pH
PaCO2
PaO2
HCO3
BE
SaO2
7.32
3.4 kPa
9.5 kPa
22 mmol/L
−4
95%
urine output 40 mls over previous 2 hours (weight 80 kg)
Mobility
Arterial line in right radial artery
Central line in right jugular neck vein
Peripheral cannula left arm
Indwelling urinary catheter
Able to transfer to chair, breathless on walking
Definition of fever
Mary’s temperature has been recorded as 38.6°C via a tympanic thermometer. This is elevated above the normal core body temperature of 37°C in the human, thus supporting a diagnosis of fever (Ryan and Levy 2003). At present there is no clear agreement as to what temperature constitutes a fever however, temperatures of >38°C are generally regarded as clinically significant. The Society of Critical Care Medicine (ISCCM) and the Infectious Disease Society of America (IDSA) have recommended that temperatures of above 38.3°C should be regarded as representative of fever and should trigger a clinical review (O’Grady et al. 1998; Ryan and Levy 2003). Mary’s temperature, at 38.6°C, fulfils the available diagnostic criteria of a clinically significant fever and should therefore prompt further investigation.
Fever is a normal host defence response arising from a number of stimuli, including infections (viral, bacterial or fungal), inflammation (trauma or autoimmune disease) or drug therapy, resulting in an elevation of the temperature set-point (Tset). Fever, as distinguished from hyperthermia, is classified as a controlled or regulated elevation of core body temperature above normal. In this state the hypothalamus is functioning normally and is responding to chemical mediators that stimulate an increase in the temperature set-point (Johnson Rowsey 1997a). It is crucial that fever is distinguished from hyperthermia, as in this state the elevation of body temperature is uncontrolled and arises from damage or failure of the temperature regulatory system, usually following head injury or spinal cord damage (Henker and Carlson 2007; Beard and Day 2008). In fever treatment is aimed at reducing body temperature through the use of antipyretic drugs whereas the management of hyperthermia is aimed at the physical cooling of the patient (Henker et al. 1997; Marik 2000; Beard and Day 2008).
The fever cascade
Mary has been admitted with a community-acquired pneumonia, suggesting that the likely cause of her fever is an infection. Infection involves the entry of microorganisms into the body from the external environment. Invading microorganisms will activate the fever cascade (Johnson Rowsey 1997a) comprising a complex physiological response involving cytokine-mediated temperature elevation (fever), acute phase and immunological stimulation and metabolic and endocrine responses (Plaisance and Mackowiak 2000). Microorganisms (exogenous pyrogens – heat-producing substances) induce monocytes to produce cytokines (endogenous pyrogens) (Ryan and Levy 2003), a group of heat-labile proteins that play a central role in the genesis of fever (Marik 2000). The cytokines known to be active in the development of fever include Interleukin (IL)-I, IL-6, tumour necrosis factor (TNF-α) and the interferons α, β and γ, with interferon being γ the most important of these (Johnson Rowsey 1997a; Marik 2000).
The interaction between cytokines and the exact mechanisms by which they affect neural tissue are complex and as yet are not entirely clear (Johnson Rowsey 1997a; Marik 2000; Ryan and Levy 2003). Cytokines bind to their own specific receptors in an area of the brain lacking the blood brain barrier, possibly the organum vasculosum laminae terminalis (OVLT) which lies in close proximity to the preoptic region of the anterior hypothalamus (Johnson Rowsey 1997a; Ryan and Levy 2003). A cytokine–receptor interaction occurs that activates the chemical phospholipase A2. This liberates arachidonic acid, the substrate necessary for prostaglandin production. Prostaglandins directly modify the activity of thermosensitive neurons in the hypothalamus, raising the temperature set-point to a new setting (Marik 2000), resulting in a fever.
When hypothalamic set-point is raised and fever begins, core blood temperature lags behind and will only equal the new set-point when heat generating mechanisms have been activated. The person experiences the ‘chill stage’ of a fever, which lasts for about 10–40 minutes. During this stage all the physiological mechanisms for heat production and heat conservation are activated (Bruce and Grove 1992). Sympathetic activation, thyroid stimulation and shivering occur to increase basal metabolic rate and raise temperature. Heat loss from convection and radiation is reduced by diverting blood away from the skin surface (see Table 3.2 for definitions of heat loss processes).
Table 3.2 The four physical processes governing heat loss.
| Physical process | Definition | Heat loss in human |
| Radiation | Process of heat loss into the atmosphere from emission of infrared radiation waves. All objects (unless at absolute zero) emit infrared radiation due to molecular collision. | Humans can lose large amounts of heat in this way, particularly when large areas of the body are exposed to the environment |
| Conduction | Process of kinetic heat exchange when one surface is in direct contact with another. | Humans do not lose a great deal of heat from conduction under normal conditions. Conductive heat loss increases significantly in immersion in water, or extended lying on cold surface following fall, unconsciousness etc. |
| Convection | The continuous process of heat loss through air currents. Air molecules are warmed as they come into contact with a warm body. Warm air rises towards the head and is replaced with cool air, which in turn is warmed. | Humans can lose significant amounts of heat via convection. Greatly enhanced by factors such as wind chill and fanning. |
| Evaporation | The process of heat loss from water evaporation. Kinetic heat is produced as a product of cellular metabolism this can be carried in water molecules to the skin surface and evaporated into the atmosphere. | When heat production is high (exercise, fever). Large quantities of heat can be dissipated by sweating in humans to restore heat balance |
Related pathophysiology
Mary is demonstrating the cardinal signs of the chill stage of a fever. She is shivering as her body attempts to generate heat (thermogenesis) through shivering. Sweating ceases during this stage and ‘goose bumps’ (horripilation) appear on the skin, trapping warm air and reducing heat loss from convection and radiation (Bruce and Grove 1992; Johnson Rowsey 1997a). Shivering results in a substantial and costly increase in energy expenditure and may compromise cardiopulmonary function. Shivering should, therefore, be avoided in the critically ill and it is advisable to assist patients to warm themselves during this stage (Holtzclaw 2004).
Mary’s sympathetic nervous system has been activated resulting in the release of the catecholamines, adrenaline and noradrenaline, increasing her heart rate and cardiac contractility and promoting vasoconstriction. An enlarged cardiac output is necessary to supply adequate oxygen to meet increased metabolic demand and there is a corresponding increase in the depth and rate of respirations to augment oxygen availability. A rising metabolic rate creates an initial cellular hypoxia as oxygen demand initially outstrips supply, lowering blood pH and PaO2 levels and stimulating the respiratory centres in the medulla and pons to increase respirations. This would account for Mary’s elevated respiratory rate of 28 breaths per minute and the metabolic acidosis evident in her blood gas analysis. Mary may find it difficult to cope with any increased demand on her respiratory system as she has an existing chest infection. A chest infection will decrease the efficiency of ventilation and decrease Mary’s capacity to compensate for further demand. Mary is also receiving a high percentage of supplemental oxygen to meet present respiratory requirements.
Mary’s skin is pale and feels cool to touch, indicating a noradrenaline-mediated vasoconstriction, and this also accounts for her increased capillary refill time of >2 seconds. Vasoconstriction effectively reduces the volume of blood present at the skin surface, thereby significantly reducing heat loss from convection and radiation and augmenting heat conservation.
During the chill stage of a fever, endocrine responses are also initiated. Sympathetic activation leads to stimulation of the thyroid gland to secrete thyroxines to raise the basal metabolic rate (BMR). An increased BMR promotes thermogenesis and also stimulates appetite, leading to sensations of hunger. Mary at this stage will be using large quantities of energy to maintain a high BMR and because of the substantial increase in energy used when shivering. This will, therefore, have implications for meeting her nutritional requirements.
As sentient beings, humans are also able to invoke behavioural responses to changes in body temperature. Feeling cold may provoke people to add extra clothing or blankets and to take hot food and drinks (see Table 3.3 for a summary of the responses evoked during the chill stage of a fever).
Table 3.3 Mechanisms activated by cold.
| Heat gain | Physical responses: signs and symptoms |
| Shivering – promotes thermogenesis as a result of intense muscular contraction | Generalised, involuntary contraction of skeletal muscles Feels cold Increased energy expenditure |
| Activation of sympathetic activity – release of adrenaline and noradrenaline | Enhanced cardiovascular activity ↑HR,↑RR Vasoconstriction–↑BP |
| Activation of thyroid hormones to increase BMR- thermogenesis | Kinetic heat energy production from nutrient metabolism Hunger |
| Prevention of Heat loss | |
| Horripilation – reduction of heat loss from skin surface via convection, radiation | Goose bumps – cold sensors of skin stimulated, erectile tissue raises hairs on skin of arms, legs |
| Vasoconstriction – prevention of heat loss from convection, radiation at skin surface | Increased capillary refill time Pale skin Cool/cold peripheries Bluish tinge to fingers, nail beds |
| Sentient behaviour or voluntary activity | warmer clothing, blankets, curling up, desire for hot drinks, hot food |
Skills-based knowledge
It is important to bear in mind that fever is a symptom of underlying disease, infection or inflammation and not a disease process in itself. Its presence should prompt investigations to determine its cause so that appropriate, targeted treatment can be commenced in a timely manner (O’Grady et al. 1998). Assessment of Mary at this stage would be focused on establishing the underlying cause of her fever by undertaking a septic screen: blood cultures, swabs and specimens for microbiological culture and sensitivity. Laboratory analysis might also include full blood count (FBC), white cell count (WCC), C-reactive protein (CRP) and procalcitonin (PCT). Ongoing assessment of her temperature should also be undertaken.
Temperature assessment
Temperature taking in clinical practice is often viewed as a relatively straightforward clinical assessment but recent studies reveal evidence of lack of consistency and accuracy in temperature taking (Holtzclaw 1998; Giuliano et al. 1999; Gilbert et al. 2002; Lefrant et al. 2003; Hooper and Andrews 2006; Kimberger et al. 2007; Moran et al. 2007). Errors arise from lack of reliability of temperature taking amongst nurses and health care assistants (Giuliano et al. 1999; Fisk and Arcona 2001; Evans and Kenkre 2006), and inadequate instrument reliability and validity in achieving accurate measurements across the range of temperatures assessed and at temperature-taking sites (Giuliano et al. 1999; Hooper and Andrews 2006; Moran et al. 2007).
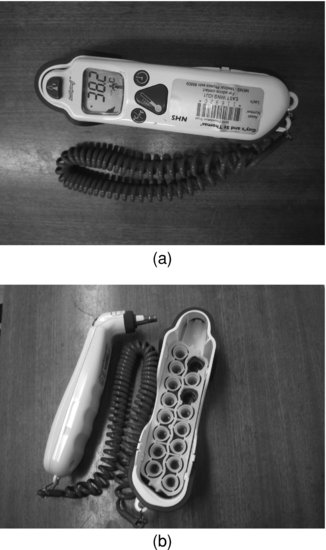
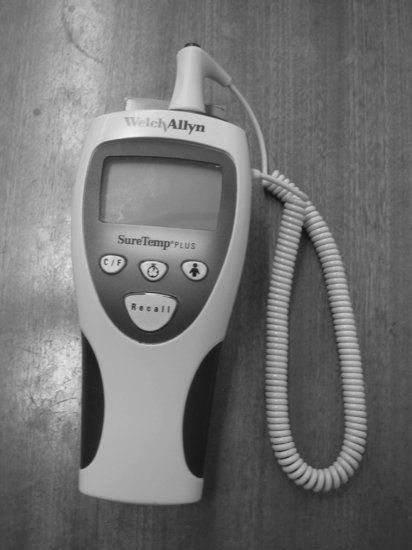
Temperature assessment can be performed invasively or non-invasively. Invasive methods provide direct measurements of core temperature by placement of temperature probes in areas of core blood circulation. Invasive devices, if the equipment is functioning correctly, provide highly accurate and consistent measurements of core temperature. Non-invasive methods only give indications of core temperature by measuring the temperature of arterial blood peripherally. Invasive devices include pulmonary artery thermistor temperature measurement (often referred to as the gold standard as it provides direct measurement of blood temperature in the thoracic cavity), oesophageal or bladder devices. Rectal temperature equates well with core temperature but is considered unpopular for both aesthetic and infection control reasons. Non-invasive methods include oral (via chemical dot or electronic probe), tympanic membrane thermometry (via infrared spectrometry), axillary (via chemical dot or electronic probe) or temporal arterial devices (see Figures 3.1 and 3.2 for examples of non-invasive methods).
To achieve the most accurate temperature assessments, nurses should consider both the best method and the most appropriate site for an individual patient. It is not necessarily imperative that non-invasive temperatures replicate core temperatures exactly but they should reflect these and detect those outside of the normal ranges (hypothermia and fever/hyperthermia) (Erickson 1999).
Mary’s temperature is currently being recorded non-invasively via a tympanic thermometer (Figure 3.1). Non-invasive measurements of shell temperature are more prone to variations due to user ability and may be affected by environmental factors (Gilbert et al. 2002) but placement of an invasive device to record Mary’s temperature at this stage would not be justified. Should very precise and more frequent temperature assessment become necessary, then placement of a urinary catheter with temperature probe or an oesophageal probe might become necessary. At present the use of the tympanic thermometer to measure Mary’s temperature would be in keeping with accepted views of its accuracy and ease of use (Erickson and Kirklin 1993; Leon et al. 2005).
The tympanic membrane is an established site for non-invasive temperature assessment as it is well vascularised and is considered, therefore, to replicate the core temperature of blood in the intracranial cavity (Shinozaki et al. 1988, Erickson and Kirklin 1993). It is also an easily accessible site that can be used to obtain temperatures in a wide range of patients. In addition, tympanic temperatures record relatively quickly and may be viewed as being efficient in terms of nursing time (Erickson and Kirklin 1993; Giuliano et al. 1999).
A number of studies have demonstrated questionable accuracy and reliability of tympanic thermometry (Hooker and Houston 1996; Manian and Greisenauer 1998; Giuliano et al. 1999; Hooper and Andrews 2006; Moran et al. 2007). Hooker and Houston (1996) and Manian and Greisenauer (1998) both found that tympanic thermometers demonstrated a lack of sensitivity and were unable to detect fever in significant numbers of patients.
In the critically ill, Moran et al. (2007) suggest that it compares poorly to invasive pulmonary artery and bladder temperatures, possibly due to a significant alteration in blood flow to the tympanic membrane during critical illness, negating the ability of the thermometer to measure blood temperature accurately. Tympanic temperatures may be affected by cerebral blood flow and could be an inappropriate method for the head-injured patient or where cerebral ischaemia is suspected (Giuliano et al. 1999). The lack of accuracy of tympanic temperatures is further supported by earlier studies where it compared poorly with other invasive and non-invasive methods (Nierman 1991; Fisk and Arcona 2001), although these authors do not speculate as to the possible cause of its poor performance.
Giuliano et al. (1999), Fisk and Arcona (2001), Hooper and Andrews (2006) and Moran et al. (2007) have challenged whether tympanic thermometry is reliable or easy to use. Giuliano et al. (1999) and Fisk and Arcona (2001) highlighted the lack of adequate education and training in the use of tympanic thermometers, resulting in significant operator error even amongst experienced nurses. Giuliano et al. (1999) found that experienced nurses required more than ten minutes of intensive training to obtain an accurate reading. Fisk and Arcona (2001) recommended abandoning the expanded use of tympanic thermometry because it would be prohibitively expensive to provide hospital-wide training to maintain operator reliability. Evans and Kenkre (2006) further point out that the majority of temperature measurements in the acute setting are undertaken by healthcare assistants, who are often the least experienced and most poorly trained.
Oral temperature assessment (Figure 3.2) is a popular alternative to the tympanic method. Doubts have persisted as to the accuracy of oral temperature measurement in the critically ill as readings are thought to be subject to factors such as warmed and humidified oxygen, bradypnoea and oral intubation (Erikson and Kirklin 1993). Recent studies, however, have shown the acceptable performance of both chemical dot and electronic thermometers in intubated patients (Giuliano et al. 1999; Moran and Mendal, 2002; Potter et al. 2003; Hooper and Andrews 2006). Factors such as humidified oxygen and respiratory rates have also been discounted as statistically significant in oral temperature assessment (Hooper and Andrews 2007). Oral electronic thermometers with an appropriate probe cover have performed better than the chemical dot type in critically ill patients (Gilbert et al. 2002; Hooper and Andrews 2007).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree