In view of his profuse bleeding, tachypnoea and decreased oxygen saturations, Mr Smith is electively intubated with a size 8.0 endotracheal tube prior to the insertion of a balloon tamponade tube, pending the arrival of the on-call endoscopy team. To manage his hypovolaemia, two 16-gauge cannulae are inserted in the emergency department and he is given intravenous colloids, whilst awaiting the arrival of cross-matched blood. After stabilisation Mr Smith is transferred to intensive care where a central venous catheter and an arterial line are inserted. Mr Smith receives in total 1 litre of colloid, 3 units of packed red blood cells, 1 unit of fresh frozen plasma (FFP) and one pool of platelets. He is commenced on intravenous terlipressin, omeprazole and antibiotic therapy (Ciprofloxacillin).
Reader activities
Having read this scenario, consider the following:
- What do you consider to be the priorities for the management of Mr Smith on arrival to intensive care?
- What is the optimal level of haemoglobin for this patient?
- What additional complications might be associated with his hypovolaemia?
Pathophysiology of cirrhosis, portal hypertension and oesophageal varices
Liver cirrhosis can occur as a consequence of any chronic liver disease whereby repeated hepatocyte damage results in the formation of fibrous tissue and the development of nodules (cirrhosis) (Sargent 2007).
The natural history of cirrhosis is characterised by an asymptomatic phase (compensated cirrhosis). Over time, as the disease progresses this eventually leads to the ‘decompensated stage’ whereby the development of portal hypertension leads to major complications; hepatic ascites, hepatorenal syndrome, infections, coagulopathy, hepatic encephalopathy and variceal bleeding (Mihas and Sanyal 2006). The Child–Pugh score (Table 6.2) is used to assess the prognosis and appropriate treatment in cirrhosis. Patients with a class C Child–Pugh score are more likely to die from the effects of a variceal bleed compared to Child–Pugh class A (Jalan and Hayes 2000). Based on the data available in Table 6.1, Mr Smith would be categorised as class A.
Table 6.2 The Child–Pugh score.
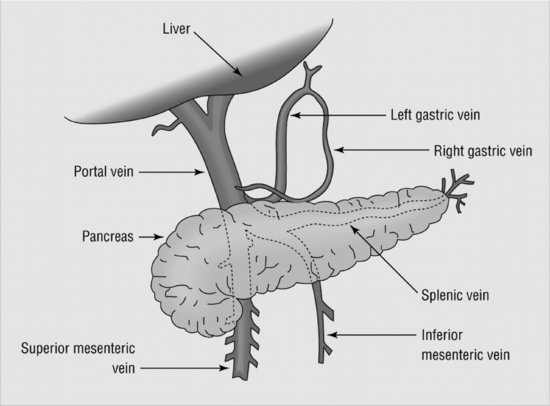
The normal anatomical relations of the liver and hepatic vein and branches are shown in Figure 6.1. The portal vein carries approximately 1.5 litres of blood from the small intestine, spleen and liver at a pressure of 5–10 mmHg (Wong 2009). As the liver becomes cirrhotic, there is an increase in intra-hepatic resistance, thus leading to portal hypertension with portal pressures exceeding 12 mmHg (Krige and Beckingham 2001). This increased pressure opens up a ‘collateral circulation’ whereby for blood flow to return to systemic circulation, portal blood flow needs to divert around the liver, especially the instrinsic veins around the gastro-oesophageal junction. These veins then dilate and become varicosed (varices) (Mihas and Sanyal 2006). These collateral vessels are inelastic and become thinner and more fragile as they enlarge and are at high risk of rupturing (Figure 6.2) (McArdle 1999).
Further information
In intensive care, Mr Smith is closely monitored with no further clinical signs of bleeding. As he continues to remain haemodynamically stable, the balloon tamponade tube is removed and he undergoes an upper gastrointestinal endoscopy, where two grade lll varices are found. These are treated with endoscopic variceal band ligation (EVL). Twenty-four hours later with no further bleeding, Mr Smith is extubated and later transferred to a ward setting.
Figure 6.1 Anatomical relations of portal vein and branches. (Krige 2001). Used with kind permission of the BMJ)
Laboratory tests and investigations
Liver function tests (LFTs) are the first line in diagnosing liver disease. They provide valuable information regarding the liver synthetic function and cellular damage and enable any biliary tree involvement to be identified (Stonesifer 2004). Other immediate investigations that are necessary for patients presenting with an acute variceal haemorrhage are full blood count, clotting screen, blood group and cross match, urea and electrolytes, and blood glucose (Wong 2009). Mr Smith already has an established diagnosis of alcohol-related liver cirrhosis, and therefore, a prior liver disease aetiology screen, liver biopsy and ultrasound to exclude any other causes of liver disease are necessary. Table 6.3 demonstrates Mr Smith’s initial laboratory investigations, normal values and rationale for abnormalities.
Table 6.3 Laboratory results and normal values.
Endoscopic treatment of oesophageal varices
Prior to the initiation of endoscopic therapy, patients need to be cardiovascularly stable, as the process itself poses an additional risk of pulmonary aspiration of inhaled blood. This justifies the need for Mr Smith to be intubated in order to protect his airway prior to endoscopy therapy (Wong 2009).
Endoscopic variceal band ligation (EVL) is the first choice of endoscopic management therapy and should be used unless banding is difficult due to profuse bleeding or it is technically unavailable (Jalan and Hayes 2000; SIGN 2008). Meta-analysis has demonstrated that EVL is superior to sclerotherapy for the control of acute bleeding, and is associated with less adverse events and a decreased mortality (Bosch 2009). EVL uses a specialised suction chamber that is inserted onto the end of an endoscope. At endoscopy the varix is sucked into the chamber and a rubber band applied. As the side effect of EVL is the formation of oesophageal ulceration, protein pump inhibitors (in Mr Smith’s case omeprazole) should be administered post-endoscopic therapy (Wong 2009).
Initial resuscitation and management of active variceal haemorrhage
Acute variceal haemorrhage can be torrential, constituting a medical emergency that may culminate in death if not promptly and properly controlled (Mihas and Sanyal 2006). Initial resuscitation and management of an active variceal haemorrhage should follow the classic ABCDE approach which is described in detail below along with the management of associated complications. There are two distinct phases in the course of variceal bleeding: the acute phase and a later phase in which there is a high risk of secondary bleeding thus necessitating the need for secondary prophylaxis. Only the management of the acute phase is reviewed in this chapter.
Airway
Mr Smith should be continually assessed and receive appropriate management of his airway. Consequently, staff involved in his care should be competent in the recognition of airway compromise and basic airway manoeuvres (SIGN 2008).
Mr Smith initially received 0.6 FiO2 (60%) via a face mask. As his initial oxygen saturations were only 94%, this was increased to 1.0 (100%). Collins (2000) and Bench (2004) recommend that all patients receive 100% oxygen via a non-rebreathe face mask during the acute phase of shock.
Endotracheal intubation is always advocated prior to insertion of a balloon tamponade tube (Figure 6.3) due to the technical difficulties of tube insertion, the inability for patients to clear secretions and the risk of bronchial aspiration. Additional indications for intubation in patients with an acute variceal bleed are uncontrolled bleeding, severe hepatic encephalopathy, inability to maintain oxygen saturations above 90% or aspiration pneumonia (Jalan and Hayes 2000; Bosch 2009).
Figure 6.3 Picture of balloon tamponade tube. (McPherson 2006). Reproduced with kind permission of the BMJ.
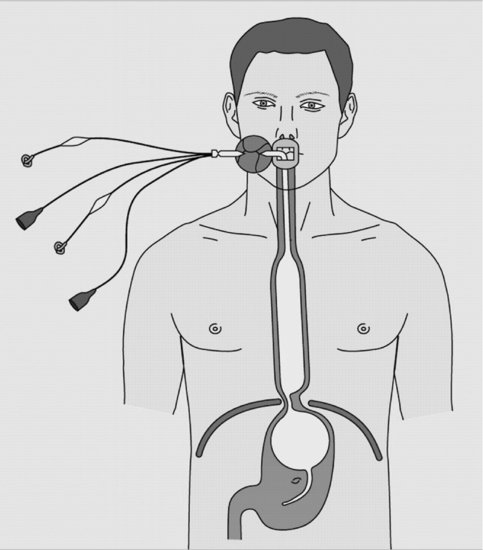
There are three main types of balloon tamponade tube (Sengstaken–Blakemore, Minnesota and Linton–Nachlas) which achieve haemostasis in up to 90% of cases by direct compression by the gastric balloon. However, there is no demonstrated survival benefit associated with their use, and a complication rate of 15–20% (asphyxiation, pneumonia, oesophageal tears, patients discomfort, tube migration and erosion and oesophageal necrosis). Balloon tamponade tubes should therefore only be used in cases of uncontrolled bleeding, or in the case of Mr Smith, where there is a delay in commencing endoscopic therapy (Jalan and Hayes 2000; Mihas and Sanyal 2006; SIGN 2008).
The Sengstaken, Blakemore and Minnesota balloon tamponade tubes (Figure 6.3) all have a gastric and oesophageal balloon. Once the tube is trans-orally positioned by a skilled practitioner, it is, however, rarely necessary to inflate the oesophageal balloon (Wong 2009). After the tube position is confirmed, the gastric balloon is usually inflated with 250 ml of water or a mixture of water and 10% radio opaque contrast (Wong 2009). Using air alone for gastric balloon inflation is associated with a risk of balloon deflation and tube migration into the pharynx, causing possible airway obstruction and potential rupture of the oesophagus (Collyer 2007).
The balloon tamponade tube is then withdrawn, and the balloon held tight against the gastro-oesophageal junction by firm skin traction (Wong 2009). The use of external traction such as a 500 ml bag of crystalloid remains common practice; however, this is deemed unnecessary and increases the risk of tube migration (Collyer 2007).
In the case of Mr Smith, the balloon tamponade tube only remained in situ for a short duration prior to successful endoscopic therapy. Most guidelines recommend that balloon tamponade tubes should only be used for a period of up to 24 hours due to the high risk of associated complications. The risk of re-bleeding post-removal of the balloon tamponade tube is approximately 50% (Jalan and Hayes 2000; De Franchis 2005).
Breathing and ventilation
Prior to his elective intubation, Mr Smith was noted to be tachypnoeic with an increased respiratory rate of 23 breaths per minute. This increase in both respiratory rate and depth is due to a physiological response to cellular hypoxia resulting from his stage three hypovolaemic shock (Table 6.4) (Collins 2000; Bench 2004). It is also worth remembering that variceal haemorrhage is extremely distressing and patients are likely to have high levels of anxiety. Post-intubation and transfer to intensive care, Mr Smith was commenced on intravenous propofol and fentanyl to minimise stress and anxiety and to facilitate ventilation and achieve ventilator synchrony (see Chapter 11 for more in-depth information regarding the use of intravenous sedation). Both oxygen saturations and arterial blood gases need to be monitored closely to assess oxygenation levels and to detect any associated metabolic acidosis related to inadequate oxygen delivery (Collins 2000; Bench 2004).
Mr Smith was found to have tense ascites on physical examination. This fluid within the peritoneal cavity will cause both a reduction in his lung volumes and an increase on his abdominal pressure. Therefore, it is usual once the haemorrhaging is controlled for patients to undergo both a diagnostic and a therapeutic paracentesis. If more than 5 litres of ascitic fluid are removed, Mr Smith should receive 6–8 g of albumin per litre of ascites removed (for example, 100 ml 20% albumin for each 2–3 litres drained) (Moore and Aithal 2006).
Circulation with haemorrhage control
Hypovolaemic shock is associated with a greater risk of death; therefore, the primary treatment aims are prompt recognition, adequate venous/central access and early aggressive fluid resuscitation (SIGN 2008). The degree of shock and physical manifestations are dependent on the percentage of blood loss and are demonstrated in Table 6.4.
Table 6.4 Classification of hypovolaemic shock by blood loss.
On initial presentation Mr Smith’s percentage of circulating blood loss and increases in both respiratory and heart rate would categorise him in class 3 hypovolaemic shock (Table 6.3). The body’s response to hypovolaemia firstly results in a compensatory stage. During this stage the body attempts to compensate for the blood lost by vasoconstriction and diversion of blood to ‘vital organs’ (Adam and Osborne 2005). This can be seen in Mr Smith’s haemodynamic profile on admission, whereby in response to his hypotension and low circulatory volume, he presented with tachycardia. This occurs because the catecholamines adrenaline and noradrenaline are released in an attempt to increase cardiac output. It is worth noting that because of such compensation, a significant decrease in systolic blood pressure does not usually occur until 30% of blood volume has been lost (Collins 2000; Bench 2004; Garreton and Malberti 2007).
As this case study demonstrates, the need for intravenous access for rapid fluid resuscitation is of paramount importance. Multiple wide-bore peripheral cannulae should be inserted initially into anticubical fossa for rapid access. Ideally, patients should also have central venous access, and in some cases it may be necessary to use wide-bore central access into the femoral vein for rapid fluid replacement (Wong 2009).
Red blood cell transfusion should be considered after a 30% loss of the circulatory volume (SIGN 2008). Most patients can, however, be resuscitated with appropriate plasma expanders whilst cross-matched blood is awaited. Nonetheless, in severe cases of variceal haemorrhage, the administration of group-compatible or O-negative blood may be warranted whilst cross matching is taking place (Wong 2009).
Previous Cochrane reviews (Alderson et al. 2000; Finfer et al. 2004) have failed to demonstrate any statistically significant difference between crystalloids and colloids and no studies to date have compared these two fluid types in patients with an upper gastrointestinal bleed. Current guidelines therefore advocate that either solution may be used for volume restoration prior to blood transfusion (SIGN 2008).
Although a low haemoglobin is associated with a reduction of oxygen-carrying capacity, the optimal level for red blood cell (RBC) transfusion in critically ill patients remains controversial (van Heerden et al. 2002). The pioneering Canadian multi-centre study by Hébert et al. (1999) and subsequent research and meta-analyses continue to demonstrate the link between RBC transfusions and increased morbidity and mortality (Marik and Corwin 2008). A haemoglobin (Hb) of 8 g/dl is usually considered adequate for most critical care patients, with the exception of those with chronic respiratory conditions, cerebral vascular disease, cardiac disease or elderly patients who may need a higher threshold (Adam and Osborne 2005). For patients like Mr Smith, with acute variceal haemorrhage, it has been recommended that blood should be given cautiously, supporting a transfusion threshold of 8 g/dl of Hb or a haematocrit of 0.24, unless there is rapid ongoing bleeding or the patient has ischaemic heart disease (De Franchis 2005). Furthermore, it has been suggested that blood transfusions may induce rebound increases in portal hypertension, and thus increase the risks of both re-bleeding and death (Bosch 2009). Generally in the anaemic patient, a transfusion of 4 ml/kg packed cells should raise Hb by 1 g/dl (Adam and Osborne 2005). In addition to the association of increased mortality in critical care patients and RBC transfusions, a comprehensive literature research by Gerber (2007) suggests infections, immunosuppression, impairment of microcirculatory blood flow, 2,3-diphosphoglycerate deficiency and numerous biochemical and physiological derangements, including hypocalcaemia and coagulopathy, can additionally be seen. These problems are usually caused by either storage or inherent properties of the transfused blood.
Hepatocyte cells in the liver synthesise all clotting factors apart from factor Vlll which are synthesised in the epithelial cells. As a result, patients with liver disease have impaired production of these plasma proteins, and consequently, it is common for patients like Mr Smith to have altered coagulopathy as demonstrated in his laboratory findings (elevated PT and INR – Table 6.3). Cardenas and Gines (2009) suggest that as patients with acute variceal haemorrhage have advanced liver disease, this coagulopathy may contribute to the failure to control bleeding. This view is, however, not universally supported (Lisman and Leebeek 2007).
Fresh-frozen plasma (FFP) is frequently administered to patients who have cirrhosis and a prolonged prothrombin time (PT). O’Shaughnessy et al. (2004), however, suggest patients with a PT greater than four seconds longer than control, are unlikely to show any benefit from this. However, as no clotting factors remain in transfused RBC, it is usual for patients receiving large transfusions to additionally receive transfused FFP, as each unit of FFP increases each clotting factor by 2–3%. One unit is usually administered for each 5–6 units of RBCs transfused (Adam and Osborne 2005; Low and Milne 2007).
A mild to moderately reduced platelet count, as seen in Mr Smith’s data (Table 6.3), is common in patients with chronic liver disease and portal hypertension. One of the causes for thrombocytopenia is an increased platelet sequestration, as 90% of platelets are stored in the spleen. This occurs as a result of congestive splenomegaly, secondary to portal hypertension (Lisman and Leebeek 2007). Mr Smith’s platelet count on presentation was 47 000 (×109/l). It is advocated that patients should receive a platelet transfusion, if platelets are <50 000 (×109/l) (Mihas and Sanyal 2006). Each unit of platelets will increase the platelet count by 5000 (×109/l) (Low and Milne 2007).
Studies exploring the use and safety of haemostatic agents such as intravenous factor Vll (FVll), transexamic acid and desmopressin (DDAVP) in acute variceal haemorrhage have not demonstrated any benefits and are therefore not advocated for routine usage (Lisman and Leebeek 2007; Cardenas and Gines 2009).
One of the first-line therapies for acute variceal bleeding is the intravenous administration of terlipressin. Terlipressin is a synthetic derivative of vasopressin, and works by causing vasoconstriction of the mesenteric arterioles thus decreasing portal venous blood inflow and portal venous pressures. It is the initial drug of choice as it has clinically been proven to improve survival in placebo-controlled randomised control trials and meta-analyses (Mihas and Sanyal 2006; Bosch 2009). In the United Kingdom, terlipressin remains the only licensed therapy for variceal bleeding, although octreotide and somatostatin have been demonstrated to have some benefits and are widely used in North America.
The vasoconstrictive effects of terlipressin are not isolated to the splanchnic arterial bed; therefore, it is imperative to obtain a baseline ECG, prior to commencing therapy. Additionally, Mr Smith would need to be monitored for any signs and symptoms of ischaemia, for example, abdominal pain (small bowel ischaemia), chest pain (myocardial ischaemia) or peripheral vascular ischaemia (Mihas and Sanyal 2006; Wong 2009). The optimal time for drug therapy ranges between 2 and 5 days, when secondary prophylactic beta blockers can be commenced (De Franchis 2005).
Kidney failure due to either acute kidney injury (AKI) or hepatorenal syndrome frequently occurs with variceal bleeding. Consequently, early fluid resuscitation is of paramount importance to avoid hypovolaemia and hypotension (Bosch 2009). It is imperative that Mr Smith’s urine output and renal function are closely monitored, with the initiation of renal support therapies if warranted. AKI and renal replacement therapies are discussed in depth in Chapter 8.
Disability of the central nervous system
Hepatic encephalopathy is often precipitated by a gastrointestinal haemorrhage, as each 100 ml of blood within the gut will contain 15–20 g protein which when broken down will increase the ammonia production and thus potentiate or increase the level of hepatic encephalopathy. The main aim of therapy, therefore, is to clear the gut/bowel of blood to decrease ammonia production. Lactulose should be administered to Mr Smith either orally or nasogastrically at a dose of 10–30 ml three times daily with the aim of producing 2–3 semi-soft stools per day. In severe bleeds, however, this is often given alongside phosphate enemas to accelerate blood clearance (Abou-Assai and Vhahcevic 2001; Sargent 2007; Houlston and O’Neil 2009). Prior to his admission, Mr Smith had abstained from alcohol for several months. Patients who are actively drinking prior to admission, however, should be monitored for alcohol withdrawal and commenced on an appropriate alcohol withdrawal protocol (Mihas and Sanyal 2006). Patients with alcohol-related liver injury are additionally at risk of developing Wernicke’s encephalopathy caused by thiamine deficiency. Mr Smith should, therefore, receive intravenous B vitamins (Pabrinex(R)) followed by a course of oral thiamine (Sargent 2006).
There are still some false assumptions that patients with liver cirrhosis need to be protein restricted to reduce the risk of hepatic encephalopathy. Protein intolerance is rare, and protein restriction has not been shown to have any major consequence on either liver function or plasma ammonia and can exacerbate protein breakdown (Cordoba et al. 2004; McCullough 2006). The incidence of protein calorie malnutrition in decompensated cirrhosis has a prevalence of 80–100%, regardless of the underlying aetiology. Nutritional requirements should therefore be met aggressively (Hamlin and Leaper 2009). The European Society of Parenteral and Enteral Nutrition (ESPEN) advocates that patients with cirrhosis should receive 35 kcal/kg/day and 1.2 g/kg/day of protein (Plauth et al. 2006). Reluctance to place a nasogastric tube due to fears of displacement or precipitating further variceal bleed is unfounded. Tubes can usually be placed 24 hours post-cessation of bleeding without risk (Plauth et al. 2006).
Insulin resistance and diabetes frequently occur in cirrhotic liver disease; therefore, Mr Smith will need his blood glucose monitored regularly (Hamlin and Leaper 2009). The management of altered blood glucose and the benefits of tight glycaemic control are discussed in greater depth in Chapter 7.
Exposure/environment
Because of the high risk of sepsis in this group of patients, and the link between infection and early re-bleeding, antibiotic therapy is considered an integral part of therapy and, as in the case of Mr Smith, should be instituted from admission (De Franchis 2005). A meta-analysis has demonstrated that antibiotic use reduces the mortality of patients who develop acute upper gastrointestinal bleeding in association with chronic liver disease (SIGN 2008). Strict asepsis of invasive lines with early removal is also paramount.
Because of the risk of spontaneous bacterial peritonitis (SBP) of his ascitic fluid, Mr Smith should undergo routine paracentesis. The diagnosis of SBP is made upon microscopic examination of the ascitic fluid. The presence of a white cell count of >250 polymorphonuclear leucocyte cells/mm3 is usually diagnostic and indicates the need to commence broad spectrum antibiotics (Gines et al. 2004).
Conclusion
Variceal haemorrhage associated with liver cirrhosis and portal hypertension is associated with high mortality. As this scenario demonstrates the initiation of appropriate airway management, aggressive fluid resuscitation, the application of pharmacological and endoscopic therapy and recognition and prevention of any associated complications are of paramount importance.
Key learning points
- The development of portal hypertension and subsequent complications of oesophageal varices and ascites mark the transition from compensated to decompensated cirrhosis.
- Oesophageal varices can result in torrential haemorrhage which is associated with a high mortality.
- The securing of a patent airway and maintaining of haemodynamic stability with aggressive fluid resuscitation are of paramount importance and take priority over endoscopic therapy.
- Endoscopic band ligation is considered superior to sclerotherapy.
- Nutrition support with no protein restrictions, good bowel management and prophylactic antibiotic therapy are an essential part of management in patients with liver cirrhosis.
Critical appraisal of research paper
Vincent JL, Sakr Y, Sprunh C (2008) Are blood transfusions associated with greater mortality rates? Results of the sepsis occurrence in acutely ill patients study. Anesthesiology 108, 31–39.
The Sepsis Occurrence in Acutely Ill Patients Study investigated the relationship between blood transfusions to mortality in 198 European intensive care units. All patients admitted during a two-week period in May 2002 were included in the study, and followed either until death or hospital discharge or for a period of 60 days. Results demonstrated that the transfused patients had both a longer length of admission and a higher mortality rate.
Reader activities
1. Read the research article written by Vincent et al. (2008).
2. Using the critical appraisal framework in Appendix I, consider the methodological quality of the paper.
3. Reflect on the use of transfused blood products in your clinical practice; consider your current haemoglobin thresholds and which groups of patients are the primary recipients of blood products.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



