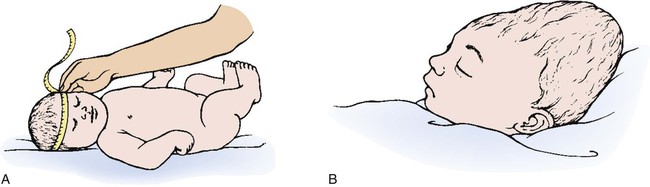
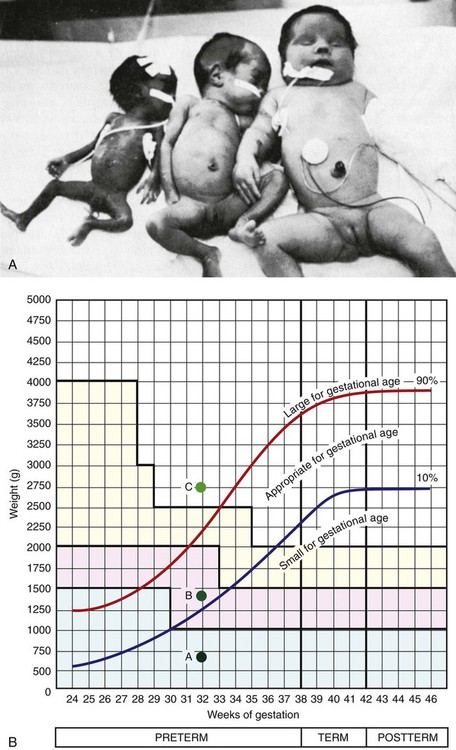
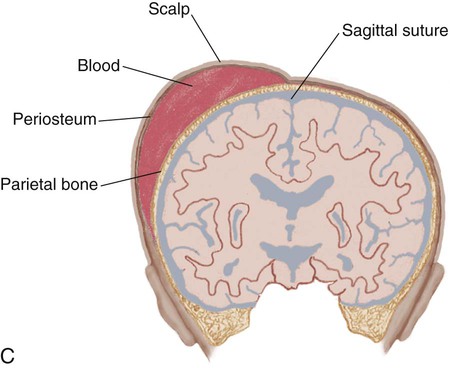
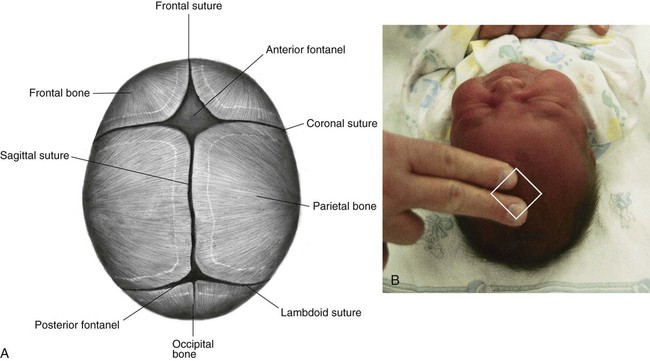
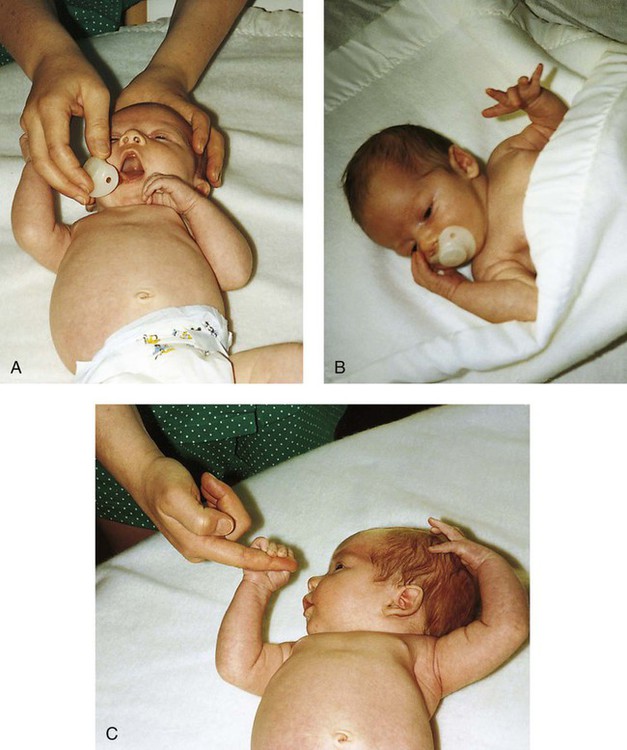
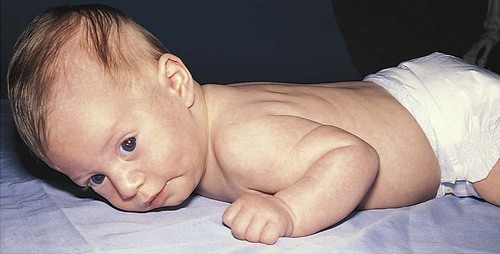
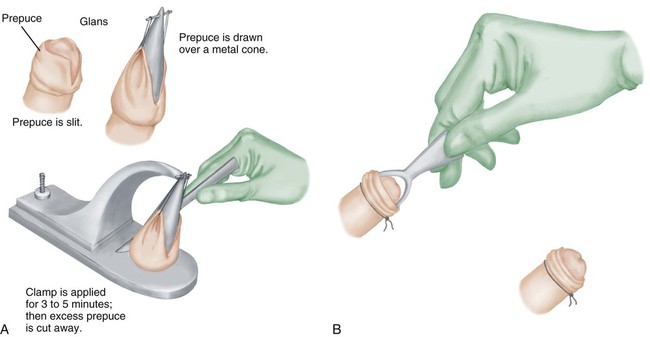
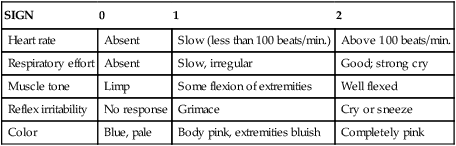
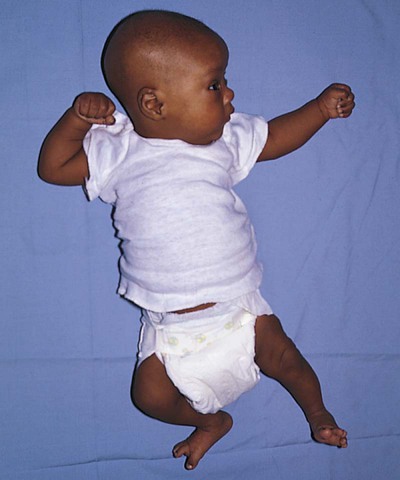
1. Define the vocabulary terms listed 2. Discuss the importance of airway maintenance in the neonate 3. Identify the range of average measurements in the newborn infant 4. Describe the importance of thermoregulation, particularly in the preterm infant 5. Discuss normal vital signs of the newborn 6. Differentiate AGA, SGA, and LGA infants 7. Differentiate low–birth weight, very low–birth weight, and extremely low–birth weight neonates 8. Describe the APGAR and the Ballard scoring systems 9. Briefly describe three normal reflexes of the neonate (including approximate age of disappearance) and the tests for their appearance 10. Discuss implications and treatment methodologies of jaundice in the newborn 11. List three causes of preterm birth 12. Describe the differences in care for the preterm infant with respiratory distress syndrome and apnea 13. Differentiate hypoglycemia and hypocalcemia 14. List three characteristics of the postterm infant 15. Describe the six neonatal states of the newborn 16. Discuss medications administered to the newborn 17. Discuss the purpose of metabolic screenings 18. Compare and contrast breastfeeding and formula feeding 19. Contrast the techniques of feeding the preterm and the full-term neonate 20. Describe precautions to prevent infection while caring for the newborn 21. Summarize teaching principles of bathing the newborn, providing cord care, and providing circumcision care 22. Discuss ways to help facilitate the maternal-infant bonding process for a preterm neonate Every parent wants a perfect baby. Reality is, however, that not all babies are born without defects. Birth defects can vary from minor to fatal. Chapter 1 discusses infant mortality. A birth defect is defined as “an abnormality of structure, function, or metabolism (body chemistry) present at birth that results in physical or mental disability or death. Several thousand different birth defects have been identified. Birth defects are the leading cause of death in the first year of life” (March of Dimes, 2006). Birth defects are the cause of death in one of every five infant deaths. The March of Dimes lists three major categories of birth defects: structural/metabolic, congenital infections, and other. Because these disorders include so many conditions, it has been necessary to limit the number discussed in this chapter and to discuss others in relevant areas of the textbook (see the Index for specific conditions). When a baby is born, an orderly process of adaptation from fetal life to extrauterine life takes place. All the body systems undergo some change. Respirations are stimulated by chemical changes within the blood and by chilling. Sensory and physical stimuli also appear to play a role in respiratory function. Gentle physical contact is used to provide stimulation to begin breathing. Cold, pain, touch, movement, and light are other stimuli that affect the stimulation of respirations. With the first breath, which initiates the opening of the alveoli, the newborn enters the world of air exchange and begins an independent existence. In addition, this process begins cardiopulmonary interdependence (see Chapter 12). The ability of the neonate to metabolize food is hampered by immaturity of the digestive system, particularly by deficiencies in enzymes from the pancreas and the liver. Although the kidneys are developed structurally, their ability to concentrate urine and maintain fluid balance is limited. This is because of a decreased rate of glomerular flow and limited renal tubular reabsorption. Most neurologic functions are also primitive. A system for recording the condition of the neonate and the need for resuscitation was devised by Dr. Virginia Apgar and is currently used in many delivery rooms. The first assessment is made 1 minute after delivery. This generally produces the lowest score. A second evaluation is made after 5 minutes. Table 5-1 shows how to determine the Apgar score. An infant with a score of 8 to 10 is in good condition and needs only routine suction and observation. Infants with a score of 4 to 7 require various forms of intervention and close observation. An infant with a score of 0 to 3 needs resuscitation and care in the NICU. Apgar scores, however, are not the sole indicator used to evaluate the long-term prognosis of a child. Table 5-1 Head circumference is generally between 33 and 35 cm (13 to 15 in). This measurement may be somewhat less because of the molding process during a vaginal delivery (Figure 5-1). Within 2 to 3 days, it is usually the normal size. Chest circumference is normally 30.5 to 33 cm (12 to 13 in). Head circumference is generally about 2 to 3 cm (1 in) greater than the chest circumference. The most accurate way to determine body temperature is to measure it with a thermometer. The initial temperature of the neonate is generally taken via the axillary route. It is not usually taken rectally because this method could cause perforation of the mucosa. Tympanic thermometers are not as accurate in a newborn. Daily routine temperatures are taken in the axilla. Review the procedure for evaluation of vital signs in Chapter 3. Immediately after birth, the newborn is thoroughly dried (especially the hair) to eliminate evaporative heat loss and placed uncovered under radiant heat (Figure 5-2). The premature infant may be placed in the isolette (Figure 5-3). The infant’s temperature is maintained at a constant level with a heat-sensitive probe that is taped over a nonbony prominence on either the abdomen or back. This allows the infant to become a thermostat for the radiant warmer. The infant’s axillary temperature is also monitored. Overhead radiant warmers have the advantage of providing easier access to the child while maintaining a neutral environment. The nurse should also do the following: • Prewarm all surfaces that come in contact with the infant. • Use discretion in bathing the infant. Regular assessment has a much higher priority than a routine daily bath because of the danger of loss of heat through evaporation. • Provide a plastic heat shield (vapor shield) for very low–birth weight infants. • Use knitted caps and booties when the infant is removed from the radiant warmer or isolette. • Wrap the infant in a blanket if he or she is removed from the radiant warmer or isolette. If the newborn is placed on the mother’s chest, skin-to-skin contact should be maintained. A cap for the newborn prevents heat loss (Figure 5-4). The nurse remains with the mother and the newborn to ensure their safety, to monitor progress, and to ensure that the newborn stays warm. Table 5-2 discusses types of heat loss. Table 5-2 An apical heart rate should be auscultated for 1 full minute (discussed in Chapter 3) in the newborn, and it can range between 120 and 160 beats per minute. This rate may increase if the infant is crying and decrease if the infant is sleeping. As a general rule, however, if the pulse is above 180 or drops below 100, the finding should be reported. Blood pressure in the newborn is usually low, and use of the correctly sized cuff is important. The average blood pressure at birth is 80/46 mm Hg. Gestational age refers to the actual time from conception to birth that the fetus remains in the uterus. A full-term infant is born between 38 and 42 weeks after conception. Infants born between 34 and 37 weeks are considered late preterm, while those born at less than 34 weeks are called preterm, and those born at more than 42 weeks are called postterm. Infants are considered appropriate for gestational age (AGA) if they are born between the 10th and 90th percentiles for weight. This infant has grown at a normal rate, regardless of the time of birth. If the infant is small for gestational age (SGA), below the 10th percentile, the infant has experienced intrauterine growth restriction or delay. In a similar fashion, those infants weighing above the 90th percentile on intrauterine growth curves are referred to as large for gestational age (LGA). Emphasis is placed on the gestational age and the level of maturation—preterm, term, and postterm (Figure 5-5). Current data also indicate that intrauterine growth rates are not the same for all babies and that individual factors must be considered. • Low–birth weight (LBW) infant—an infant whose birth weight is less than 2500 g (5.5 lbs), regardless of gestational age • Very low–birth weight (VLBW) infant—an infant whose birth weight is less than 1500 g (3.3 lbs) • Extremely low–birth weight (ELBW) infant—an infant whose birth weight is less than 1000 g (2.2 lbs) • Intrauterine growth restriction (IUGR)—an infant whose intrauterine growth is restricted Several differences are seen between a premature and a full-term infant. Muscle tone is decreased in the infant who is not full-term. The position that the infant maintains can also indicate low gestational age. When in a prone position, the full-term infant lies with the pelvis high and the knees drawn up under the abdomen. The premature infant that is placed in a prone position lies with the pelvis low and the knees at the side of the abdomen, with the hips flexed. In the supine position, the infant of 28 to 32 weeks’ gestational age lies in a froglike position with the lower limbs extended and the hips abducted. The full-term infant in a supine position lies with the limbs strongly flexed. Differences also exist in the hand movement of the infant across the chest to the opposite side of the neck. The reach of an infant of 28 weeks’ gestation can extend well past the acromion, whereas the hand of the full-term infant does not go beyond that point. If the hand is put behind the neck to the opposite side, the same difference between the ages is noted. This is called the scarf sign (Figure 5-6). The new Ballard scoring system is used to determine gestational age and consists of an evaluation of physical characteristics and neuromuscular tone (see Appendix C). This condition usually clears within 24 to 48 hours. Occasionally, a hematoma (hemato, blood; oma, tumor) protrudes from beneath the scalp. The cephalhematoma takes longer to subside, but it usually clears by the time the infant is 2 to 4 weeks of age (Figure 5-7). Cephalhematoma can increase the risk of hyperbilirubinemia (the additional accumulation of blood increases the number of red blood cells, therefore there is an increased release of bilirubin; refer to section on jaundice). Fontanels are junctures at the cranial bones that can be felt as soft spots on the cranium of the young infant. Two can be palpated on the neonate’s head. The fontanels may be smaller immediately after birth than several days later because of molding. The anterior fontanel is diamond-shaped and located at the junction of the two parietal and the two frontal bones. It usually closes by 12 to 18 months of age (Figure 5-8). The posterior fontanel is triangular and located between the occipital and the parietal bones. It is much smaller than the anterior fontanel and has usually ossified by the end of the second month. The pulsating of the anterior fontanel may be seen by the nurse. These areas are covered by a tough membrane, and there is little chance of their being injured with ordinary care. The nervous system directs most of the body’s activity. The neonate can move his or her arms and legs vigorously but cannot control them. The reflexes that a full-term baby is born with, such as blinking, sneezing, gagging, rooting, sucking, and grasping (Figure 5-9 and Table 5-3), help keep the child alive. The rooting reflex causes the infant to turn the head in the direction of anything that touches the cheek, such as in anticipation of food. The nurse should remember this when helping a mother breastfeed her infant. If the breast touches the infant’s cheek, the newborn turns toward it to find the nipple. The infant can also cry, swallow, and lift the head slightly when lying on the stomach. If startled, the newborn extends the extremities and then draws the legs up and folds the arms across the chest in an embrace position. The hands open, but the fingers often remain curved. This is normal and is called the Moro reflex (Figure 5-10). Its absence may indicate abnormalities of the nervous system. Table 5-3 Neurologic Signs Present at Birth in the Newborn The tonic neck reflex is a postural reflex that is sometimes assumed by babies while asleep (Figure 5-11). The head is turned to one side, with the arm and leg extended on the same side, whereas the opposite arm and leg are flexed in a “fencing” position. This reflex disappears around the 20th week of life. Prancing movements of the legs, seen when a newborn is held upright on the examining table, are termed the dancing reflex. Undetected hearing loss can cause a child to develop problems in speech, language, and cognitive development and can also lead to development of behavioral problems. Hearing loss is a common birth defect, occurring in up to 3 per 1000 newborn infants, and needs to be identified as soon as possible. In the past, parental observation and assessment by health care providers have not been reliable in identifying hearing loss in the first year of life. In 2000, the Joint Committee on Infant Hearing (JCIH) recommended universal screening of hearing loss before hospital discharge. The automated Auditory Brainstem Response (ABR) screening test as well as the Evoked Otoacoustic Emissions (OAE) screening test detect hearing loss in infants. The detection of hearing loss and early interventions aid the child in achieving academic and social success because they allow for the development of thinking and visual or spoken language skills. The nurse refers to the child’s chart to review the Apgar score and to determine whether or not there were any particular difficulties during the birth process. The orders left by the doctor are reviewed. The nurse must observe the newborn very closely. Respiratory distress may be indicated by the rate and character of respirations, color (the nurse observes the newborn for signs of cyanosis), and overall general behavior. Any retractions should be reported immediately. (See Complications of the Preterm Infant Respiratory System later in this chapter for a discussion on retractions.) Mucus may be seen draining from the nose or mouth. Gentle suctioning with a bulb syringe may also be indicated. See Chapter 3 to review the use of a bulb syringe. Movements of the neonate are random and uncoordinated. The newborn lacks the muscular control to hold the head up (Figure 5-12). The development of muscular control proceeds from head to foot and from the center of the body to the periphery (discussed in Chapter 4). The baby, therefore, holds up the head before sitting erect. In fact, the head and neck muscles are the first ones under control. The legs are small and short and may appear bowed. There should be no limitation of movement. Fingers clenched in a fist should be separated and observed. Circumcision is the surgical removal of the foreskin. The procedure has been subject to much controversy. Among the risks are infection and hemorrhage. Infants with congenital anomalies of the penis, such as hypospadias (occurs when the opening of the urethra is on the undersurface of the penis), should not be circumcised because the foreskin may be needed for surgery. Studies show that the risk for penile cancer and urinary tract infections are reduced in circumcised men compared with those who are uncircumcised; however, the incidence of such illness is so low that circumcision cannot be justified for prophylaxis (Hirji et al., 2005). There is also new research that indicates male circumcision has proven to be a primary prevention strategy against transmission of HIV (Uys, 2009/2010). A discussion of the pros and cons of this procedure should be included as part of the prenatal and postpartum education. The parents’ knowledge and understanding of the procedure of circumcision is necessary because a surgical consent form must be signed before this procedure can be performed. When circumcision is desired, it is performed after 12 hours of age. This period of time allows the newborn to adjust from the stress of birth and for bonding to begin. The nurse needs to advocate for the use of pain medication for babies undergoing this procedure. Analgesics and/or anesthesia should be prescribed for pain control. For the circumcision procedure, the newborn is restrained on a circumcision board. The foreskin is freed with a probe, an incision is made the length of the foreskin, and a Plastibell, Gomco clamp, or Mogen clamp (rarely used) is used to control blood loss. Excess foreskin is removed with a scalpel or a scissor (Figure 5-13). After this procedure, it is important for the nurse to observe for bleeding, irritation, and voiding. Pain is always assessed as the fifth vital sign. The skin of newborn Caucasian babies is red to dark pink in color. The skin of African-American babies may be reddish brown. Infants of Latin descent may appear to have an olive or yellowish tint to the skin. The body is usually covered with fine hair called lanugo, which tends to disappear during the first weeks of life. Lanugo is more evident in premature infants (Figure 5-14). Vernix caseosa, a cheeselike substance that covers the skin of the neonate, is made up of cells and glandular secretions and is thought to protect the skin from infection. White pinpoint pimples caused by obstruction of sebaceous glands may be seen on the nose and chin. These are called milia and disappear within a few weeks. Mongolian spots, bluish discolorations of the skin, are common in babies of African-American, Latino, Native American, or Mediterranean descent. They are usually found over the sacral and gluteal areas (Figure 5-15). They disappear spontaneously during the first years of life. Be careful not to confuse Mongolian spots with bruises that can occur from child abuse. Pallor or generalized cyanosis is not normal and should be reported.
The Newborn Infant
Introduction to the Newly Born Infant
![]() http://evolve.elsevier.com/Price/pediatric/
http://evolve.elsevier.com/Price/pediatric/
Adaptations of the Neonate
Initial Exam of the Newborn Infant
Airway
Apgar Scoring
SIGN
0
1
2
Heart rate
Absent
Slow (less than 100 beats/min.)
Above 100 beats/min.
Respiratory effort
Absent
Slow, irregular
Good; strong cry
Muscle tone
Limp
Some flexion of extremities
Well flexed
Reflex irritability
No response
Grimace
Cry or sneeze
Color
Blue, pale
Body pink, extremities bluish
Completely pink
![]() Measurements
Measurements
Vital Signs
Temperature
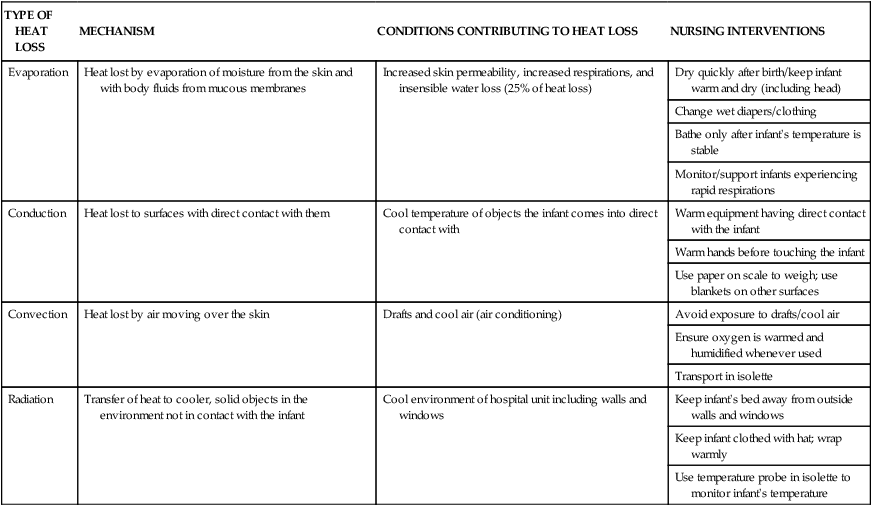
TYPE OF HEAT LOSS
MECHANISM
CONDITIONS CONTRIBUTING TO HEAT LOSS
NURSING INTERVENTIONS
Evaporation
Heat lost by evaporation of moisture from the skin and with body fluids from mucous membranes
Increased skin permeability, increased respirations, and insensible water loss (25% of heat loss)
Dry quickly after birth/keep infant warm and dry (including head)
Change wet diapers/clothing
Bathe only after infant’s temperature is stable
Monitor/support infants experiencing rapid respirations
Conduction
Heat lost to surfaces with direct contact with them
Cool temperature of objects the infant comes into direct contact with
Warm equipment having direct contact with the infant
Warm hands before touching the infant
Use paper on scale to weigh; use blankets on other surfaces
Convection
Heat lost by air moving over the skin
Drafts and cool air (air conditioning)
Avoid exposure to drafts/cool air
Ensure oxygen is warmed and humidified whenever used
Transport in isolette
Radiation
Transfer of heat to cooler, solid objects in the environment not in contact with the infant
Cool environment of hospital unit including walls and windows
Keep infant’s bed away from outside walls and windows
Keep infant clothed with hat; wrap warmly
Use temperature probe in isolette to monitor infant’s temperature
![]() Heart Rate and Blood Pressure
Heart Rate and Blood Pressure
Weight and Gestational Age
Maturity
Characteristics of the Newborn Infant
![]() Head
Head
Nervous System
![]() Reflexes
Reflexes
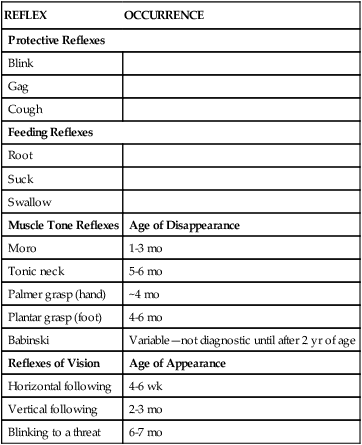
REFLEX
OCCURRENCE
Protective Reflexes
Blink
Gag
Cough
Feeding Reflexes
Root
Suck
Swallow
Muscle Tone Reflexes
Age of Disappearance
Moro
1-3 mo
Tonic neck
5-6 mo
Palmer grasp (hand)
~4 mo
Plantar grasp (foot)
4-6 mo
Babinski
Variable—not diagnostic until after 2 yr of age
Reflexes of Vision
Age of Appearance
Horizontal following
4-6 wk
Vertical following
2-3 mo
Blinking to a threat
6-7 mo

Sensory System
Hearing
Circulatory and Respiratory System
Musculoskeletal System
Movements and Tremors
Genitourinary System
![]() Male Genitalia
Male Genitalia
Integumentary System
![]() Skin
Skin

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Newborn Infant
Get Clinical Tree app for offline access