Nutrition and Fluids
Objectives
• Define the key terms and key abbreviations in this chapter.
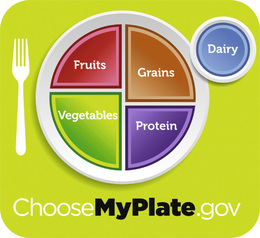
• Explain the purpose and use of the MyPlate symbol.
• Describe the functions and sources of nutrients.
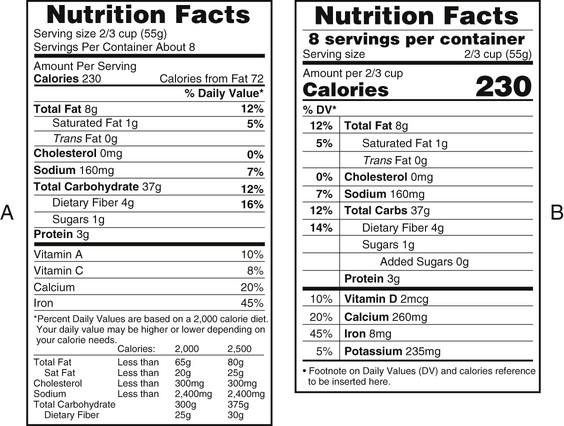
• Explain how to read and use food labels.
• Describe the factors that affect eating and nutrition.
• Describe OBRA requirements for serving food.
• Describe the special diets and between-meal snacks.
• Identify the signs, symptoms, and precautions for aspiration and regurgitation.
• Explain how to assist with measuring food intake.
• Describe fluid requirements and the causes of dehydration.
• Explain how to assist with special fluid orders.
• Explain the purpose of intake and output records.
• Identify what to count as fluid intake and output.
• Explain how to assist with food and fluid needs.
• Explain how to provide drinking water.
• Explain how to prevent foodborne illness.
• Perform the procedures described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Key Abbreviations
| F | Fahrenheit |
| FDA | Food and Drug Administration |
| GI | Gastro-intestinal |
| ID | Identification |
| I&O | Intake and output |
| mg | Milligram |
| mL | Milliliter |
| NPO | Non per os; nothing by mouth |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
| oz | Ounce |
| USDA | United States Department of Agriculture |
Food and water are necessary for life. The person’s diet affects physical and mental well-being and function. A poor diet and poor eating habits:
Eating and drinking provide pleasure. They often are part of social times with family and friends. A friendly, social setting for meals is important. Otherwise, the person may eat poorly.
Many factors affect dietary practices. They include culture, finances, and personal choice. (See Caring About Culture: Meal Time Practices.) Dietary practices also include selecting, preparing, and serving food. The health team includes these factors in planning the person’s nutrition needs.
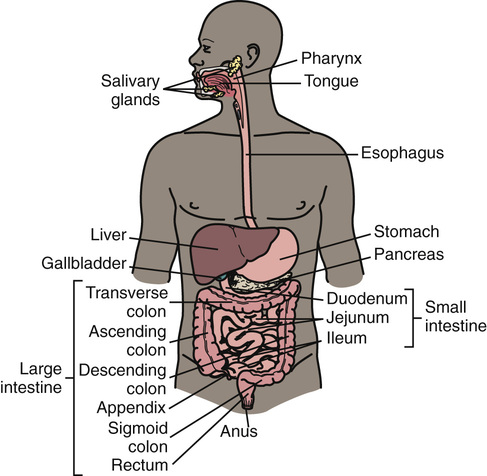
See Body Structure and Function Review: The Digestive System.
See Focus on Long-Term Care and Home Care: Nutrition and Fluids.
See Focus on Surveys: Nutrition and Fluids, p. 444.
Basic Nutrition
Nutrition is the processes involved in the ingestion, digestion, absorption, and use of food and fluids by the body. Good nutrition is needed for growth, healing, and body functions. A well-balanced diet and correct calorie intake are needed. A high-fat, high-calorie diet causes weight gain and obesity. A low-calorie diet promotes weight loss.
Foods and fluids contain nutrients. A nutrient is a substance that is ingested, digested, absorbed, and used by the body. Nutrients are grouped into fats, proteins, carbohydrates, vitamins, minerals, and water (p. 447).
Fats, proteins, and carbohydrates give the body fuel for energy. The amount of energy provided by a nutrient is measured in calories. A calorie is the fuel or energy value of food.
Dietary Guidelines
The Dietary Guidelines for Americans, 2015 is for persons 2 years of age and older. A summary of the most up-to-date Dietary Guidelines can be found on the Evolve Student Resources for this textbook. The Guidelines are also for persons at risk for chronic disease. Certain diseases are linked to poor diet and lack of physical activity. They include cardiovascular disease, hypertension (high blood pressure), diabetes, obesity, osteoporosis, and some cancers. The Dietary Guidelines help people:
The Dietary Guidelines focus on:
MyPlate
The MyPlate symbol (Fig. 27-2) encourages well-balanced meals with foods from 5 food groups. Issued by the United States Department of Agriculture (USDA), MyPlate helps you make wise food choices by:
• Avoiding over-sized portions
• Making half of your plate fruits and vegetables
• Making at least half of your grains whole grains
• Drinking fat-free or low-fat (1%) milk
The amount needed from each food group depends on age, sex, and physical activity (Table 27-1). Activity should be moderate or vigorous (Box 27-1). The USDA recommends that adults do at least 1 of the following.
• 2 hours and 30 minutes each week of moderate physical activity
• 1 hour and 15 minutes each week of vigorous physical activity
Physical activity at least 3 days a week is best. Each activity should be for at least 10 minutes at a time. Adults also should do strengthening activities at least 2 days a week. Push-ups, sit-ups, and weight-lifting are examples.
See Focus on Children and Older Persons: MyPlate.
Grains Group.
Foods made from wheat, rice, oats, cornmeal, barley, or other cereal grains are grain products. Bread, pasta, oatmeal, breakfast cereals, tortillas, and grits are examples.
Grains have these health benefits.
Vegetable Group.
Vegetables can be eaten raw or cooked. They may be fresh, frozen, canned, dried, or juice.
Vegetables have these health benefits.
• May protect against certain cancers. Cancers of the mouth, stomach, and colon-rectum are examples.
• May reduce the risk of kidney stones.
• May reduce the risk of bone loss.
• May help lower calorie intake. Most vegetables are low in fat and calories.
• Contain no cholesterol. (Cholesterol is a soft, waxy substance. It is found in the bloodstream and all body cells. Dietary sources are from animal foods—egg yolks, meat, poultry, shellfish, milk, and milk products.)
• May prevent certain birth defects.
• Contain these nutrients—potassium, dietary fiber, folate (folic acid), vitamins A and C.
Fruit Group.
Any fruit or 100% fruit juice counts as part of the fruit group. Fruits may be fresh, frozen, canned, or dried. Avoid fruits canned in syrup. Syrup contains added sugar. Choose fruits canned in 100% fruit juice or water.
Fruits have these health benefits.
• May protect against certain cancers. Cancers of the mouth, stomach, and colon-rectum are examples.
• May reduce the risk of kidney stones.
• May reduce the risk of bone loss.
• May help prevent constipation.
• May help lower calorie intake. Most fruits are low in fat and calories.
• May prevent certain birth defects.
• Contain these nutrients—potassium, dietary fiber, vitamin C, and folate (folic acid).
Protein Foods Group.
This group includes all foods made from meat, poultry, seafood, eggs, processed soy products, nuts, and seeds. Beans and peas are included in this group as well as the vegetable group.
When selecting foods from this group, remember:
• Using fat for cooking increases the calories. Fried chicken and eggs fried in butter are examples.
• Salmon, trout, and herring are rich in substances that may reduce the risk of heart disease.
• Liver and other organ meats are high in cholesterol.
• Egg yolks are high in cholesterol. Egg whites are cholesterol-free.
Many proteins are high in fat and cholesterol. Heart disease is a major risk. However, this group provides nutrients needed for health and body maintenance.
Oils.
Oils are fats that are liquid at room temperature. Vegetable oils for cooking are examples. They include canola oil, corn oil, and olive oil. Oils come from plants and fish. Because they have nutrients, the USDA includes oils in food patterns. However, oils are not a food group.
Adult women are allowed 5 to 6 teaspoons daily. Adult men are allowed 6 to 7 teaspoons daily. Some foods are high in oil—nuts, olives, some fish, and avocados.
When making oil choices, remember:
Nutrients
No food or food group has every essential nutrient. A well-balanced diet ensures an adequate intake of essential nutrients.
• Vitamins—are needed for certain body functions. The body stores vitamins A, D, E, and K. Vitamins C and the B complex vitamins are not stored. They must be ingested daily. The lack of a certain vitamin results in illness. See Table 27-2.
TABLE 27-2
Common Vitamins
| Vitamin | Major Functions | Sources |
| Vitamin A | Growth; vision; healthy hair, skin, and mucous membranes; resistance to infection | Liver, spinach, green leafy and yellow vegetables, yellow fruits, fish liver oils, egg yolks, butter, cream, whole milk |
| Vitamin B1 (thiamin) | Muscle tone, nerve function, digestion, appetite, normal elimination, carbohydrate use | Pork, fish, poultry, eggs, liver, breads, pastas, cereals, oatmeal, potatoes, peas, beans, soybeans, peanuts |
| Vitamin B2 (riboflavin) | Growth, healthy eyes, protein and carbohydrate metabolism, healthy skin and mucous membranes | Milk and milk products, liver, green leafy vegetables, eggs, breads, cereals |
| Vitamin B3 (niacin) | Protein, fat, and carbohydrate metabolism; nervous system function; appetite; digestive system function | Meat, pork, liver, fish, peanuts, breads and cereals, green vegetables, dairy products |
| Vitamin B12 | Forming red blood cells, protein metabolism, nervous system function | Liver, meats, poultry, fish, eggs, milk, cheese |
| Folate (folic acid) | Forming red blood cells, intestinal function, protein metabolism | Liver, meats, fish, poultry, green leafy vegetables, whole grains |
| Vitamin C (ascorbic acid) | Forming substances that hold tissues together; healthy blood vessels, skin, gums, bones, and teeth; wound healing; preventing bleeding; resistance to infection | Citrus fruits, tomatoes, potatoes, cabbage, strawberries, green vegetables, melons |
| Vitamin D | Absorbing and metabolizing calcium and phosphorus, healthy bones | Fish liver oils, milk, butter, liver, exposure to sun light |
| Vitamin E | Normal reproduction, forming red blood cells, muscle function | Vegetable oils, milk, eggs, meats, cereals, green leafy vegetables |
| Vitamin K | Blood clotting | Liver, green leafy vegetables, egg yolks, cheese |
• Minerals—are needed for bone and tooth formation, nerve and muscle function, fluid balance, and other body processes. Foods containing calcium help prevent musculo-skeletal changes. See Table 27-3, p. 448.
TABLE 27-3
Common Minerals
| Mineral | Major Functions | Sources |
| Calcium | Forming teeth and bones, blood clotting, muscle contraction, heart function, nerve function | Milk and milk products, green leafy vegetables, whole grains, egg yolks, dried peas and beans, nuts |
| Phosphorus | Forming bones and teeth; use of proteins, fats, and carbohydrates; nerve and muscle function | Meat, fish, poultry, milk and milk products, nuts, egg yolks, dried peas and beans |
| Iron | Allows red blood cells to carry oxygen | Liver, meat, eggs, green leafy vegetables, breads and cereals, dried peas and beans, nuts |
| Iodine | Thyroid gland function, growth, metabolism | Iodized salt, seafood, shellfish |
| Sodium | Fluid balance, nerve and muscle function | Almost all foods |
| Potassium | Nerve function, muscle contraction, heart function | Fruits, vegetables, cereals, meats, dried peas and beans |
Food Labels
Food labels are used to make informed food choices for a healthy diet (Fig. 27-3). Food labels contain information about:
• Serving size and the number of servings in each package.
• Calories. The number of servings eaten determines the number of calories of that food.
How a serving fits into the daily diet is called the Daily Value (DV). The DV is a percent (%). The percent is based on 2000 calories daily. The % DV helps you decide if a food is high or low in a nutrient. According to the Food and Drug Administration (FDA), a 5% DV is low. A DV of 20% or more is high.
Meeting Nutritional Needs
A team approach is needed to meet a person’s nutritional needs. The person, nursing team, doctor, dietitian, speech-language pathologist, and occupational therapist are involved. So is the family if necessary. The person’s likes, dislikes, and life-long habits are part of the nutritional care plan.
See Focus on Long-Term Care and Home Care: Meeting Nutritional Needs.
Factors Affecting Eating and Nutrition
Many factors affect eating and nutrition.
• Culture. Culture influences dietary practices, food choices, and food preparation. Frying, baking, smoking, or roasting food and eating raw food are cultural practices. So is using sauces, herbs, and spices. See Caring About Culture: Food Practices.
• Religion. Selecting, preparing, and eating food often involve religious practices (Box 27-2, p. 450). A person may follow all, some, or none of the dietary practices of his or her faith. Respect the person’s religious practices.
• Appetite. Appetite relates to the desire for food. Aromas and thoughts of food can stimulate the appetite. Loss of appetite (anorexia) can occur. Causes include illness, drugs, anxiety, pain, and depression. Unpleasant sights, thoughts, and smells are other causes.
• Chewing problems. Mouth, teeth, and gum problems can affect chewing. Examples include oral pain, dry or sore mouth, gum disease (Chapter 22), and dentures that fit poorly. Broken, decayed, or missing teeth also affect chewing, especially the meat group.
• Swallowing problems. Stroke; pain; confusion; dry mouth; and diseases of the mouth, throat, and esophagus can affect swallowing. See “The Dysphagia Diet” on p. 454.
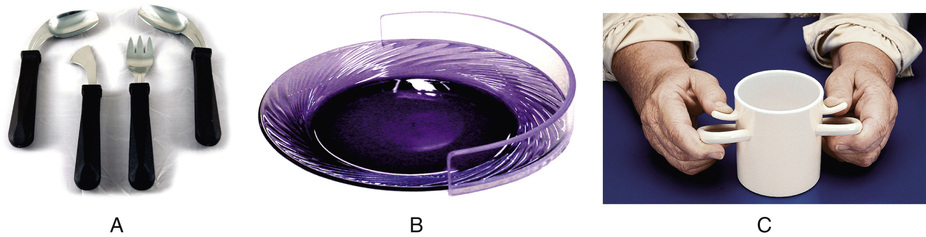
• Disability. Disease or injury can affect the hands, wrists, and arms. Adaptive equipment (assistive devices) let the person eat independently (Fig. 27-4, p. 450). The speech-language pathologist and occupational therapist teach the person how to use them. Make sure each person has needed devices.
See Focus on Children and Older Persons: Factors Affecting Eating and Nutrition, p. 450.
Special Diets
Doctors may order special diets (Table 27-4).
TABLE 27-4
Special Diets
| Diet | Use | Foods Allowed/Restricted |
| Clear liquid—foods liquid at body temperature and that leave small amounts of residue; non-irritating and non-gas forming | After surgery; for acute illness, infection, nausea and vomiting; and to prepare for GI exams | Water, tea, and coffee (without milk or cream); carbonated drinks; gelatin; fruit juices without pulp (apple, grape, cranberry); fat-free broth; hard candy, sugar, and Popsicles |
| Full liquid—foods liquid at room temperature or that melt at body temperature | Advance from clear-liquid diet after surgery; for stomach irritation, fever, nausea, and vomiting; for persons unable to chew, swallow, or digest solid foods | Foods on the clear-liquid diet; custard; eggnog; strained soups; strained fruit and vegetable juices; milk and milk-shakes; cooked cereals; plain ice cream and sherbet; pudding; yogurt |
| Mechanical soft—semi-solid foods that are easily digested | Advance from full-liquid diet; chewing problems, GI disorders, and infections | All liquids; eggs (not fried); broiled, baked, or roasted meat, fish, or poultry that is chopped or shredded; mild cheeses (American, Swiss, cheddar, cream, cottage); strained fruit juices; refined bread (no crust) and crackers; cooked cereal; cooked or pureed vegetables; cooked or canned fruit without skin or seeds; pudding; plain cakes and soft cookies without fruit or nuts |
| Fiber- and residue-restricted—foods that leave a small amount of residue in the colon | Diseases of the colon and diarrhea | Coffee, tea, milk, carbonated drinks, strained fruit and vegetable juices; refined bread and crackers; creamed and refined cereal; rice; cottage and cream cheese; eggs (not fried); plain puddings and cakes; gelatin; custard; sherbet and ice cream; canned or cooked fruit without skin or seeds; potatoes (not fried); strained cooked vegetables; plain pasta; no raw fruits or vegetables |
| High-fiber—foods that increase residue and fiber in the colon to stimulate peristalsis | Constipation and GI disorders | All fruits and vegetables; whole-wheat bread; whole-grain cereals; fried foods; whole-grain rice; milk, cream, butter, and cheese; meats |
| Bland—foods that are non-irritating and low in roughage; foods served at moderate temperatures; no strong spices or condiments | Ulcers, gallbladder disorders, and some intestinal disorders; after abdominal surgery | Lean meats; white bread; creamed and refined cereals; cream or cottage cheese; gelatin; plain puddings, cakes, and cookies; eggs (not fried); butter and cream; canned fruits and vegetables without skin and seeds; strained fruit juices; potatoes (not fried); pastas and rice; strained or soft cooked carrots, peas, beets, spinach, squash, and asparagus tips; creamed soups from allowed vegetables; no fried or spicy foods |
| High-calorie—3000 to 4000 calories daily; includes 3 full meals and between-meal snacks | Weight gain and some thyroid problems | Dietary increases in all foods; large portions of regular diet with 3 between-meal snacks |
| Calorie-controlled—adequate nutrients while controlling calories to promote weight loss and reduce body fat | Weight loss | Foods low in fats and carbohydrates and lean meats; avoid butter, cream, rice, gravies, salad oils, noodles, cakes, pastries, carbonated and alcoholic drinks, candy, potato chips, and similar foods |
| High-iron—foods high in iron | Anemia; after blood loss; for women during the reproductive years | Liver and other organ meats; lean meats; egg yolks; shellfish; dried fruits; dried beans; green leafy vegetables; lima beans; peanut butter; enriched breads and cereals |
| Fat-controlled (low cholesterol)—foods low in fat and prepared without adding fat | Heart, gallbladder, and liver diseases; disorders of fat digestion; diseases of the pancreas | Skim milk (fat-free) or buttermilk; cottage cheese (no other cheeses allowed); gelatin; sherbet; fruit; lean meat, poultry, and fish (baked, broiled, or roasted); fat-free broth; soups made with skim milk (fat-free); margarine; rice, pasta, breads, and cereals; vegetables; potatoes |
| High-protein—aids and promotes tissue healing | Burns, high fever, infection, and some liver diseases | Meat, milk, eggs, cheese, fish, poultry; breads and cereals; green leafy vegetables |
| Sodium-controlled—a certain amount of sodium is allowed | Heart disease, fluid retention, liver diseases, and some kidney diseases | Fruits and vegetables and unsalted butter are allowed; adding salt at the table is not allowed; highly salted foods and foods high in sodium are not allowed; the use of salt during cooking may be restricted |
| Gluten-free—foods without the gluten protein | Celiac disease | Beans; seeds; nuts; eggs; meats, fish, and poultry (without breading, batter, or marinade); fruits and vegetables; most dairy foods; gluten-free grains and starches (arrowroot, corn, cornmeal, hominy, flax, millet, rice, soy, and tapioca); gluten-free flours (rice, soy, corn, potato, bean); no foods containing wheat, barley, triticale, or rye |
| Diabetes meal plan—the same amount of carbohydrates, protein, and fat are eaten at the same time each day | Diabetes | Determined by nutritional and energy requirements |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 cup cooked rice, cereal, or pasta
cup cooked rice, cereal, or pasta cups
cups to 3 cups
to 3 cups to 2 cups
to 2 cups cup dried fruit
cup dried fruit oz natural cheese
oz natural cheese oz
oz to
to  oz
oz cup cooked dry beans
cup cooked dry beans oz nuts or seeds
oz nuts or seeds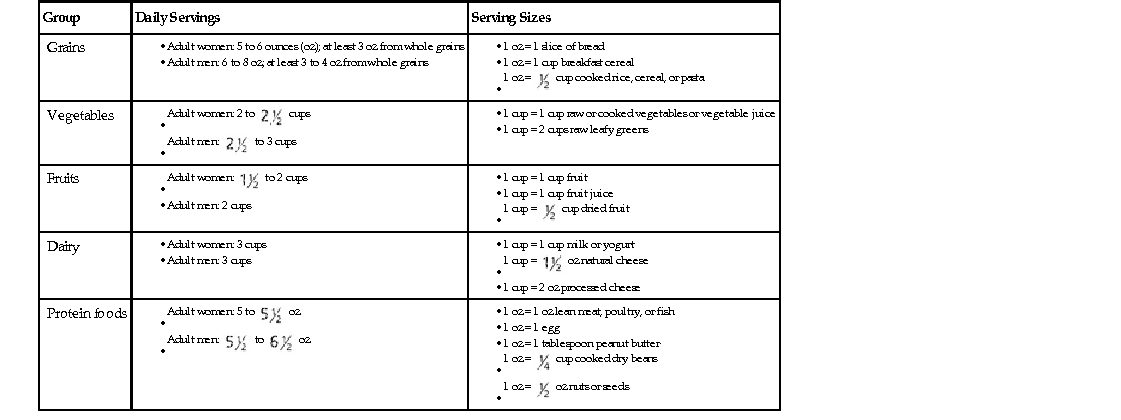
 miles per hour)
miles per hour) miles per hour)
miles per hour)