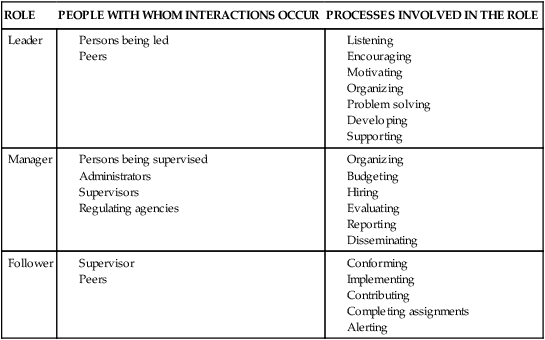
• Construct the full scope of a manager role by outlining Responsibilities, Opportunities, Lines of communication, Expectations, and Support (ROLES). • Analyze specific examples of role transitions as a staff nurse and a nurse manager. • Describe the phases of role transition by using a life experience. • Construct a response to an unexpected role transition. • Compare strategies to facilitate a successful role transition. Role transition involves transforming one’s professional identity. A new graduate makes a transition from the student role to the nurse role. Expectations of students are clearly specified in course and clinical objectives. Expectations for a new nurse as an employee may not be so clear. The new graduate nurse faces the first of several professional transitions. The Literature Perspective and Research Perspectives on p. 539 provide further information on role transitions for new graduate nurses, which are helpful for new graduates, their co-workers, and their managers. Organizations play a key role in assisting employees through role transitions. Changes in roles can be either painful or exciting and depend largely on the work culture and support provided. According to Sewell (2008), “role transition is a hurdle encountered by every nurse entering the workforce. A host of new experiences await the neophyte beyond the clinical experiences of nursing school” (p. 49). Accepting a management position dictates accepting three roles that involve complex processes. The roles of leader, manager, and follower are complex because they involve working through and with unique individuals in a rapidly changing environment. Examples of the people with whom you interact and the processes involved in each role are shown in Table 27-1. In nursing, each of these roles relates to patients and clients. TABLE 27-1 The transition from a staff nurse role to a nurse manager/leader role can occur overnight. The nurse moves from the clinical work of patient care to lead a group of employees. Clark (2008) notes that “leadership is not simply granted to individuals and is not about responding passively to events. It is about creating possibilities that were absent before” (p. 30). McConnell (2008) says that a healthcare professional who takes on a manager position is taking on a second occupation. “The professional who enters management must wear two hats” (p. 278). One role is as the professional on technical and clinical matters, and one is as a generalist manager. Acronyms help us retain and organize information. “ROLES” (Box 27-1) is an acronym that is useful in role transition. L represents lines of communication, which are at the heart of every leadership role. No matter what role an individual is in, there are relationships with multiple individuals including supervisors and peers. Roles incorporate patterns of structured interactions between the manager and people in these groups. The nurse manager receives and sends messages. Being a skillful listener can be more important than being skillful in sending messages. Skill is required to communicate both the content and the intent of the message effectively. Only through practice can one develop skill. In Chapter 18, techniques of effective communication are described that are extremely important to a new manager in building the team. Finding out in advance what the explicit and implicit expectations are of the people involved can facilitate a smoother role transition by decreasing role ambiguity (Hardy, 1978). Hardy’s work with role theory suggests a strong relationship between role ambiguity (one type of role stress) and role strain. The major concepts of role theory are presented in the Theory Box above.
Role Transition
Introduction
Types of Roles
ROLE
PEOPLE WITH WHOM INTERACTIONS OCCUR
PROCESSES INVOLVED IN THE ROLE
Leader
Manager
Follower
Roles: The ABCs of Understanding Roles
Role Transition
Get Clinical Tree app for offline access




