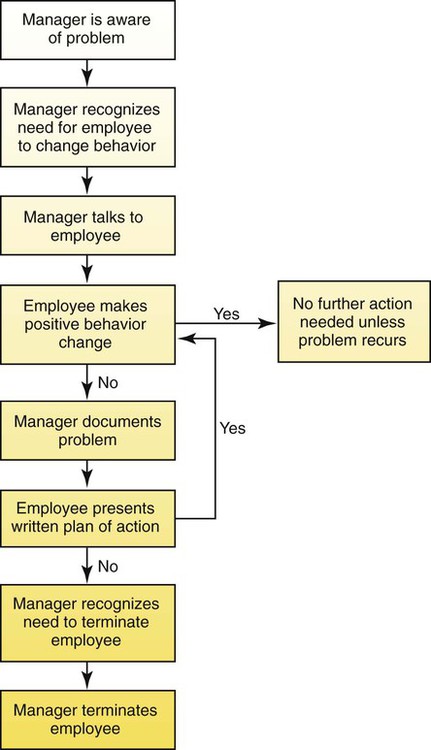
• Differentiate common personal/personnel problems. • Relate role concepts to clarification of personnel problems. • Examine strategies useful for approaching specific personnel problems. • Prepare specific guidelines for documenting performance problems. • Value the leadership aspects of the role of the novice nurse. One of the most vexing personnel problems is that of absenteeism. Inadequate staffing adversely affects patient care both directly and indirectly. When an absent caregiver is replaced by another who is unfamiliar with the routines, employee morale suffers and care may not meet established standards. Working with inadequate staffing or working overtime to cover for absent workers creates physical and mental stress. Replacement personnel usually need more supervision, which not only is costly but also may decrease productivity and the quality of patient care. Indirectly, co-workers may become resentful about being forced to assume heavier workloads and/or may be pressured to work extra hours. Chronic absenteeism may lead to increased staff conflicts, to decreased morale, and eventually to increased absenteeism among the entire staff. Given that nurses prefer to avoid conflict and negative behavior and to accommodate or make excuses for these situations (Sportsman, 2005), one way to confront persistent absenteeism is to discuss the situation directly with the employee (also see Chapter 18) by verbalizing: • “I feel concerned when I see that you have been absent 3 days this month.” • “Can you see how excessive absences affect the smooth functioning of the unit, the work load of other team members, and the safety of patients?” • “This rate of absences cannot continue. What is your plan for addressing this situation?” Absenteeism cannot be totally eliminated. There are always unplanned illnesses, accidents, bad weather, sick family members, a death in the family, and even jury duty, which are legitimate reasons for missing work and beyond the control of management. However, some portion of absenteeism is voluntary and preventable; thus the cause must be identified so that it may be addressed. Wallace (2009) identified issues leading to absenteeism including personal situations such as sick dependent family members, poor health, job stress or high work demands such as long hours, excessive workload, lack of control over work, and poor support from managers. These stressors lead to a poor work environment and lower the morale of fully engaged nurses. Absenteeism may also indicate poor work satisfaction. Dissatisfied staff may in fact be completely disengaged, which can lead to increased absences. If the leader believes that the issue is attributable to work dissatisfaction, unit-based discussions may lead to insight about the sources. Such discussions provide an excellent opportunity for the novice nurse to listen, to learn, and to speak to issues. If the underlying cause can be identified, there may be a way to prevent the loss of the dissatisfied employee if retention is the goal. Some employees who convey that they are never happy with their jobs may continually disrupt the overall unit with their absenteeism and should be terminated. The Evidence section on p. 494 illustrates some of those factors to consider. With role theory as a framework, absenteeism has been linked to role stress and role strain. Absence from work is a way of withdrawing from an undesirable situation short of actually leaving, and many employees increase their absenteeism just before submitting their resignation. If the healthcare worker is experiencing some form of role stress, it might be manifested through absenteeism. Role strain may be reflected by (1) withdrawal from interaction; (2) reduced involvement with colleagues and the organization; (3) decreased commitment to the mission and the team; and (4) job dissatisfaction. All of these could be manifested through absenteeism. With this framework, management of absenteeism is based on the belief that competent role performance requires interpersonal competence. “Role competence is the ability of a person in an interdependent position, which is ongoing in time, to carry out lines of action that are task and interpersonally effective” (Hardy & Conway, 1988, on p. 195). Role behavior occurs in a social context rather than in isolation. Therefore the nurse leader needs to understand the existing situation, when the situation changed to its current status, when it needs to change further, and how to accomplish such change. Because people who are more satisfied in their work usually commit to “be there” for their team, enhancing job satisfaction may be an effective strategy toward reducing absenteeism. One model for nonpunitive discipline can be found in Figure 24-1. This model demonstrates how undesirable behaviors, such as absenteeism, can be successfully altered. Box 24-1 identifies specific steps that are involved in nonpunitive discipline. This model of nonpunitive discipline allows employees to free themselves from some role stress by clarification of role expectations and assumptions. Employees can receive satisfaction from the realization that a problem may not be inadequate performance caused by personal faults but, rather, a lack of clarification of role expectations within the organization. Novice nurses may be called on to implement the process described in Box 24-1. For example, the novice nurse may be involved with the nurse manager or a support staff member or, in extenuating circumstances, the new nurse may be directly involved in the process. Remember, the focus is on the clear understanding of the situation, the growth of the individual, and the smooth and effective functioning of the team. The problem of uncooperative or unproductive employees is another area of frustration for the nurse leader. Hersey, Blanchard, and Johnson (2008) identified two major dimensions of job performance that relate to this problem: motivation and ability. The type and intensity of motivation vary among employees because of differing needs and goals that employees express. The leader can best handle employees with motivation problems by attempting to determine the cause of the problem and by working to provide an environment that is conducive to increased motivation for the employee. If the employee is uncooperative or unproductive because of a lack of ability, education and training are appropriate interventions. Sometimes an unproductive employee simply lacks maturity. This lack of maturity may be described as emotional intelligence underdevelopment that results in such problems as being socially inept or unable to control one’s impulses (Strickland, 2000). The management tips column in Health Care Manager describes this situation in “Case in Health Care Management: Managing the Drama Queen” (2004). These employees are frequently defensive and emotional or tearful. They lack self-insight into their behavior. Sometimes immaturity in an employee may not be readily apparent to the leader but may be manifested in any of the following actions: defiance, testing of workplace guidelines, passivity or hostility, or little appreciation for any management decisions. The challenge for the nurse leader is not to react in kind but, rather, to relate to this employee in a positive and mature manner. A sense of humor and the ability to tease the employee into a more receptive, jovial mood are sometimes helpful. However, the leader needs to determine whether the undesirable behaviors are reflecting a state of being uncomfortable or incompetent (LaDuke, 2000). For example, if an employee states, “Administration is always making decisions to make our jobs harder,” rather than making a hostile or defensive comment in reply, the manager could take the employee aside and say, “I notice that you seem to be angry about this new policy. Let’s talk about it some more.” Immature employees either act immaturely all of the time or regress to an immature level when stressed. The nurse leader must recognize immaturity in an employee and react calmly and without anger. The leader must keep in mind that this employee may be displaying dynamics rooted in unresolved personal areas and that the behavior is not a personal attack on the leader. The best way to deal with this behavior is to confront the employee with the specific problem and define realistic limits of acceptable behavior with consequences for nonadherence. Generally, employees comply with specific limits but will test management in other areas. As this testing occurs, the leader must continue the same limit-setting technique. Remember that the immature employee usually has problems because of a lack of self-worth, power, and self-control. Praise and affirmation are valuable tools that the leader can use to help these employees feel better about themselves. Chapter 3 addresses generational issues if they are factors to consider. Most healthcare agencies use skills checklists or a competency evaluation program to ascertain that their employees have and maintain essential skills for the job they are expected to do. A skills checklist is one way to determine basic clinical competency (Table 24-1). This checklist typically contains a number of basic skills along with ones that are essential for safe functioning in the specific area of employment. Any type of skills review should be directly linked to quality-improvement indicators. The employee may be asked to do a self-assessment of the listed skills or competencies and then have performance of the skills validated by a peer or co-worker. This is a very effective method for the leader to assess the skill level of employees and to determine where additional education and training may be necessary. In addition, if the leader discovers that an employee cannot perform a skill adequately, the skills list can easily be checked and directly observed behaviors can be assessed to determine at what level the employee is functioning. At the completion of the assessment, a specific plan for remediation can be developed. Sometimes, an employee may be able to perform all of the tasks on a skills checklist but still cannot manage overall patient care effectively. If, in questioning the employee or in evaluating the employee’s performance, the manager/leader determines that there is a lack of knowledge or that there are problems with time management, formal education may be the proper course of action. In either event, the leader must establish a written contract containing a plan of action that sets time limits within which certain expectations must be achieved. This ensures compliance on the part of the employee. A more comprehensive program for competency evaluation might include not only the skills checklist but also unit-specific objectives, an overall framework for evaluation, and critical-thinking exercises that are interactive in nature (Johnson, Opfer, VanCura, & Williams, 2000). The role of the novice nurse leader, particularly with ancillary personnel, is to support the nurse manager as well as be helpful and supportive of the team members who are striving to improve. TABLE 24-1
Managing Personal/Personnel Problems
Personal/Personnel Problems
Absenteeism
Uncooperative or Unproductive Employees
Immature Employees
Clinical Incompetence




