Understanding the Person
Objectives
• Define the key terms in this chapter.
• Identify the parts that make up the whole person.
• Explain how to properly address the person.
• Explain Abraham Maslow’s theory of basic needs.
• Explain how culture and religion influence health and illness.
• Identify the emotional and social effects of illness.
• Describe the persons cared for in health care agencies.
• Identify the elements needed for good communication.
• Describe how to use verbal and nonverbal communication.
• Explain the methods and barriers to good communication.
• Explain how to communicate with persons who have disabilities or who are comatose.
• Explain why family and visitors are important to the person.
• Identify courtesies given to the person, family, and friends.
• Explain how to communicate with persons who have behavior problems.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
The patient or resident is the most important person in the agency. Age, religion, and nationality make each person unique. So do culture, education, occupation, and life-style. Each person is special and has value. The person is treated with respect—as someone who thinks, acts, feels, and makes decisions.
Caring for the Person
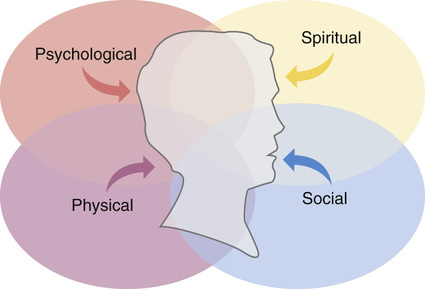
For effective care, you must consider the whole person. Holism means whole. Holism is a concept that considers the whole person. The whole person has physical, social, psychological, and spiritual parts. These parts are woven together and cannot be separated (Fig. 9-1).
Each part relates to and depends on the others. As a social being, a person speaks and communicates with others. Physically, the brain, mouth, tongue, lips, and throat structures must function for speech. Communication is also psychological. It involves thinking and reasoning.
Holistic care involves the whole person. To consider only the physical part is to ignore the person’s ability to think, make decisions, and interact with others. It also ignores the person’s experiences, life-style, culture, religion, joys, sorrows, and needs.
Disability and illness affect the whole person. For example, Mrs. Beal had a stroke. She needs help with physical needs in a nursing center. She had to leave her home. Relationships with her husband and children are changed. She is angry with God for letting this happen to her. The health team plans care to help her deal with her problems.
Addressing the Person
You must know and respect the whole person for effective, quality care. Too often a person is referred to as a room number. For example: “12A needs the bedpan” rather than “Mrs. Brown in 12A needs the bedpan.” This strips the person of his or her identity. It reduces the person to a “thing.”
Patients and residents are not “things.” They are not your family or children. They are complex human beings. To address patients and residents with dignity and respect:
Basic Needs
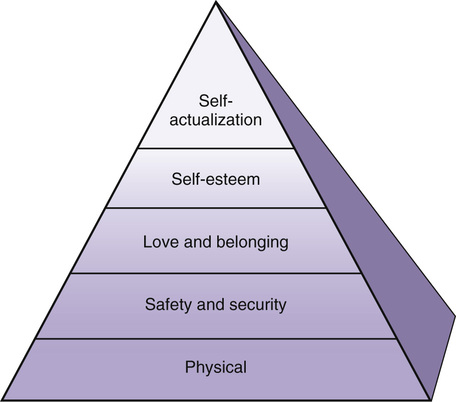
A need is something necessary or desired for maintaining life and mental well-being. According to Abraham Maslow, a famous psychologist, basic needs must be met for a person to survive and function. In this theory, needs are arranged in order of importance (Fig. 9-2). Lower-level needs must be met before higher-level needs. Basic needs, from the lowest level to the highest level, are:
People normally meet their own needs. Disease, injury, or advanced age may prevent them from doing so. Ill or injured persons usually seek health care.
Physical Needs
Oxygen, food, water, elimination, rest, and shelter are needed to live and survive. A person dies within minutes without oxygen. Without food or water, weakness and illness occur within a few hours. The kidneys and intestines must function. If not, poisonous wastes build up in the blood and can cause death. Without enough rest and sleep, a person becomes very tired. Without shelter, the person is exposed to extremes of heat and cold.
Safety and Security Needs
The person needs to feel safe from harm, danger, and fear. Many people are afraid of health care agencies. Some care involves strange equipment. Some care causes pain or discomfort. People feel safe and more secure if they know what will happen. For every task, even a simple bath, the person should know:
See Focus on Long-Term Care and Home Care: Safety and Security Needs, p. 94.
Love and Belonging Needs
Love and belonging needs (emotional needs) relate to love, closeness, and affection. They also involve meaningful relationships with others. Some people become weaker or die from the lack of love and belonging. This is seen in children and in older persons who have out-lived family and friends. Family, friends, and the health team can meet love and belonging needs.
Self-Esteem Needs
Esteem is the worth, value, or opinion one has of a person. Self-esteem means to think well of oneself and to see oneself as useful and having value. People often lack self-esteem when ill, injured, older, or disabled. For example:
• A woman lost her hair from cancer treatments. She does not feel attractive or whole.
• A person has a slow, crippling disease.
You must treat all persons with respect. While it takes more time, encourage them to do as much for themselves as possible. This helps increase self-esteem.
The Need for Self-Actualization
Self-actualization means experiencing one’s potential. It involves learning, understanding, and creating to the limit of a person’s ability. This is the highest need. Rarely, if ever, is it totally met. Most people constantly try to learn and understand more. This need can be postponed and life will continue.
Culture and Religion
Culture is the characteristics of a group of people—language, values, beliefs, habits, likes, dislikes, and customs. They are passed from 1 generation to the next. The person’s culture influences health beliefs and practices. Culture also affects thinking and behavior during illness and when in a hospital or nursing center.
People come from many cultures, races, and nationalities. Their family practices and food choices may differ from yours. So might their hygiene habits and clothing styles. Some speak a foreign language. Some cultures have beliefs about what causes and cures illness. (See Caring About Culture: Health Care Beliefs.) They may perform rituals to rid the body of disease. (See Caring About Culture: Sick Care Practices.) Many cultures have health beliefs and rituals about dying and death (Chapter 55). Culture also is a factor in communication.
Religion relates to spiritual beliefs, needs, and practices. Religions may have beliefs about daily living, behaviors, relationships with others, diet, healing, days of worship, birth and birth control, drugs, and death.
Many people find comfort and strength from religion during illness. They may want to pray and observe religious practices. Hospitals and nursing centers offer religious services. Many have chapels or meditation areas for prayer (Fig. 9-3). Assist the person to attend services as needed. Some residents leave nursing centers to worship.
A person may want to see a cleric (Chapter 1). If so, tell the nurse. Make sure the room is neat and orderly. Have a chair ready for the cleric. Provide privacy during the visit.
The nursing process reflects the person’s culture and religion. The care plan includes the person’s cultural and religious practices.
You must respect the person’s culture and religion. You will meet people from many cultures and religions. Learn about their beliefs and practices. This helps you understand the person and give better care.
A person may not follow all the beliefs and practices of his or her culture or religion. Some people do not practice a religion. Each person is unique. Do not judge the person by your standards. And do not force your ideas on the person.
See Focus on Communication: Culture and Religion.
See Focus on Long-Term Care and Home Care: Culture and Religion.
Effects of Illness and Disability
People do not choose illness or injury. Physical, psychological, and social effects occur. Disabilities may result. A disability is any lost, absent, or impaired physical or mental function. It may be temporary or permanent.
Normal activities—work, driving, fixing meals, yard work, hobbies—may be hard or impossible. Daily activities bring pleasure, worth, and contact with others. People often feel angry, upset, and useless when unable to perform them. These feelings may increase if help is needed with routine functions.
Fears of death, disability, chronic illness, and loss of function are common. Some people explain why they are afraid. Others do not share feelings. Some fear being laughed at for being afraid. A person with a broken leg may fear having a limp or not walking again. Surgery may bring fears of cancer. These feelings are normal and expected. You need to understand the effects of illness and disability. How would you feel and react if you had the person’s problems?
Sometimes recovery is delayed or does not occur. Then the psychological and social effects of illness or disability become greater.
Anger is a common response to illness and disability. Persons needing nursing center care are often angry. They may direct anger at you. However, they are usually angry at the situation. You might have problems dealing with a person’s anger. If so, ask the nurse for help. (See “Behavior Issues,” p. 104.)
You can help the person feel safe, secure, and loved. Take an extra minute to “visit,” to hold a hand, or to give a hug. (Remember to maintain professional boundaries. See Chapter 5.) Show that you are willing to help with personal needs. Respond promptly. Treat each person with respect and dignity.
See Focus on Long-Term Care and Home Care: Effects of Illness and Disability.
Optimal Level of Function
Patients and residents are helped to maintain their optimal level of function. This is the person’s highest potential for mental and physical performance. Encourage the person to be as independent as possible. Always focus on the person’s abilities. Do not focus on disabilities.
Hospital patients are often treated as sick, dependent people. Promoting this “sick role” in a nursing center reduces quality of life. The health team focuses on improving the person’s quality of life. You must help each person regain or maintain as much physical and mental function as possible.
Persons You Will Care For
People are often grouped in health care by their problems, needs, and age.
• Mothers and newborns. Obstetrics is the field of medicine concerned with the care of women during pregnancy, labor, and childbirth and for 6 to 8 weeks after birth (Chapter 52). They receive pre-natal (before birth) care in clinics or doctors’ offices. When labor begins, mothers are admitted to hospital obstetrics (maternity) units. Pregnancy, labor, and childbirth are normal and natural events. However, problems can occur during and after pregnancy and childbirth.
• Children. Pediatrics is the field of medicine concerned with the growth, development, and care of children—newborns to teenagers (usually to age 16). Pediatric units are designed and equipped for the needs of children and parents. The nursing staff meets the child’s physical, safety, and emotional needs (Fig. 9-4).
• Persons having surgery. Care is given before and after surgery (Chapter 35). Surgeries range from simple to very complex. Appendix removal (appendectomy) is a simple surgery. Heart and brain surgeries are complex. Before surgery, the person is prepared for the surgery and for what happens after it. This includes addressing fears and concerns. Needs after surgery relate to relieving pain, preventing complications, and adjusting to body changes.
• Persons with mental health disorders. Psychiatry is the field of medicine concerned with mental health disorders (Chapter 48). Problems vary from mild to severe. Some persons need help coping with life stresses. Others are severely disturbed. They cannot do simple things—eat, bathe, or get dressed. Some persons present dangers to themselves or others. They need special care and treatment.
• Persons needing bariatric care. Bariatrics is the field of medicine focused on the treatment and control of obesity. Obesity is having an excess amount of total body fat. Body weight is 20% or more above what is normal for that person’s height and age. Some people are morbidly obese. (Morbid means diseased.) Morbid obesity means that the person weighs 100 pounds or more over his or her normal weight. Persons with bariatric needs are at risk for many serious health problems. They include heart disease, high blood pressure, stroke, cancer, diabetes, skin problems, and depression. The person has many physical and emotional needs.
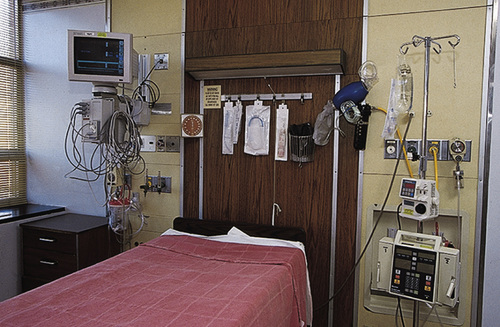
• Persons in special care units. Some people are seriously ill or injured. Special care units are designed to treat and prevent life-threatening problems. They include emergency rooms and intensive care, coronary care, burn, and kidney dialysis units (Fig. 9-5).
• Persons needing sub-acute care or rehabilitation. Some persons need more recovery time than hospital care allows. Others need rehabilitation (Chapter 41). They need to regain functions lost from surgery, illness, or accidents.
• Older persons. Geriatrics is the field of medicine concerned with problems and diseases of old age and older persons. Aging is a normal process (Chapter 12). It is not an illness or disease. Many older persons enjoy good health. Others have acute or chronic illnesses. Body changes normally occur with aging. Social and psychological changes also occur. (See Focus on Long-Term Care and Home Care: Persons You Will Care For.)