The Role of the Hematologic System in Oxygen Transport
QUICK LOOK AT THE CHAPTER AHEAD
This chapter will review the roles of the hematologic system in oxygen transport:
Red blood cells and hemoglobin
Laboratory tests of the hematologic system
 CASE STUDY
CASE STUDYWhen Miss D comes into the campus health office, she is moving slowly. She states that she has no energy and just wants to sleep all the time. Miss D is a 20-year-old college student and has been into the office before because of heavy menstrual periods. She is thin, 5 feet 6 inches tall, and weighs 110 pounds. She has been skipping meals because of midterms, drinking diet soda, and eating popcorn in her room. Her blood work comes back with a hematocrit of 31 and a hemoglobin of 8.7.
 INTRODUCTION
INTRODUCTIONOxygen is transported throughout the body by the hematologic or hematopoietic system. This system is composed of blood, plasma, and lymph. Blood is composed of plasma, red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes). The hematologic system has the following three important functions:
♦ Gas exchange (oxygen and carbon dioxide)
♦ Nutrient delivery to the cells
♦ Waste removal from the cells
Additionally, the hematologic system is involved in the acid-base balance, fluid and electrolyte balance, delivery of hormones, protection from foreign organisms, and temperature regulation.
The red blood cell (especially the hemoglobin molecule within the red blood cell) plays a crucial role in oxygen transport. The hemoglobin binds to oxygen in the pulmonary capillaries in the alveolar walls. Hemoglobin transports the oxygen through the arterial system, releasing it at the cellular level. Readily available oxygen allows the cells to create energy
aerobically. Without sufficient oxygen, the cells produce energy anaerobically, creating lactic acid as an end product. Sufficient oxygen for aerobic metabolism is referred to as critical oxygen (O2 crit).
aerobically. Without sufficient oxygen, the cells produce energy anaerobically, creating lactic acid as an end product. Sufficient oxygen for aerobic metabolism is referred to as critical oxygen (O2 crit).
The red blood cell, or erythrocyte, is the most numerous of the formed elements in blood. Red blood cells (RBC) are of particular interest in a text on oxygenation because they carry hemoglobin, the molecule that binds to oxygen during transport. Approximately 98% of oxygen in blood is carried bound to hemoglobin as oxyhemoglobin. RBCs make up about 40% to 50% of the total blood volume. This percentage is referred to as the hematocrit. RBCs are produced in the bone marrow and have a life span of about 120 days. Balanced production and destruction of red blood cells maintains a stable blood count. Every day, 1% of RBCs are produced by the bone marrow, and another 1% are destroyed by phagocytic cells in the liver, spleen, and bone marrow.
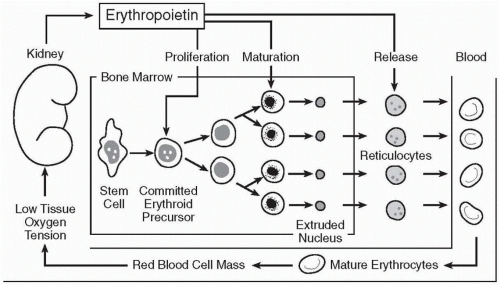
RBCs are released by the bone marrow as reticulocytes (immature RBC) and develop into erythrocytes in the circulating blood within 24 to 48 hours of their release from the bone marrow. The normal percentage of reticulocytes in the circulating blood is 1% to 1.5% of the total RBCs. Abnormally high percentages of reticulocytes may occur during times of rapid RBC production.
The bone marrow is stimulated to produce red blood cells by the hormone erythropoietin (see Figure 8-1). The kidneys produce this hormone when the capillary endothelial cells in the kidney sense hypoxia. Human erythropoietin is now produced using recombinant DNA technology (epoetin alpha). It is used to stimulate bone marrow production in severe anemia that occurs in conditions such as chronic renal failure.
 The bone marrow is stimulated to produce red blood cells by the hormone erythropoietin.
The bone marrow is stimulated to produce red blood cells by the hormone erythropoietin.Hemoglobin is the master transporter of oxygen. It is composed of two pairs of polypeptide chains, each attached to a heme unit. The heme unit is made of iron. If iron stores are low due to nutritional deficiencies, then the red blood cells contain low levels of hemoglobin (iron deficiency anemia). Hemoglobin also contains the red pigment, porphyrin. This pigment combines with oxygen in hemoglobin and gives oxygenated blood the distinctive red color.
Hemoglobin carries the majority of the oxygen to the capillaries, where it moves out of the red blood cell, into the plasma, across the capillary wall, and into the interstitial fluid, becoming available to the cells. Only a small portion (1-2%) of the blood’s oxygen is dissolved in plasma; the rest is bound to hemoglobin. The portion of oxygen that is dissolved in plasma can be measured as the Po2. The oxygen that is combined with hemoglobin is measured as the percent of saturated hemoglobin (So2).
 Only a small portion (1-2%) of the blood’s oxygen is dissolved in plasma, the rest is bound to hemoglobin.
Only a small portion (1-2%) of the blood’s oxygen is dissolved in plasma, the rest is bound to hemoglobin.The hemoglobin-oxygen bond (oxyhemoglobin) is a loose bond that is quickly reversed in the capillaries at the cellular level. Each gram of hemoglobin carries 1.34 mL of oxygen when it is saturated. For oxygen to become available to the cells, the oxyhemoglobin bond must be broken (dissociated). Hemoglobin’s affinity for oxygen or its capacity to bind to oxygen depends on the pH of the blood and the presence of specific enzymes. Hemoglobin binds more strongly to oxygen when the blood is alkaline and releases it more easily when the pH is more
acidic. This relationship or affinity between hemoglobin and oxygen is described in the oxygen-hemoglobin dissociation curve. (Refer to Chapter 2 for more on this topic.) The enzymes 2-3-DPG and G6PD also affect hemoglobin’s affinity for oxygen.
acidic. This relationship or affinity between hemoglobin and oxygen is described in the oxygen-hemoglobin dissociation curve. (Refer to Chapter 2 for more on this topic.) The enzymes 2-3-DPG and G6PD also affect hemoglobin’s affinity for oxygen.
 Each gram of hemoglobin carries 1.34 mL of oxygen when it is saturated.
Each gram of hemoglobin carries 1.34 mL of oxygen when it is saturated. Hemoglobin binds more strongly to oxygen when the blood is alkaline and releases it more easily when the pH is more acidic.
Hemoglobin binds more strongly to oxygen when the blood is alkaline and releases it more easily when the pH is more acidic.Red blood cells and hemoglobin also function to remove carbon dioxide and other waste from the cellular level. Carbon dioxide is a waste product of aerobic metabolism and is transported away from the cells in three ways: dissolved in the plasma as carbon dioxide, attached to hemoglobin (carbaminohemoglobin), and as bicarbonate (HCO–3). Seventy to 80% of the carbon dioxide in the blood is carried as bicarbonate or dissolved in plasma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree