The Person’s Unit
Objectives
• Define the key terms and key abbreviations in this chapter.
• Explain how to maintain the person’s unit.
• Describe how to control temperature and drafts, odors, noise, and lighting for the person’s comfort.
• Describe the basic bed positions.
• Identify the 7 hospital bed system entrapment zones.
• Identify the persons at risk for bed entrapment.
• Explain how to use the furniture and equipment in the person’s unit.
• Describe how a bathroom is equipped for the person’s use.
• Describe how to promote safety, privacy, and comfort in the person’s unit.
• Describe OBRA and CMS requirements for resident rooms.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
The person’s unit is the personal space, furniture, and equipment provided for the person by the agency (Fig. 20-1). The person’s unit is designed to provide comfort, safety, and privacy.

A private room has 1 patient or resident unit. Semi-private rooms have 2 units. Some rooms have 3 or 4 units.
You need to keep the person’s unit clean, neat, safe, and comfortable. See Box 20-1, p. 304.
See Focus on Long-Term Care and Home Care: The Person’s Unit, p. 304.
Comfort
Age, illness, and activity affect comfort. So do temperature, ventilation, noise, odors, and lighting. These factors are controlled to meet the person’s needs.
See Focus on Communication: Comfort.
Temperature and Ventilation
Most healthy people are comfortable with room temperatures between 68°F (Fahrenheit) and 74°F. This range may be too hot or too cold for others. Persons who are older or ill may need higher temperatures for comfort.
Less active persons usually do not like cool areas. Nor do those needing help to move about. They need warm clothing and room temperatures. You may find the rooms rather warm.
Stale room air and lingering odors affect comfort and rest. Ventilation systems provide fresh air and move room air. Drafts occur as air moves. Infants, older persons, and those who are ill are sensitive to drafts. To protect them from drafts:
• Have them wear the correct clothing.
• Have them wear enough clothing.
• Offer lap robes to those in chairs and wheelchairs. Lap robes cover the legs.
• Provide enough blankets for warmth.
• Cover them with bath blankets when giving care.
See Focus on Children and Older Persons: Temperature and Ventilation.
Odors
Odors occur in health care settings and in home care. Food aromas and flower scents are pleasant. Bowel movements and urine have embarrassing odors. So do draining wounds and vomitus. Body, breath, and smoke odors may offend others.
Some people are very sensitive to odors. They may become nauseated. Good nursing care, ventilation, and housekeeping practices help prevent odors. To reduce odors:
• Empty, clean, and disinfect bedpans, urinals, commodes, and kidney basins promptly.
• Make sure toilets are flushed.
• Check incontinent persons often (Chapters 24 and 26).
• Clean persons who are wet or soiled from urine, feces, vomitus, or wound drainage.
• Change wet or soiled linens and clothing promptly.
• Keep laundry containers closed.
• Follow agency policy for wet or soiled linens and clothing.
• Dispose of incontinence and ostomy products promptly (Chapters 24 and 26).
• Provide good hygiene to prevent body and breath odors (Chapter 22).
Smoke odors present special problems. If you smoke, follow the agency’s policy. Practice hand-washing after smoking. Practice hand-washing after handling smoking materials and before giving care. Give careful attention to your uniform, hair, and breath because of smoke odors.
Noise
According to the CMS, a “comfortable” sound level:
Common health care sounds may disturb some persons. Examples include:
• The clanging and clattering of equipment, dishes, and meal trays
• Loud voices, TVs, radios, music players, and so on
• Intercom systems and call lights
• Equipment or wheels needing repair or oil
Loud talking and laughter in hallways and at the nurses’ station are common. Patients and residents may think that the staff are talking and laughing about them.
People want to know the cause and meaning of new sounds. This relates to safety and security needs. Some sounds seem dangerous, frightening, or irritating. Patients and residents may become upset, anxious, and uncomfortable. What is noise to 1 person may not be noise to another. For example, some people enjoy loud music. It disturbs others.
Health care agencies are designed to reduce noise. Window coverings, carpets, and acoustical tiles absorb noise. Plastic items make less noise than metal equipment (bedpans, urinals, wash basins). To decrease noise levels:
See Focus on Communication: Noise, p. 306.
See Focus on Children and Older Persons: Noise, p. 306.
See Focus on Surveys: Noise, p. 306.
Lighting
According to the CMS, comfortable lighting:
• Lets the person control the intensity, location, and direction of light.
• Lets visually impaired persons maintain or increase independent functioning.
Good lighting is needed for safety and comfort. Glares, shadows, and dull lighting can cause falls, headaches, and eyestrain. A bright room is cheerful. Dim light is better for relaxing and rest.
Adjust lighting to meet the person’s changing needs. The over-bed light provides soft, medium, or bright lighting. Ceiling lights provide soft to very bright light. Also adjust window coverings as needed.
Persons with poor vision need bright light. This is very important at meal time and when moving about in the room and agency. Bright lighting also helps the staff perform procedures.
Always keep light controls within the person’s reach. This protects the right to personal choice.
See Focus on Children and Older Persons: Lighting.
Room Furniture and Equipment
Rooms are furnished and equipped to meet basic needs—comfort, sleep, elimination, nutrition, hygiene, and activity. There is equipment to communicate with staff, family, and friends. The right to privacy is considered.
The Bed
Beds have electrical or manual controls. Beds are raised horizontally to give care and to reduce bending and reaching. A low horizontal position lets the person get out of bed with ease (Fig. 20-2). The head and foot of the bed are flat or raised varying degrees.

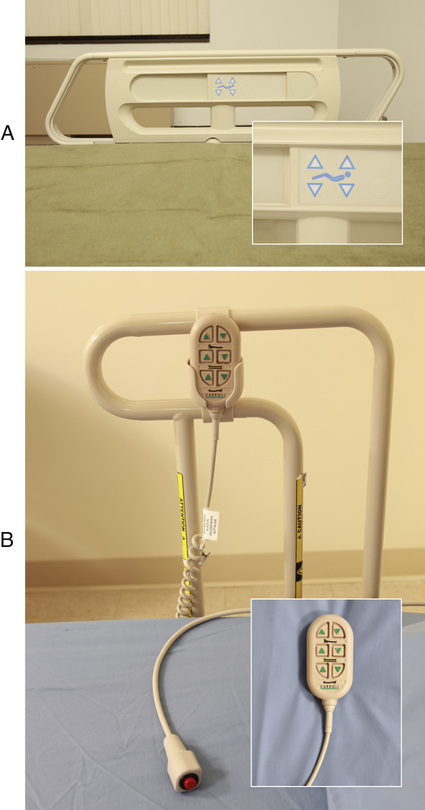
Electric beds are common. Controls are on a side panel, bed rail, or the foot-board (Fig. 20-3, A). Some controls are hand-held devices (Fig. 20-3, B). Patients and residents are taught to use the controls safely. They are warned not to raise the bed to the high position or to adjust the bed to harmful positions. They are told of position limits or restrictions.