The Role of the Nurse in Drug Research
Objectives
• Discuss basic ethical principles.
• Relate the basic ethical principles governing informed consent and risk-to-benefit ratio.
• Describe the objectives of each phase of human clinical experimentation.
• Discuss the role of the nurse in clinical drug trials using the nursing process.
Key Terms
active control, p. 109
autonomy, p. 106
beneficence, p. 106
control group, p. 107
Declaration of Helsinki, p. 107
double-blind, p. 109
experimental group, p. 107
FDA Modernization Act of 1997, p. 108
Good Clinical Practice: Consolidated Guideline, p. 107
informed consent, p. 106
open-label study, p. 109
placebo, p. 109
Prescription Drug User Fee Act, p. 108
single-blind, p. 109
triple-blind, p. 109
veracity, p. 106
In the United States, all prescription drugs must be approved by the U.S. Food and Drug Administration (FDA) before they are made available on the market. Drug studies take place in a variety of inpatient and outpatient settings. Drug research involves risk and is a “high-cost item,” with the estimated average cost to develop each new drug being more than $1 billion.
Drug research and development are complex processes that are of particular interest and importance to professional nursing practice. The nursing process facilitates the integration of cutting-edge research.
This chapter is devoted to a description of basic ethical principles governing informed consent and risk-to-benefit ratio, preclinical testing and human clinical experimentation, and the nurse’s role and nursing process in clinical drug trials.
Basic Ethical Principles
Four basic ethical principles are relevant to research involving human subjects: respect for persons, beneficence, justice, and veracity. These are integral to the issues of informed consent and risk-to-benefit ratio in research involving human beings.
Respect for Persons
Individuals undergoing treatment in any health care system should be treated as independent persons who are capable of making decisions in their own best interests. Individuals whose decision-making capability is diminished are entitled to protection. The nurse can determine this with consistent reassessment of the patient’s cognitive state. Patients should be made aware of the alternatives available to them in their health care, as well as the consequences that stem from those alternatives. The patient’s choice should be honored whenever possible. It is imperative that the nurse recognize when the patient is not capable of rational decision making and therefore entitled to protection.
Autonomy is an integral component of respect for persons. Autonomy is the right to self-determination. In health care settings, health care personnel must respect the patient’s right to make decisions about themselves, even if the decision is not what the personnel want or think is best for the patient. Generally, patients can refuse any and all treatments (right of autonomy) except when the decision poses a threat to others—such as with tuberculosis, when taking medications is legally mandated. Patients have the right to refuse to participate in a research study and may withdraw from studies at any time without penalty of any kind.
Beneficence
Beneficence is the duty to do good and to not harm others, to maximize possible benefits, and to minimize possible harm that might occur in research. It is often not possible to know whether something is beneficial unless it is tested and individuals have been exposed to the risks. A question central to this issue is: Who makes this decision—the patient, or those caring for the patient?
Justice
Justice requires that all people be treated fairly. Expansion of justice includes equal access to health care for all. Justice can be limited when it interferes with the rights of others. The principle of justice, in the context of clinical drug trials, means that social benefits and burdens can be allocated objectively and that those with equivalent circumstances should be treated equally. A challenge to the nurse is the allocation of scarce resources.
Veracity
Veracity requires health care personnel to tell the truth and the whole truth. When there is “bad news” to tell the patient, the health care provider may be reluctant to tell the truth and answer questions honestly. The patient has the right to know the truth, including the bad news.
Informed Consent
Informed consent has its roots in the 1947 Nuremberg Code. The two most relevant aspects of this Code are the participant’s right to be informed and the fact that participation is voluntary, without coercion. If the nurse suspects that a patient is being coerced to participate in a study, the nurse is obligated to report this promptly to the party named on the informed consent (the patient should have a copy of the consent for reference). Informed consent has dimensions beyond protection of the individual patient’s choice and includes the following:
1. Promotion of individual autonomy
2. Protection of patients and subjects from harm
3. Avoidance of fraud and duress in health care
4. Encouragement for professionals to be thorough and clear in communicating information
5. Promotion of educated decision making among patients
It is the role of the health care provider, not the nurse, to explain the study to the patient (including what is expected of the patient) and to respond to questions. While giving written consent, the patient must be alert and able to comprehend.
It is the nurse’s role to protect patients from any anticipated harm. The nurse, in collaboration with the health care provider and pharmacist, must be knowledgeable about all aspects of a drug study, including all inclusion and exclusion criteria for participants (Box 10-1).
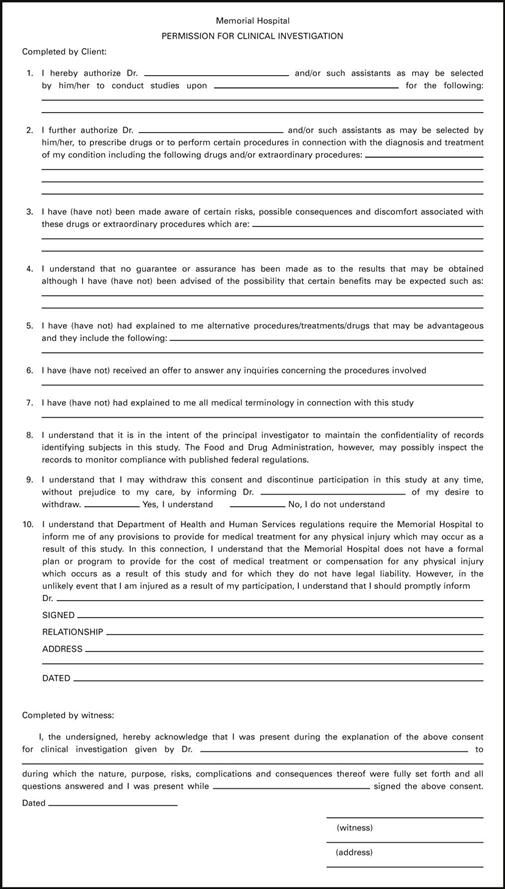
Figure 10-1 shows an example of Permission for Clinical Investigation, and Box 10-2 shows an Informed Consent Checklist.