Oxygen Needs
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe the factors affecting oxygen needs.
• List the signs and symptoms of altered respiratory function.
• Describe the tests for respiratory problems.
• Explain the measures that promote oxygenation.
• Describe the devices used to give oxygen.
• Explain how to safely assist with oxygen therapy.
• Perform the procedures described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Oxygen (O2) is a gas. It has no taste, odor, or color. It is a basic need required for life. Death occurs within minutes if breathing stops. Brain damage and serious illness can occur without enough oxygen. Illness, surgery, and injuries affect the amount of oxygen in the body. Respiratory complications are risks after surgery.
You assist in the care of persons with oxygen needs. You must give safe and effective care.
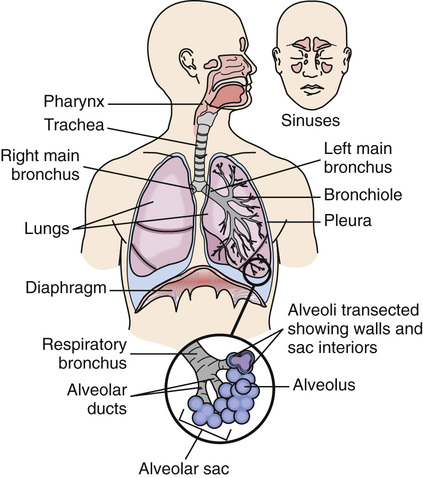
See Body Structure and Function Review: The Respiratory System.
Factors Affecting Oxygen Needs
Any disease, injury, or surgery involving the respiratory or circulatory systems affects the intake and use of O2. Body systems depend on each other. Altered function of any system (for example, the nervous, musculo-skeletal, or urinary system) affects oxygen needs. Oxygen needs are affected by:
Altered Respiratory Function
Respiratory function involves 3 processes. Respiratory function is altered if even 1 process is affected.
• Air moves into and out of the lungs.
• O2 and CO2 are exchanged at the alveoli.
• The blood carries O2 to the cells and removes CO2 from them.
Hypoxia
Hypoxia means that cells do not have enough (hypo) oxygen (oxia). Cells cannot function properly. Anything affecting respiratory function can cause hypoxia. The brain is very sensitive to inadequate O2. Restlessness, dizziness, and disorientation are early signs. Report the signs and symptoms in Box 39-1 at once.
Hypoxia threatens life. All organs need O2 to function. Oxygen is given (p. 651). The cause of hypoxia is treated.
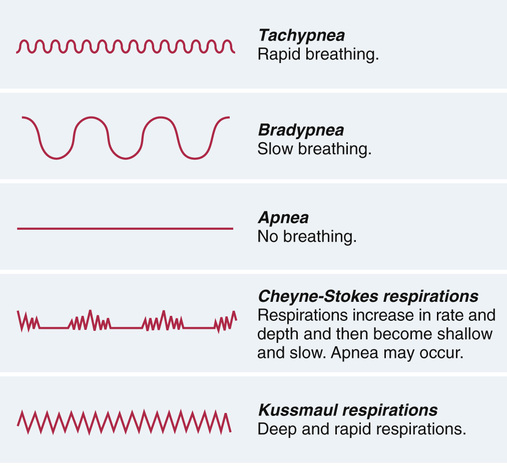
Abnormal Respirations
Adults normally breathe 12 to 20 times per minute. Infants and children have faster rates. Normal respirations are quiet, effortless, and regular. Both sides of the chest rise and fall equally. These breathing patterns are abnormal (Fig. 39-2).
• Apnea—lack or absence (a) of breathing (pnea). It occurs in cardiac arrest and respiratory arrest. Sleep apnea is another type of apnea (Chapter 45).
• Dyspnea—difficult, labored, or painful (dys) breathing (pnea). Heart disease and anxiety are causes.
• Kussmaul respirations—very deep and rapid respirations. They signal diabetic coma.
Respiratory Tests
Respiratory problems may be acute or chronic. Report your observations promptly and accurately (see Box 39-1). The health team must take quick action to meet oxygen needs. The problem must be corrected and prevented from becoming worse.
The doctor may order a chest x-ray to detect lung changes. If necessary, other complex tests are ordered. You may be involved in pulse oximetry and sputum specimens. Assist with other tests as directed by the nurse.
 Pulse Oximetry
Pulse Oximetry
Pulse oximetry measures (metry) the oxygen (oxi) concentration in arterial blood. Oxygen concentration is the amount (percent) of hemoglobin containing O2. An agency may use 1 of these terms.
Measurements are used to prevent and treat hypoxia. The normal range is 95 to 100%. For example, if 97% of all hemoglobin (100%) carries O2, tissues get enough oxygen. If only 90% contains O2, tissues do not get enough oxygen. As low as 85% may be normal for persons with some chronic diseases.
A sensor attaches to a finger, toe, earlobe, nose, or forehead (Fig. 39-3). Light beams on 1 side of the sensor pass through tissues. A detector on the other side measures the amount of light passing through the tissues. With this information, the oximeter measures the O2 concentration.
A good sensor site is needed. Avoid swollen sites and sites with skin breaks. If blood flow to fingers or toes is poor, then the earlobe, nose, and forehead sites are used.
Bright light, nail polish, fake nails, and movements affect measurements.
• Place a towel over the sensor to block bright lights.
• Remove nail polish or use another site.
• Do not use a finger site if there are fake nails.
• Use the earlobe if the person has movements from shivering, seizures, or tremors.
• Do not measure blood pressure on the side of a finger site. Blood pressure cuffs affect blood flow.
Oxygen concentration is often measured with vital signs. The pulse rate may be displayed on the pulse oximeter along with the oxygen concentration. Report and record measurements according to agency policy.
Oximeter alarms are set for continuous monitoring. An alarm sounds if:
See Focus on Children and Older Persons: Pulse Oximetry.
See Delegation Guidelines: Pulse Oximetry, p. 646.
See Promoting Safety and Comfort: Pulse Oximetry, p. 646.
See procedure: Using a Pulse Oximeter, p. 646.