.
See Promoting Safety and Comfort: Bedpans.
See procedure: Giving the Bedpan, p. 392.
 Urinals
Urinals
Men use urinals to void (Fig. 24-9, p. 394). Plastic urinals have caps and hook-type handles. The urinal hooks to the bed rail within the man’s reach. He stands to use the urinal if possible. Or he sits on the side of the bed or lies in bed to use it. Some men need support when standing.

After voiding, the urinal cap is closed. This prevents urine spills. Remind men to hang urinals on bed rails and to signal after using them. Remind them not to place urinals on over-bed tables and bedside stands. Over-bed tables are used for eating and as a work surface. Bedside stands are used for personal items and supplies. These surfaces must not be contaminated with urine.
Some beds may not have bed rails. Follow agency policy for where to place urinals.
See Focus on Communication: Urinals, p. 394.
See Delegation Guidelines: Urinals, p. 394.
See Promoting Safety and Comfort: Urinals, p. 394.
See procedure: Giving the Urinal, p. 394.