Safety
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe accident risk factors.
• Explain why you identify a person before giving care.
• Explain how to correctly identify a person.
• Describe the safety measures to prevent burns, poisoning, and suffocation.
• Identify the signs and causes of choking.
• Explain how to prevent equipment accidents.
• Explain how to handle hazardous chemicals.
• Identify natural and human-made disasters.
• Describe fire prevention measures and oxygen safety.
• Explain what to do during a fire.
• Explain how to protect yourself from workplace violence.
• Describe your role in risk management.
• Perform the procedures described in this chapter.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Key Abbreviations
| AED | Automated external defibrillator |
| C | Centigrade |
| CDC | Centers for Disease Control and Prevention |
| CMS | Centers for Medicare & Medicaid Services |
| CO | Carbon monoxide |
| CPR | Cardiopulmonary resuscitation |
| EMS | Emergency Medical Services |
| F | Fahrenheit |
| FBAO | Foreign-body airway obstruction |
| HCS | Hazard Communication Standard |
| ID | Identification |
| MET | Medical Emergency Team |
| OSHA | Occupational Safety and Health Administration |
| PASS | Pull the safety pin, aim low, squeeze the lever, sweep back and forth |
| RACE | Rescue, alarm, confine, extinguish |
| RRT | Rapid Response Team |
| SDS | Safety data sheet |
Safety is a basic need. Patients and residents are at great risk for accidents and falls. (See Chapter 14 for falls.) Some accidents and injuries cause death.
The health team must provide for safety. This includes you. Common sense and simple safety measures can prevent most accidents. Sometimes extraordinary measures are needed. You must protect patients, residents, visitors, co-workers, and yourself. The safety measures in this chapter apply to all health care settings and everyday life.
The goal is to decrease the person’s risk of accidents and injuries without limiting mobility and independence. The care plan lists other safety measures for the person. Measures to promote safety must not interfere with the person’s rights (Chapter 2).
A Safe Setting
In a safe setting, a person has little risk of illness or injury. The person’s setting is free of hazards to the extent possible. The person feels safe and secure physically and mentally. The risk for infection, falls, burns, poisoning, and other injuries is low. Temperature and noise levels are comfortable. Smells are pleasant. There is enough room and light to move about safely. The person and the person’s property are safe from fire and intruders. The person is not afraid and has few worries and concerns.
The person must receive the right care and treatment. To protect the person from harm, follow the person’s care plan. Also practice the safety measures in this chapter.
See Teamwork and Time Management: A Safe Setting.
Accident Risk Factors
Some people cannot protect themselves. They present dangers to themselves and others. They rely on others for safety. Certain factors increase the risk of accidents and injuries. Follow the person’s care plan.
• Age. Children and older persons are at risk for injuries. See Focus on Children and Older Persons: Accident Risk Factors (Age).
• Awareness of surroundings. People need to know their surroundings to protect themselves from injury. Confused and disoriented persons may not understand what is happening to and around them. A coma can occur from illness or injury. Coma is a state of being unaware of one’s setting and being unable to react or respond to people, places, or things.
• Impaired mobility. Some diseases and injuries affect mobility. A person may know there is danger but cannot move to safety. Some persons cannot walk or propel wheelchairs. Some persons are paralyzed.
• Paralysis means loss of muscle function, sensation, or both.
• Paraplegia is paralysis in the legs and lower trunk. (Para means beyond. Plegia means paralysis.)
• Quadriplegia (tetraplegia) is paralysis in the arms, legs, and trunk. (Quad and tetra mean 4. Plegia means paralysis.)
• Hemiplegia is paralysis (plegia) on 1 side (hemi) of the body.
Identifying the Person
Each person has different treatments, therapies, and activity limits. Life and health are threatened from the wrong care.
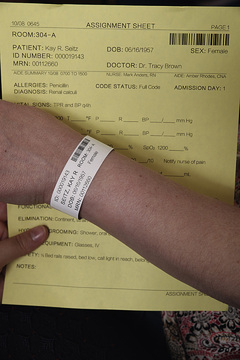
The person may receive an identification (ID) bracelet when admitted to the agency (Fig. 13-1). The bracelet has the person’s name, room and bed number, birth date, age, doctor, and other identifying information.

You use the bracelet to identify the person before giving care. Your assignment sheet states what care to give. To identify the person:
• Compare identifying information on the assignment sheet with that on the ID bracelet (Fig. 13-2). Carefully check the information. Some people have the same first and last names. For example, John Smith is a very common name.
See Focus on Communication: Identifying the Person.
See Focus on Long-Term Care and Home Care: Identifying the Person.
See Promoting Safety and Comfort: Identifying the Person.
Preventing Burns
Burns are a leading cause of death among children and older persons. Smoking, spilled hot liquids, children playing with matches, barbecue grills, fireplaces, and stoves are common causes. So are electrical items and very hot water (sinks, tubs, showers). The safety measures in Box 13-1 can prevent burns.
Burn severity (Chapter 54) depends on water temperature and length of exposure (Table 13-1). The person’s condition is also a factor.
TABLE 13-1
Temperature and Time for a Third Degree Burn
| Fahrenheit (F) | Centigrade (C) | Time Required for a Third Degree Burn to Occur |
| 155°F | 68°C | 1 second |
| 148°F | 64°C | 2 seconds |
| 140°F | 60°C | 5 seconds |
| 133°F | 56°C | 15 seconds |
| 127°F | 52°C | 1 minute |
| 124°F | 51°C | 3 minutes |
| 120°F | 48°C | 5 minutes |
| 100°F | 37°C | Usually a safe temperature for bathing |
See Focus on Children and Older Persons: Preventing Burns.
Preventing Poisoning
A poison is any substance harmful to the body when ingested, inhaled, injected, or absorbed through the skin. If too much is taken, any substance can be poisonous. Poisonings are intentional or unintentional.
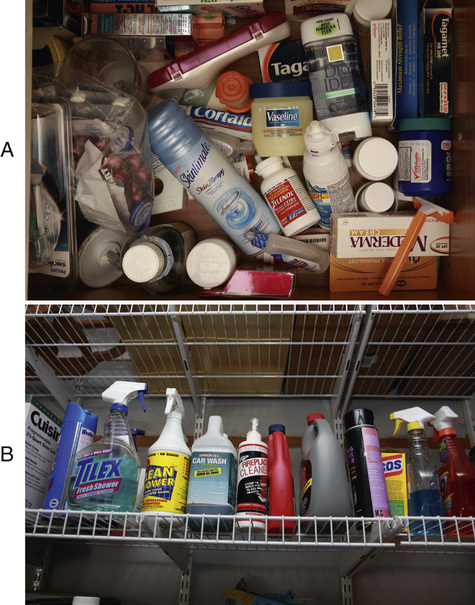
Poisoning can cause illness, brain damage, coma, and death. Children and older persons are at risk. Drugs and household products are common poisons. Poisoning in adults may be from carelessness, confusion, or poor vision when reading labels. As a result, a person may take too much of a drug.
Common poisons include:
• Drugs (legal and illegal) and vitamins
• Fertilizers, insecticides, bug sprays, and so on
• Alcohol
The measures in Box 13-2 (p. 160) can prevent poisoning.
See Focus on Long-Term Care and Home Care: Preventing Poisoning.
See Promoting Safety and Comfort: Preventing Poisoning, p. 161.
Lead Poisoning
Lead is a metal. When in the body, it affects normal body functions. A very strong poison, it can injure the brain, nervous system, red blood cells, kidneys, liver, teeth, and bones. It can lower intelligence and cause learning and behavior problems. See Box 13-3, p. 162, for the sources of lead poisoning.
Lead enters the body through:
Children between the ages of 6 months and 6 years are at risk for lead poisoning. Lead can affect almost every body system. Signs and symptoms are usually gradual in onset. They are not always obvious. See Box 13-3 for signs, symptoms, and safety measures.
See Focus on Long-Term Care and Home Care: Lead Poisoning.
Carbon Monoxide Poisoning
Carbon monoxide (CO) is a deadly colorless, odorless, and tasteless gas. It is produced by the burning of fuel—gas, oil, kerosene, wood, charcoal (Box 13-4, p. 163). Fuel-burning devices must work properly and must be used correctly. Otherwise, dangerous levels of CO can build up in closed or semi-closed areas. Instead of breathing in oxygen, the person breathes in air filled with CO. Red blood cells pick up CO faster than oxygen. Oxygen does not get into the body. CO can quickly or slowly kill. If not fatal, brain and nervous system damage can result.