Anatomy and Physiology of the Cardiovascular System
TERMS
blood pressure
cardiac output
sinoatrial node
QUICK LOOK AT THE CHAPTER AHEAD
The cardiovascular and respiratory systems are both integral to oxygenation. The cardiovascular system provides oxygen to the tissues and removes carbon dioxide and waste products. In this chapter, we will review the following:
Anatomy of the cardiovascular system
Processes of circulation and perfusion
Relationships between resistance, pressure, viscosity, and blood flow
Components of blood pressure
 CASE STUDY
CASE STUDYMr. M is a 76-year-old man with newly diagnosed coronary artery disease. In the past, he has had chest pain after overexerting himself. When this happens, he usually stops what he is doing, sits down, and the pain subsides in a few minutes. Today, he wants to know why he still has chest pain even after sitting down for an hour.
 INTRODUCTION
INTRODUCTIONAlthough the respiratory system provides oxygen to the body, it is the cardiovascular system that moves the oxygen to the cells and removes carbon dioxide. The heart works as a pump to move oxygenated blood throughout the arterial system and returns deoxygenated blood to the heart and lungs via the venous system. This process of pumping and circulating is called perfusion, and without it the other processes—ventilation and diffusion—would not provide oxygen to the cells.
The cardiovascular system is composed of two parts: a heart that pumps the blood and the vascular network through which blood is channeled. The vascular network consists of arteries and veins. The arteries carry blood away from the heart, and the veins return blood to the heart. In this chapter, the heart and the components of the vascular network will be discussed as they pertain to the process of oxygenation.
 THE HEART
THE HEARTThe heart is an amazing organ and the cardiovascular system could not function without it. Although the heart is small, about the size of a clenched fist in an adult, it can pump 100,000 times a day. The heart rate can change depending on the needs of the body. The heart rate and cardiac output are finely regulated by neural and hormonal mechanisms to ensure oxygenation of the tissues.
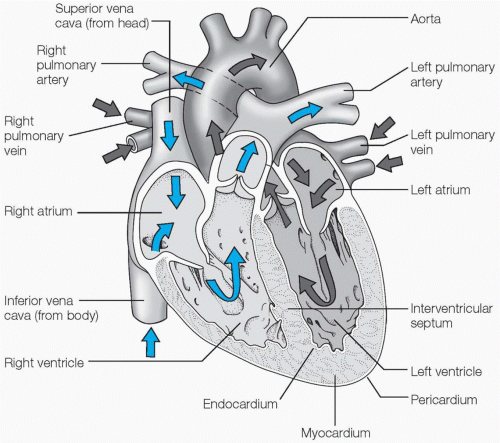
The heart is a muscular organ, lying near the center of the thoracic cavity (see Figure 5-1). It is somewhat anterior in the chest and situated directly behind the sternum. The heart lies
within a pericardial cavity, which is lined by a thin, serous membrane called the pericardium. A membrane called the epicardium surrounds the heart itself. Pericardial fluid is the lubricant between the pericardium and the epicardium. There is only about 10 cc of pericardial fluid, but it reduces friction between the surfaces of the two membranes.
within a pericardial cavity, which is lined by a thin, serous membrane called the pericardium. A membrane called the epicardium surrounds the heart itself. Pericardial fluid is the lubricant between the pericardium and the epicardium. There is only about 10 cc of pericardial fluid, but it reduces friction between the surfaces of the two membranes.
The heart is composed of three layers: the epicardium, the myocardium or cardiac muscle, and the endocardium. The epicardium is one of three layers of the heart that is part of the serous pericardium. The myocardium contracts rhythmically to move blood through the heart, into the pulmonary vasculature, and out again into the systemic vasculature. The endocardium is the lining of the inner surfaces of the heart’s chambers.
The heart is divided into four chambers: the right atrium, the right ventricle, the left atrium, and the left ventricle (see Figure 5-2). The atria serve to collect blood as it returns to the heart, draining it into the ventricles to be pumped into circulation. The atria contract at the end of diastole, providing the “atrial kick”—a 30% increase in blood return to the ventricle that is particularly useful in increasing cardiac output during exertion.
 The atria contract at the end of diastole, providing the “atrial kick”—a 30% increase in blood return to the ventricles, that is particularly useful in increasing cardiac output during exertion.
The atria contract at the end of diastole, providing the “atrial kick”—a 30% increase in blood return to the ventricles, that is particularly useful in increasing cardiac output during exertion.The two cycles of the heart are referred to as diastole and systole. During diastole, the chambers of the heart fill with blood. Systole is the contraction of the heart muscle, expelling blood from the heart into the aorta and
pulmonary artery. Venous blood enters the right atrium from the superior and inferior vena cavae. It flows into the right ventricle and then leaves the right side of the heart via the pulmonary artery. Blood passes through the pulmonary vasculature in the lungs, where gas exchange takes place at the alveolar membrane. Reoxygenated blood returns to the left side of the heart at the left atrium via the pulmonary vein. It moves into the left ventricle and is pushed into the aorta by the contraction of the myocardium, where it begins its journey through the systemic vasculature.
pulmonary artery. Venous blood enters the right atrium from the superior and inferior vena cavae. It flows into the right ventricle and then leaves the right side of the heart via the pulmonary artery. Blood passes through the pulmonary vasculature in the lungs, where gas exchange takes place at the alveolar membrane. Reoxygenated blood returns to the left side of the heart at the left atrium via the pulmonary vein. It moves into the left ventricle and is pushed into the aorta by the contraction of the myocardium, where it begins its journey through the systemic vasculature.
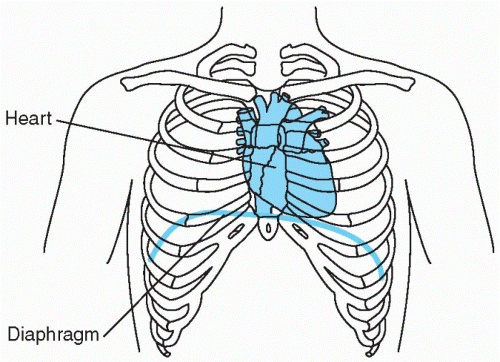 Figure 5-1 Position of the heart in the thoracic cavity. |
Valves control the flow of blood between the atria and ventricles of the heart and some of the blood vessels that are connected to the heart (see Figure 5-3). The valves of the heart alternately open and close to ensure one-way blood flow through the heart. There are four valves in
the heart: the aortic, pulmonic, mitral, and tricuspid valves. There are no valves where the large vessels drain into the atria.
the heart: the aortic, pulmonic, mitral, and tricuspid valves. There are no valves where the large vessels drain into the atria.
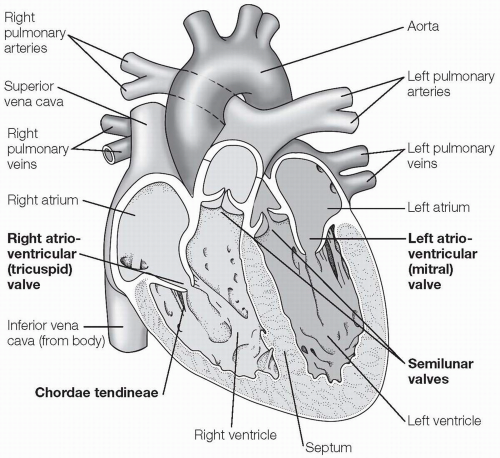 Figure 5-3 The heart valves. A cross section of the heart showing the four chambers and the location of the major vessels and valves. |
Circulation through the heart valves flows in an orderly sequence when the valves are working properly. Blood drains from the superior and inferior vena cavae into the right atrium. It passes the tricuspid valve lying between the right atrium and right ventricle. During systole, the pulmonic valve opens and blood flows from the right ventricle into the pulmonary artery. After a trip through the pulmonary vasculature, reoxygenated blood flows through the pulmonary vein and into the left atrium. It passes through the mitral valve between the left atrium and left ventricle. The final valve that blood passes through as it leaves the heart is the aortic valve, which lies where the left ventricle connects to the aorta. The closing of the heart valves can be heard as heart sounds (the assessment of heart sounds will be reviewed in Chapter 6).
Blood flows from an area of higher pressure to an area of lower pressure. As blood moves from the heart through the circulatory system, it slowly loses pressure. The blood pressure in the aorta is approximately 120/80 mmHg: 120 mmHg being the systolic blood pressure and 80 being the diastolic blood pressure. The mean arterial pressure is the arithmetic mean of the blood pressure in the arterial circulation (between 70 to 100 mmHg). Mean capillary pressure, the arithmetic mean of the blood pressure in the capillary circulation, is approximately 40 mmHg. As blood travels in the venous circulation, the mean pressure is 10 mmHg, and when it reaches the right atrium the pressure is only 2 to 5 mmHg.
 The mean arterial pressure is the arithmetic mean of the blood pressure in the arterial circulation (between 70 to 100 mmHg.)
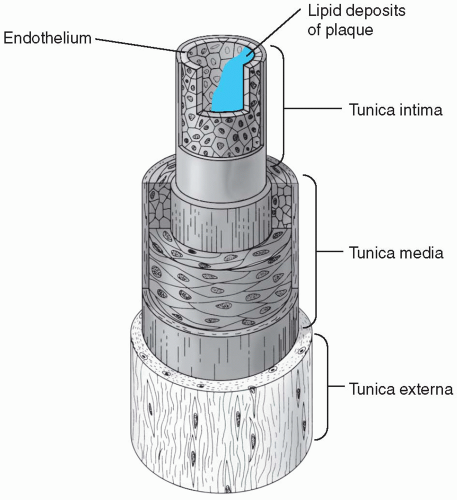
The mean arterial pressure is the arithmetic mean of the blood pressure in the arterial circulation (between 70 to 100 mmHg.)The heart muscles work continuously, requiring oxygen and nutrients just like other tissues. The muscles of the heart are supplied with oxygen by the coronary circulation. The coronary arteries begin at the ascending aorta just past the aortic valve where blood pressure is the highest in the systemic circulation. They branch into smaller arteries to supply different parts of the heart muscle. When coronary arteries are blocked by atherosclerosis or clots, hypoxia occurs in the heart muscle distal to the blockage (see Figure 5-4). Patients with hypoxic cardiac tissues may experience chest pain or angina, especially during exertion. If hypoxia continues and the heart muscle does not receive enough oxygen, part of the myocardium dies. This is called a “heart attack” or myocardial infarction. This part of the heart muscle no longer functions properly. Depending on the location and extent of the tissue death, a myocardial infarction may make the heart incapable of maintaining adequate blood flow and output or impair the conduction system, both potentially life-threatening complications.
 Depending on the location and extent of the tissue death, the myocardial infarction may make the heart incapable of maintaining adequate blood flow and output or impair the conduction system, potentially life-threatening complications.
Depending on the location and extent of the tissue death, the myocardial infarction may make the heart incapable of maintaining adequate blood flow and output or impair the conduction system, potentially life-threatening complications. Patients with hypoxic cardiac tissues may experience chest pain or angina, especially during exertion. If hypoxia continues and the heart muscle does not receive enough oxygen, part of the myocardium dies.
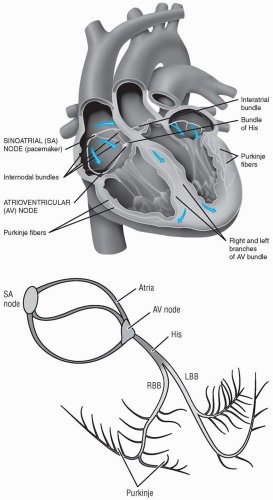
Patients with hypoxic cardiac tissues may experience chest pain or angina, especially during exertion. If hypoxia continues and the heart muscle does not receive enough oxygen, part of the myocardium dies.The myocardium contracts due to an electrical conduction system contained within the muscle walls (see Figure 5-5). This electrical system
stimulates the specialized muscle fibers of the heart to contract. The atria fill and contract first followed by the filling and contraction of the ventricles. In this rhythmic pattern the heart fills and then pushes blood out into the pulmonic and systemic circulation. The conduction system originates in the sinoatrial node in the right atrium. The sinoatrial node (SA node) is considered the “pacemaker of the heart.” The electrical impulse travels down the fibers to the atrioventricular node (AV node) at the base of the right atrium. At least four smaller branches, including Bachmann’s bundle, travel from the right atrium to the left atrium, allowing for synchronized contraction of both atria. At the AV node, the conduction pathway branches into the right and left bundle branches, innervating the ventricles of the heart. Special cells called Purkinje fibers carry the impulses to the myocardial cells of the ventricles. The electrical activity in the heart can be recorded on an electrocardiogram (EKG). The EKG is used to represent
the mechanical activity of the heart during the cardiac cycle (the use of the EKG in the assessment of the heart will be reviewed in Chapter 6).
stimulates the specialized muscle fibers of the heart to contract. The atria fill and contract first followed by the filling and contraction of the ventricles. In this rhythmic pattern the heart fills and then pushes blood out into the pulmonic and systemic circulation. The conduction system originates in the sinoatrial node in the right atrium. The sinoatrial node (SA node) is considered the “pacemaker of the heart.” The electrical impulse travels down the fibers to the atrioventricular node (AV node) at the base of the right atrium. At least four smaller branches, including Bachmann’s bundle, travel from the right atrium to the left atrium, allowing for synchronized contraction of both atria. At the AV node, the conduction pathway branches into the right and left bundle branches, innervating the ventricles of the heart. Special cells called Purkinje fibers carry the impulses to the myocardial cells of the ventricles. The electrical activity in the heart can be recorded on an electrocardiogram (EKG). The EKG is used to represent
the mechanical activity of the heart during the cardiac cycle (the use of the EKG in the assessment of the heart will be reviewed in Chapter 6).
 The sinoatrial node (SA node) is considered the “pacemaker of the heart.”
The sinoatrial node (SA node) is considered the “pacemaker of the heart.” THE VASCULAR NETWORK
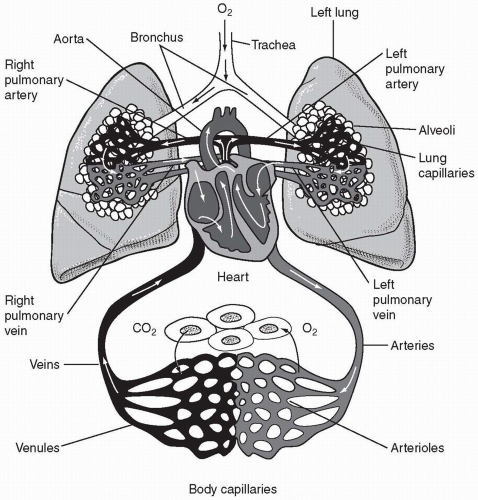
THE VASCULAR NETWORKThe miles and miles of blood vessels that distribute oxygen and nutrients to the cells and remove waste products make up the vascular network. This network can be further divided into two main circuits: the systemic circuit and the pulmonic circuit (see Figure 5-6). The systemic circuit supplies
all the body’s tissues, except the lungs, with blood. The lungs are provided with blood via the pulmonic circuit. Both circuits are made up of a central pump (the heart), and arteries, veins, and capillaries. The pump for the pulmonic system is the right ventricle of the heart, and the pump for the systemic circuit is the left ventricle. Both circuits are connected and dependent on the adequate and equal functioning of the other. The circulatory system is a closed, pressurized system; if
one side of the heart fails, then the other side is affected. For example, if a patient is in a right-sided heart failure, then blood backs up in the venous vasculature. Or, in the case of left-sided heart failure, blood will accumulate in the pulmonary vasculature with resulting pulmonary edema.
all the body’s tissues, except the lungs, with blood. The lungs are provided with blood via the pulmonic circuit. Both circuits are made up of a central pump (the heart), and arteries, veins, and capillaries. The pump for the pulmonic system is the right ventricle of the heart, and the pump for the systemic circuit is the left ventricle. Both circuits are connected and dependent on the adequate and equal functioning of the other. The circulatory system is a closed, pressurized system; if
one side of the heart fails, then the other side is affected. For example, if a patient is in a right-sided heart failure, then blood backs up in the venous vasculature. Or, in the case of left-sided heart failure, blood will accumulate in the pulmonary vasculature with resulting pulmonary edema.
 There are two main circuits of circulation: the systemic circuit and the pulmonic circuit. The systemic circuit supplies all the body’s tissues, except the lungs, with blood. The lungs are provided with blood via the pulmonic circuit. The pump for the pulmonic system is the right ventricle of the heart, and the pump for the systemic circuit is the left ventricle.
There are two main circuits of circulation: the systemic circuit and the pulmonic circuit. The systemic circuit supplies all the body’s tissues, except the lungs, with blood. The lungs are provided with blood via the pulmonic circuit. The pump for the pulmonic system is the right ventricle of the heart, and the pump for the systemic circuit is the left ventricle.The Arterial System
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree