Scenario 2
Peter, a 73-year-old gentleman is admitted with type II (hypercarbic) respiratory failure (non-pneumonic). He has chronic obstructive pulmonary disease (COPD) and smokes 30 cigarettes a day. He is normally quite well and has had no previous ICU admissions. His last hospital admission was one year ago for exacerbation of his COPD.
Following an unsuccessful trial of non-invasive ventilation (NIV) on a general ward, he was intubated and ventilated on biphasic positive airways pressure (BIPAP). An assessment of his status at this point can be seen in Box 2.2.
Box 2.2 Peter’s initial assessment data.
| pH | 7.2 |
| PaCO2 | 11 kPa |
| PaO2 | 7.5 kPa |
| HCO3− | 30 mmol/L |
| Base excess (BE) | −6 mmol/L |
| FiO2 | 0.4 (40%) |
| Inspiratory pressure | 25 cmH2O |
| PEEP | 10 cmH2O |
| Set respiratory rate | 14 breaths per minute |
After 24 hours of ventilation on BIPAP, blood gases begin to normalise and weaning is commenced by reducing the mandatory respiratory rate to 8 breaths per minute. Peter is seen to be making an effort to breathe. Two hours later the ventilation mode is changed to continuous positive airways pressure (CPAP) of 5 cmH2O with pressure support of 25 cmH2O; however, Peter soon begins to tire. Tidal volumes drop from 500 to 300 mL and the total respiratory rate increases from 20 to 35. Peter’s breathing appears laboured and he is using all his accessory muscles. He becomes tachycardic, hypertensive and restless.
Reader activities
Having read the two scenarios, consider the following questions:
- When should John’s weaning have been commenced?
- What factors should you take into consideration when preparing to wean John?
- How would you wean John and Peter? Write a weaning plan for Peter.
- What parameters would you use to wean Peter and John?
- Do you think Peter would be difficult to wean?
- How would you know Peter had tired?
- Why are ABGs not the first sign of fatigue/respiratory distress?
Definition of weaning
Doctoral research has indicated that weaning is often defined, by nurses, according to the technology used and location of care (Crocker 2006). Moreover, the traditional view of weaning centres upon the eventual liberation of the patient from the ventilator (American College of Chest Physicians, the American Association for Respiratory Care and the American College of Critical Care Medicine (Collective Task Force) 2002). The method of respiratory support required and the geographical location are immaterial. Weaning may also be said to begin as soon as the decision to reduce the level of respiratory support is made.
There are two stages to weaning, pre-weaning or titrating ventilator support and active weaning (Crocker and Kinnear 2008). Pre-weaning involves preparation for weaning in order to optimise the weaning process and should begin as soon as the patient is ventilated. The weaning process should involve the patient. One single-weaning trajectory is not possible; patients are individuals and, as such, weaning must be individualised. A description of patients’ weaning trajectories as described by Egerod (2003) illustrates this. The Modernisation Agency (MA 2002) classifies weaning depending on the requirement for ventilatory assistance (Table 2.2).
Table 2.2 Classification of weaning.
Source: Modernisation Agency (2002).
| Acute ventilatory dependence | 6 hours a day, includes CPAP, NIV and IPPV |
| Weaning delay | Need for ventilation for >2 weeks in absence of non-respiratory factor |
| Chronic ventilatory dependence | CPAP by mask excluded, IPPV required regularly day or night irrespective of the number of hours |
| Weaning failure | Ventilation >3 weeks |
For the purposes of this chapter weaning is defined as:
The gradual reduction of respiratory support (excluding oxygen) until the point has been reached when the patient either no longer requires assistance (for 24 hours a day) or has reached their maximum potential and has therefore come to a position when a further reduction of support cannot be achieved. In this case the patient may still require continuous or intermittent respiratory support.
In the past, patients with COPD have been associated with delayed weaning or failure to wean and, thus, clinicians have been reluctant to instigate invasive ventilation (Wildman et al. 2003). Recent research, however, has demonstrated that such patients can have a good outcome (Ai-Ping et al. 2005), and this has improved significantly with the introduction of NIV (Keenan et al. 2003) and the development of weaning centres (Quinnell et al. 2006).
Pathophysiology related to weaning
Initial weaning failure is usually due to incomplete resolution of the underlying illness which necessitated ventilation or the development of a new problem. Weaning depends on the strength of the respiratory muscles, the load applied to these muscles and central drive (see Table 2.3).
Table 2.3 The determinants of ventilation and common conditions associated with failure to wean.
Source: Adapted from Hemant et al. (2006).
| Central drive | Respiratory muscle strength | Load |
| Sedation | Disuse atrophy | Left-ventricular failure |
| Metabolic alkalosis | Polyneuropathy | Pulmonary oedema |
| Delirium Raised intracranial pressure | Prolonged use of steroids, aminoglycosides and muscle relaxants | Hyperinflation |
| Hypophosphatemia and hypomagnesia | Bronchospasm, upper airway obstruction | |
| Hyperinflation | Restrictive conditions, obesity, pleural effusions | |
| Ventilator-induced lung injury | Ventilator–patient dysynchrony | |
| Increased carbon dioxide production |
The adequacy of pulmonary gas exchange and the performance of the respiratory pump are important considerations during weaning assessment. The most common reason for failure to wean is an inadequate respiratory pump caused by either a decrease in the neuromuscular capacity of the respiratory muscles or an increased load (Krachman et al. 2001). For example, due to the COPD, Peter’s lungs are hyperinflated, which results in a mechanically disadvantaged respiratory pump. Peter also has evidence of bronchospasm on auscultation. Any additional load such as this can lead to the development of respiratory muscle fatigue.
Tests and investigations
Assessment of readiness to wean
There are no absolutes in weaning. Much of weaning is trial and error. There are two stages involved: pre-requisites or assessment of readiness for weaning and consideration of the method of weaning itself.
The first pre-requisite is that the reason for ventilation is resolving. A systematic assessment of the patient’s readiness to wean should then follow. Many units have written guidelines to assist decision-making (for example, see Table 2.4). These will include parameters within which it is considered safe to wean. Many of these have been developed based on clinician experience rather than research evidence.
Table 2.4 Pre-requisites for weaning and readiness to wean.
| Pre-requisites for weaning | ||
| Physical | Respiratory | FiO2 <0.5, FiO2/PaO2 150–300 mmHg, low levels of PEEP, acid–base balanced, ABGs acceptable and normal for patient, chest secretions acceptable. CXR acceptable. |
| Cardio-vascular system | CVS stable (± inotropes), Hb >7, or 10 g/L for COPD, temp <38.5°C, >35°C | |
| Central nervous system | Respiratory drive in tact, pain controlled, sedation off or minimal amount, ICP within normal range | |
| GI tract | Feeding in progress or being considered, trace elements normalised, gut not distended | |
| Psychological | Anxiety/mood/motivation | Patient prepared, involved, has rested, consider assessment of anxiety, mood, motivation, sleep, presence of delirium and treat appropriately |
| Readiness to wean | ||
| Occlusion pressure (PO.1) | Normal value −3.4 to −4.5 | Determines patient’s level of support required and assessment of respiratory muscle function. |
| Rapid shallow breathing index (RSBI) | Below 105 | f divided by TV |
| Spontaneous breathing trials (SBT) | 30–120 minutes. T-piece or ventilator mode with or without PEEP and support/tube compliance | Once daily. If successful commence weaning, unsuccessful continue to ventilate. |
Using these pre-requisites, can you identify when John could have been assessed for weaning readiness? Can you see why it is important to have a two-stage approach to weaning? Preparing the patient for weaning is as important as weaning itself. The amount of oxygen and the level of sedation given to John could have been reduced much earlier and this would have allowed for weaning suitability to be assessed. There was a delay in preparing John to wean and this resulted in extending the number of ventilator days.
Inspiratory volumes
Normal Vt in an adult is 5–7 mL/kg. Therefore, a male of 70 kg would be expected to have a Vt of 350–490 mL. Compare this with John’s set Vt of 700 mL a level at which acute lung injury could be triggered (see Chapter 1).
Respiratory rate and Vt are sensitive indicators of respiratory fatigue. When Vt drops, respiratory rate increases in response, in order to maintain an adequate minute volume, as can be seen in Peter’s data. Gas exchange may not be affected until the Vt drops to a level whereby effective ventilation is compromised, and at this stage ABGs change. It is therefore important to monitor the patient’s respiratory observations closely and not rely solely on blood gases. In this way respiratory fatigue is picked up early and appropriate interventions can be applied.
A number of additional tools are available, which can be used to help predict the likelihood of successful weaning for John and Peter, and guide the speed at which weaning takes place.
The ratio of PaO2 to FiO2 is commonly used as an additional measurement in assessing oxygenation in mechanically ventilated patients. The PaO2/FiO2 ratio is calculated by dividing the PaO2 by the FiO2 (see Box 2.3 for examples).
Box 2.3 Calculation examples for PaO2/FiO2.
John’s initial ABG showed a PaO2 of 13kPa. Dividing this by his FiO2, which was 0.1, gives a PaO2/FiO2 ratio of 130 kPa.
Peter’s initial PaO2 was 7.5 kPa. Dividing this by his FiO2, which was 0.4, gives a PaO2/FiO2 ratio of 18.75 kPa.
A value less than 40 kPa would indicate inadequate gas exchange and thus would require an increase in support.
Rapid, shallow breathing is the frequency of breaths (f) divided by the tidal volume in litres (Vt) (Howie 1999). John’s initial respiratory rate was 12 breaths per minute. Dividing this by his Vt, which was 700 mL, and multiplying it by 1000, to convert into litres, gives him an RSBI of 17. Further examples can be seen in Table 2.5. An RSBI of less than 105 has been widely accepted as an adequate value upon which to commence or progress weaning and extubation (Yang and Tobin 1991).
Table 2.5 Calculation examples for PaO2/FiO2.
Airway occlusion pressure (P0.1) could also be used to assess John’s and Peter’s readiness to wean. Many acute diseases will increase the work of breathing (WoB) by altering compliance, airway resistance and carbon dioxide production. An increase in WoB also increases oxygen demand. The patient’s ability to tolerate this is dependent on the power of their respiratory pump. This is dependent on the strength and endurance of the respiratory muscles. One way of measuring this is to use P0.1 (Whitelaw and Derenne 1993). This gives a measurement of the effect of all the respiratory muscles active at a given time and does not depend on resistance or compliance of the respiratory system. Many ventilators now have this measurement facility. It is operated by occluding the inspiratory limb for 0.1 second. This would not cause any adverse effect on Peter or John and they would be unaware that it was being measured. Normal values are between −3.5 to −4.5 cmH2O (see Table 2.6). The interpretation of occlusion pressure must, however, be treated with caution. Although it is reliable in measuring output at the first part of inspiration, it should be used in conjunction with other measures and indices.
Table 2.6 Interpretation of P0.1 and clinical applications.
| P0.1 Value | Interpretation | Clinical application |
| −3.4 to −4.5 | Normal range | Ventilation optimal |
| Below −3.5 | Suggests patient is able to do more or ventilator providing too much support ventilator | Reduce support (e.g. reduce ASB) Note: A very low value (<1.0) may indicate the patient is unable to initiate a breath due to severe weakness or over sedation. |
| Above −4.5 | Suggests patient requires more support | Increase support (e.g. increase ASB or add a rest period). |
| −6 or above | Suggests the patient is tired and may fail to wean | Rest and provide full ventilation for 24 hours. |
Spontaneous breathing trials (SBT)
Many units now include an assessment of the patient’s readiness to wean using a daily spontaneous breathing trial (SBT). This can be achieved in two ways: either using a T-piece with 5 cmH2O of PEEP or using a spontaneous mode on the ventilator with 5 cmH2O PEEP and some level of support or tube compliance to counteract the extra WoB. The length of time the trial should last is a matter of debate. This ranges from 30 minutes to 2 hours. If there are no signs of fatigue, then weaning may begin. If the patient fails, then no further attempt at weaning should be made until the following day. Signs of fatigue have been defined by the Spanish Collaborative Group (Brochard et al. 1994; Esteban et al. 1995). These are:
- Respiratory rate (RR) > 35/minute or a change in RR > 50% above baseline
- SaO2 < 90%
- Heart rate > 140 or sustained increase or decrease of 20% lower than baseline
- Systolic blood pressure > 180 mmHg or < 90 mmHg
- Increased agitation
- Signs of increased WoB.
Other available tools include the weaning continuum developed by Burns et al. (2000). The Burns Wean Assessment Programme (BWAP) is a computer application designed to help clinicians assess, evaluate and track factors important in weaning but has not been widely used in the UK (Burns et al. 1994).
Managing the patient during weaning
Following a decision to commence weaning, a number of issues need to be considered.
Methods of Weaning
A number of randomised controlled trials (RCTs) have been conducted in an effort to develop a body of evidence to support the systematic weaning of patients (for example, Esteban et al. 1995). The extensive research has not, to date, however, provided a clear answer as to the best method of weaning. This could be due to the inconsistencies in design. Firstly, patient groups were not homogenous and included short- and long-term patients, those following surgery and those with chronic disease. Secondly, the definition of successful weaning varied from 2 to 48 hours post-separation from the ventilator, with some studies including extubation as a criterion. Thirdly, weaning failure was inconsistently defined, and fourthly, outcome measures were not consistently applied. In a review by Meade et al. (2001), it was identified, however, that although all these factors may have obscured the impact of the ventilation mode, results do suggest that multiple daily T-piece weaning or pressure support may be superior to synchronized intermittent mandatory ventilation. Further, Meade et al. (2001) suggest that early extubation with the use of non-invasive positive-pressure ventilation as required may be a useful strategy in selected patients.
Peter is likely to be more difficult to wean due to his history of COPD. Butler et al. (1999) conducted a systematic review of the literature in difficult-to-wean patients in order to ascertain which of the three commonly used techniques of weaning (T-piece; SIMV or pressure support ventilation (PSV)) leads to the highest proportion of successfully weaned patients in the shortest time. Difficult-to-wean patients were determined by the length of time on the ventilator (over 72 hours) or a failed trial of spontaneous breathing after 24 hours of ventilation. Only 4 out of 667 identified studies met the criteria for the review.1 Although individual trials reported outcomes in favour of a specific weaning mode, no mode was demonstrated to be consistently superior to the other two. Two of the four studies gave conflicting results, Brochard et al. (1994) supporting PSV and Esteban et al. (1995) supporting T-piece as the optimum method of weaning. Pooling of the results only highlighted the heterogeneity of the study designs.
Results of the reviews by Meade et al. (2001) and Butler et al. (1999) indicate that there is currently insufficient evidence to identify a clearly superior mode for weaning any group of patients. Furthermore, Butler et al. (1999) state that the manner in which the mode of weaning is applied may have a greater effect on the likelihood of weaning than the mode itself (Butler et al. 1999: 2332). Differences in clinicians’ intuitive threshold for the reduction or discontinuation of ventilatory support appears to have a greater impact on the failure of SBTs, and on reintubation, than do modes of weaning (Meade et al. 2001). Clinical decisions regarding choice of mode may also be determined by the ventilators available within the department and the knowledge and competence of the healthcare staff utilising them.
Based on this evidence, the methods of ventilation used for John and Peter could both be considered suitable, although the parameters set need to be adjusted to ensure that that ventilation does not cause more harm than good (see Chapter 1 on ALI/ARDS for information on lung protective ventilation). Further, the decision to progress Peter from BIPAP to CPAP and PS appears justified.
The nursing role
Nursing research in this area has focused on patient communication whilst being ventilated (Bergbom-Engberg and Haljamae 1989; Hafsteindottir 1996), patients’ recollections of stressful experiences whilst being ventilated (Gries and Fernsler 1988; Jablonski 1994; Rotondi et al. 2002) or patients’ perceptions of fatigue (Higgens 1998). The patients’ view of weaning has been under-investigated until recently (Cook et al. 2001). In a Canadian study of 20 patients undergoing ventilation and weaning, it was revealed that patients were actively engaged in a variety of physical, cognitive and emotional activities that contributed to successful weaning. These activities patients called work (Logan and Jenny 1997). The authors concluded that patients’ work should be understood and supported by clinicians (nurses) in order to facilitate recovery from mechanical ventilation and weaning (Logan and Jenny 1997: 140). In a more recent study, Johnson (2004) interviewed nine Australian ICU patients undergoing weaning and identified four themes. Reclaiming the everyday world (the only theme discussed in the published literature) meant re-engaging with staff (and families) in the ICU, seeking control over treatments and attempting to communicate, question and interpret the environment (Johnson 2004). It is vital that these findings are taken into consideration if we are to understand and respond appropriately to the needs of patients like Peter.
The lack of consensus regarding the method of weaning has resulted in a change of focus in the literature to the use of protocols (for example, Blackwood et al. 2004; Tonnelier et al. 2005) and the role of the healthcare professional in weaning (for example, Blackwood 2003; Fulbrook et al. 2004; Gelsthorpe and Crocker 2004). Thorens et al. (1995) was the first paper (Swiss) to investigate the influence of the quality of nursing on the duration of weaning from mechanical ventilation in patients with chronic respiratory disease. Using an ‘index of nursing’, the effective workforce of nurses (indicated by the number of nurses and their qualifications) was compared with the ideal workforce required by the number of patients and their severity of disease. This index of nursing was then compared to the duration of weaning from mechanical ventilation. The study concluded that the quality of nursing appeared to be a measurable and critical factor in patients who were weaning with chronic respiratory disease. During the study, there were a number of changes, including an increase in medical staff and beds. These and other factors such as nurse education were not explored and these may have had bearings on the study. Despite this important research, there has not been any attempt to replicate or extend this work.
Despite many references to reducing weaning times using protocols (for example, Kollef et al. 1997), it is not clear whether nurse-led weaning strategies hasten weaning from mechanical ventilation compared to physician-led strategies. A systematic review of the literature by Price (2001) argues there is no evidence that nurses are leading weaning and therefore reducing weaning time, and suggests that it is the use of protocols rather than the person leading the weaning process that makes the difference (Price 2001). Recent research comparing protocol-led weaning by nurses to a historical matched cohort in a French ICU showed that nurse protocol-directed weaning does reduce the duration of mechanical ventilation and the length of stay in the ICU (Tonnelier et al. 2005). The incidence of ventilator-associated pneumonia (VAP), ventilator discontinuation failure rates and ICU mortality were similar in both groups.
Evidence of weaning effectiveness on its own does not guarantee that protocols will be used in practice (Blackwood 2003). Furthermore, there is a thought that protocols are too difficult to develop due to the unpredictability of patients’ illnesses (Blackwood et al. 2004). The use of protocols or nurse-led weaning is not yet a common practice in ICUs in England (Blackwood 2003). A survey demonstrated that clinicians (doctors) were leading weaning in 152 units, with only 33 (17%) units using protocols (Modernisation Agency 2002: 16).
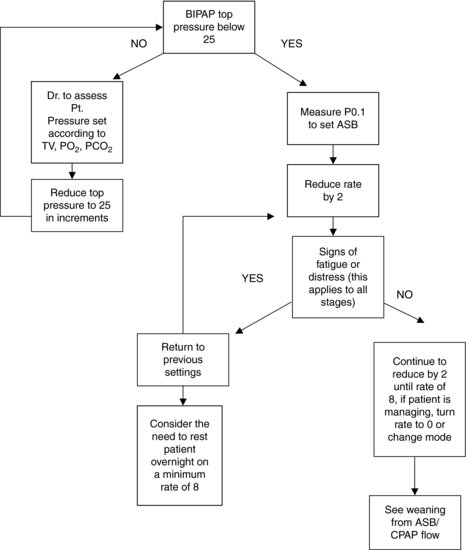
Fairman and Lynaugh (1998) found in their study of American intensive care nurses that the use of protocols strictly limited the scope of nurses’ patient care decisions, but represented an enormous change in doctor–nurse relationships. Where protocols did not exist, nurses and doctors continued to make informal contracts defining boundaries of nurses’ authority and responsibility. Protocols may be seen as a form of restraint applied by the intensivists. Nurses may appear happy to accept the use of protocols in order to extend their decision-making, which was previously limited (Crocker 2002). This was not found to be the case in a recent pilot study (Gelsthorpe and Crocker 2004). The authors demonstrated that nurses based the decision to wean on their professional judgement and disregarded the weaning protocols2 (see Figure 2.1 for an example of a weaning protocol). The authors suggested that protocolised weaning may not be useful in the decision to commence weaning as individual judgement may override the protocol and cause variance in weaning (Gelsthorpe and Crocker 2004). The use of protocols in weaning may be a form of control; therefore, their use may be seen as not only limiting nurses’ powers of decision-making but also reducing it to not much more than following a set of guidelines. Nurses, however, may not be in a position to accept this transfer of technology. Gelsthorpe and Crocker (2004) showed that nurses were delegating the responsibility for weaning to the medical staff. Experience was an influential factor in establishing the decision to wean, with less-experienced staff erring on the side of caution and delaying weaning. The study demonstrated that weaning followed a medical paradigm (systems approach) with a concentration on physiological factors which influenced the decision to wean. Blackwood et al. (2004) identified that physicians in the ICU had reservations regarding the use of protocols in weaning because of the variability of nursing experience and indicated that doctors should retain control over weaning. The transfer of technology from medicine to nursing, therefore, is not a simple one.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree