The medical assistant should sit with the back supported and the head in a neutral position (not forward or to one side). The feet should be flat on the floor or supported on a foot stool. Figure 39-1 shows proper body position for answering the telephone. If the receiver is tucked between the head and shoulder, it places strain on the shoulder muscles and may change the voice quality, so this should be avoided. A headset, which consists of an earpiece that fits over the ear and a mouthpiece in front of the mouth, allows for good body posture and leaves the hands free. This is recommended if the medical assistant spends a lot of time on the telephone. Figure 39-2 shows such a headset. Most offices have a multiline phone, with several extensions. It is important for the medical assistant to learn how to determine which line is ringing, how to place calls on hold, and how to transfer calls to all parts of the medical office. Figure 39-3 illustrates a multiline telephone with many extensions. Speed dialing allows storage of frequently called telephone numbers in the telephone system’s memory. These numbers can be called by pressing a button or a one- or two-digit code. Call forwarding allows forwarding of incoming calls to another telephone number. This service is turned on and off by dialing a sequence of numbers and activity keys. Call park allows a call to be placed on hold and retrieved from another telephone. Caller ID identifies the caller’s telephone number before the telephone is answered. This feature may be available on some, but not all, telephones within a telephone system. • Calls from other physicians are put through at once. • Emergency calls are treated as urgent and receive top priority. They will be discussed in detail later in this chapter. • If the caller is a relative of the physician, the medical assistant either puts the caller through or speaks to the physician via intercom to determine how to handle the call. After the caller’s name has been obtained, the caller usually states the reason for the call or asks for a staff member or department. When the caller asks for a staff member by name, the medical assistant usually transfers the call. If that staff member is with a patient, the medical assistant may offer to take a message or transfer the call to voicemail. Often the caller asks for the physician. Most physicians do not take calls while they are seeing patients. Additional questions may show that the medical assistant can handle the call, or it may be necessary to take a message for the physician (Procedure 39-1).
Telephone Techniques
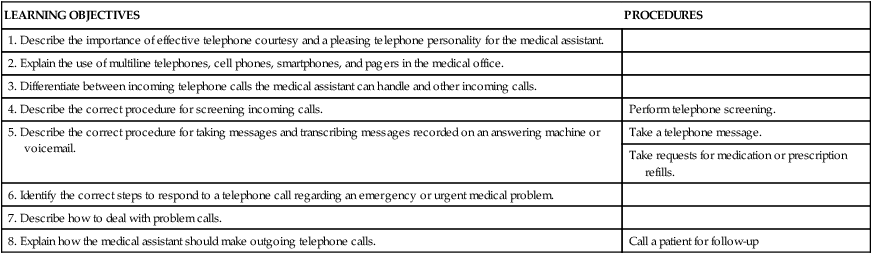
LEARNING OBJECTIVES
PROCEDURES
1. Describe the importance of effective telephone courtesy and a pleasing telephone personality for the medical assistant.
2. Explain the use of multiline telephones, cell phones, smartphones, and pagers in the medical office.
3. Differentiate between incoming telephone calls the medical assistant can handle and other incoming calls.
4. Describe the correct procedure for screening incoming calls.
Perform telephone screening.
5. Describe the correct procedure for taking messages and transcribing messages recorded on an answering machine or voicemail.
Take a telephone message.
Take requests for medication or prescription refills.
6. Identify the correct steps to respond to a telephone call regarding an emergency or urgent medical problem.
7. Describe how to deal with problem calls.
8. Explain how the medical assistant should make outgoing telephone calls.
Call a patient for follow-up
Introduction to Telephone Techniques
Using the Telephone Effectively
Telephone Courtesy
Effective Telephone Communication

Telephone Technology
Multiline Phones
Special Features
Incoming Calls
Managing Incoming Calls
Performing Telephone Screening

Telephone Techniques
Get Clinical Tree app for offline access