The Person Having Surgery
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe the common fears and concerns of surgical patients.
• Describe pre-operative and post-operative care.
• List the signs and symptoms to report after surgery.
• Perform the procedures described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Key Abbreviations
| AE | Anti-embolism; anti-embolic |
| CBC | Complete blood count |
| ECG | Electrocardiogram |
| EKG | Electrocardiogram |
| ID | Identification |
| IV | Intravenous |
| NG | Naso-gastric |
| NPO | Non per os; nothing by mouth |
| OR | Operating room |
| PACU | Post-anesthesia care unit |
| post-op | Post-operative |
| pre-op | Pre-operative |
| SCD | Sequential compression device |
| TED | Thrombo-embolic disease |
The many reasons for surgery include to:
Surgery may require a hospital stay. In-patients are admitted the morning of surgery or 1 or 2 days before surgery. Some patients go to surgery from the emergency room. Patients stay for 1 or more days after surgery.
Same-day surgery (out-patient, 1-day, or ambulatory surgery) is common. The surgeries are done in hospitals and surgi-centers (surgery centers). Surgi-centers are designed and equipped for certain surgical and diagnostic procedures. The person goes home the same day or the next day.
Surgeries are described as:
The person is prepared for what happens before, during, and after surgery. Pre-operative (pre-op) refers to before surgery. Post-operative (post-op) refers to after surgery. Some people recover in nursing centers or rehabilitation centers. Some need home care.
Psychological Care
Surgery causes many fears and concerns (Box 35-1). Past experiences affect feelings. Some persons had surgery before. Others have not. Patients are affected when family and friends talk about their own surgeries. Most people know about tragic events—surgery on the wrong person or body part, instruments left in the body, death during or after surgery. Some people do not share fears and concerns. They may cry, be quiet or withdrawn, or talk about other things. Some pace. Others are very cheerful.
Mental preparation is important. Respect the person’s fears and concerns. Show warmth, sensitivity, and caring.
Patient Information
The doctor explains the need for surgery to the patient and family. They are told about:
• The surgery, risks, and possible complications
• The risks from not having surgery
• The date and time of the surgery
Questions are answered. Misunderstandings are cleared up. Care instructions are given.
After surgery, the doctor talks to the patient and family. Often the health team knows the results before the person.
See Focus on Communication: Patient Information.
Your Role
You can assist in the person’s psychological care before and after surgery.
• Listen. The person may talk about fears and concerns.
• Refer questions to the nurse.
• Explain the care you will give and its need.
• Follow communication rules (Chapters 7 and 9).
• Use verbal and nonverbal communication (Chapter 9).
• Provide care with skill and ease.
• Report signs of fear or anxiety (Chapter 48).
Pre-Operative Care
The pre-operative (pre-op) period may be many days or a few minutes. If time allows, the person is prepared mentally and physically for anesthesia and surgery. The goal is to prevent complications before, during, and after surgery.
See Teamwork and Time Management: Pre-Operative Care.
Pre-Operative Teaching
The nurse explains what to expect before, during, and after surgery. Teaching includes:
• Deep breathing, coughing, and incentive spirometry—are practiced. Post-op, they are done every 1 to 2 hours when the person is awake. See Chapter 39.
• Post-anesthesia care unit (PACU)—commonly called the recovery room, this is where the person wakes up after surgery (Fig. 35-1). The care given is explained.

• Vital signs—are taken often until they are stable.
• Turning and re-positioning—are done at least every 1 to 2 hours post-op.
• Early ambulation—is done as soon as possible post-op.
• Pain—relates to the type and amount of pain to expect and how pain-relief drugs are given.
• Position restrictions—are common after some surgeries. For example, the hip is abducted after hip replacement surgery (Chapter 44).
See Focus on Children and Older Persons: Pre-Operative Care.
Special Tests
Pre-op, the doctor evaluates the person’s health status. These tests are common.
Other tests depend on the person’s condition and surgery. For expected blood loss, the person’s blood is tested for blood type and compatible blood. This is called type and crossmatch.
The person is prepared for the tests as needed. Test results must be on the chart before surgery.
Nutrition and Fluids
A light meal usually is allowed. Then the person is NPO for 6 to 8 hours before surgery. These measures reduce the risk of vomiting and aspiration during anesthesia and after surgery. An NPO sign is placed in the person’s room. The water mug is removed.
Bowel Elimination
Bowel surgeries may require a bowel prep—cleansing the bowel of feces. Feces contain microbes. When the intestine is opened, feces can spill into the sterile abdominal cavity. The bowel prep prevents this contamination.
For the bowel prep, the doctor orders special fluids for the person to drink. Or the doctor orders what enemas to give and when.
Urinary Elimination
The person voids before the nurse gives pre-op drugs. If the person has a catheter, the drainage bag is emptied. The output is measured and recorded.
Often catheters are inserted in the OR. For pelvic and abdominal surgeries, the bladder must be empty. A full bladder is easily injured during surgery. Catheters also allow accurate output measurements during and after surgery.
Personal Care
Personal care before surgery involves:
• Other. Often elastic stockings (p. 598) are put on before transport to the OR. So are sequential compression devices (p. 601).
See Promoting Safety and Comfort: Personal Care.
Jewelry
Jewelry is easily lost or broken in the OR and PACU. Transfers to and from the OR, PACU, and the person’s room also present safety risks. And jewelry can cause pressure injuries (Chapter 37). Therefore all jewelry is removed and stored for safe-keeping. This includes body-piercing jewelry. Record jewelry removal and storage according to agency policy.
The person may want to wear a wedding ring or religious medal. Secure the item in place with gauze and tape according to agency policy. Hand, arm, shoulder, and breast surgeries can cause swelling of the fingers. Wedding rings are removed for such surgeries.
 Skin Preparation
Skin Preparation
Microbes from skin and hair can enter the body through the surgical incision. To reduce the risk of infection, a skin prep is done. For the skin prep, the doctor orders 1 or more of the following.
• Cleansing with an anti-microbial soap. Anti means against.
• Clipping the hair at and around the site.
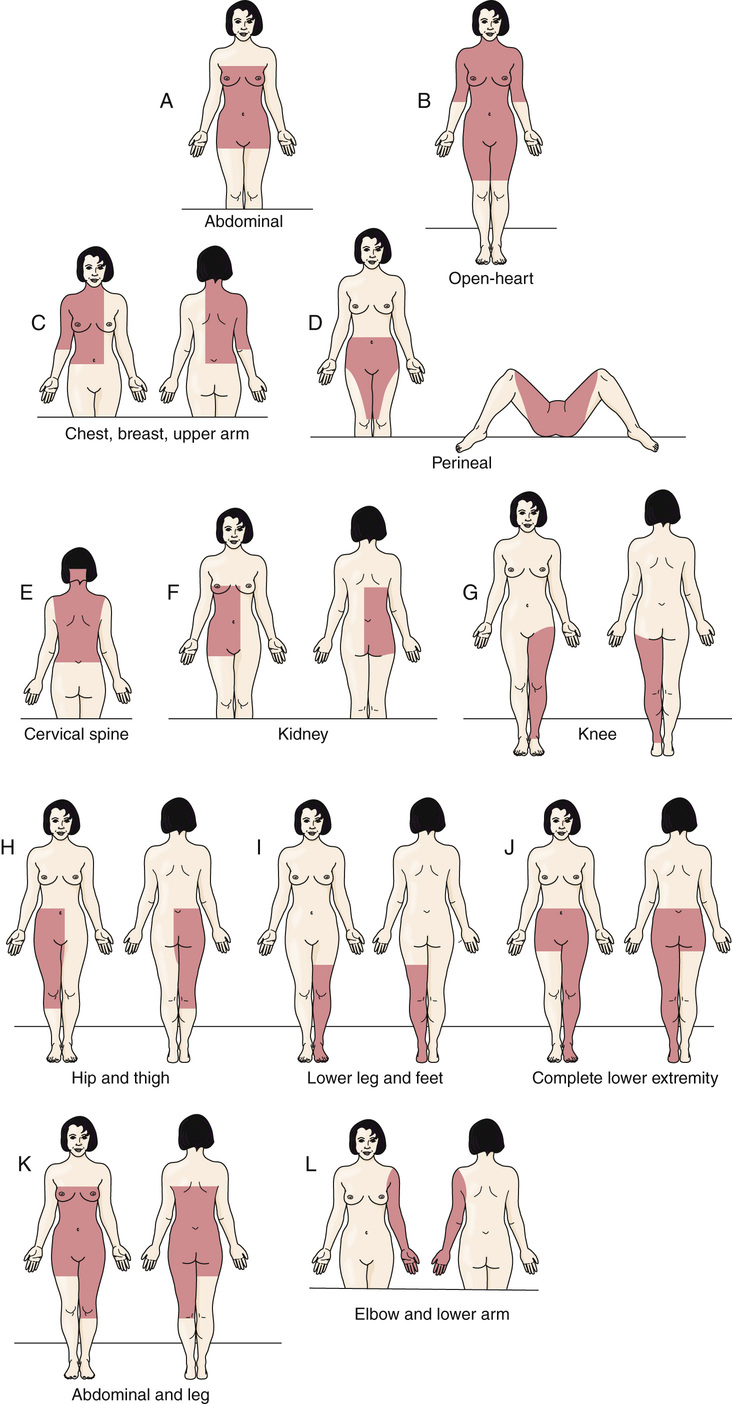
The incision site and a large area around it are prepped (Fig. 35-3, p. 592). The prep is done in the person’s room or in the OR. To remove hair, a hair cream remover is used. Or the skin is shaved.
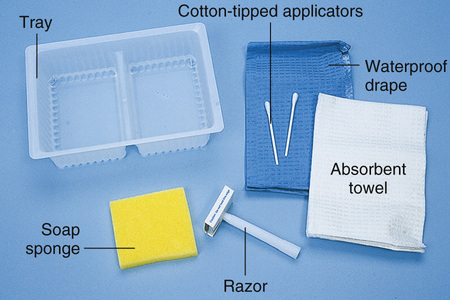
A skin prep kit is used for shaving. The kit has a razor, a sponge filled with soap, a basin (tray), a drape, and a towel (Fig. 35-4, p. 593). Lather the skin with soap. Then shave in the direction of hair growth (Fig. 35-5, p. 593).

See Delegation Guidelines: Skin Preparation, p. 593.
See Promoting Safety and Comfort: Skin Preparation, p. 593.
See procedure: The Surgical Skin Prep—Shaving the Skin, p. 593.