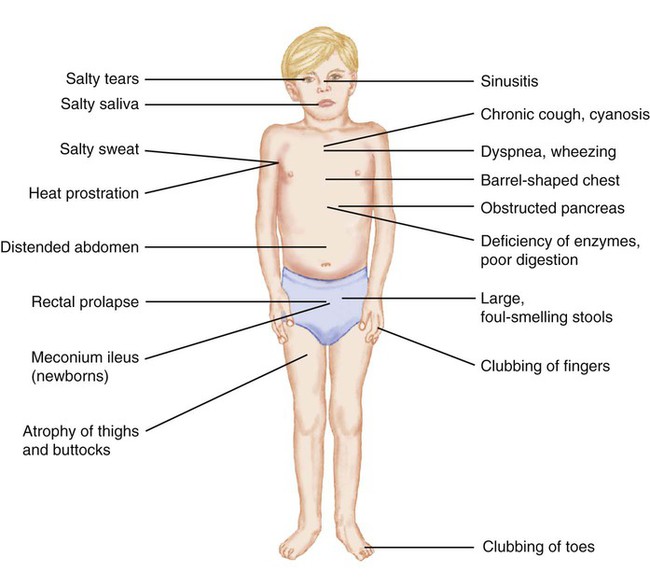
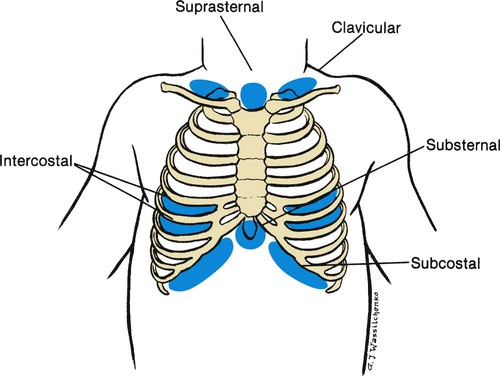
1. Define the vocabulary terms listed 2. List the differences found in the respiratory system of a child, and identify potential risks 3. Develop a teaching plan for the parents of a newborn regarding SIDS prevention 4. Illustrate the anatomic difference in the ear canals of adults and children, and describe the significance of this difference along with nursing care for a child with otitis media 5. Summarize the nursing care for an infant with bronchiolitis 6. Explain the dietary needs for a child with cystic fibrosis 7. Outline the nursing observation and care necessary for a 2-year-old child with croup 8. Describe the nursing care for a child undergoing surgery for removal of tonsils and adenoids 9. Describe the nursing care of the child with asthma, including monitoring of respiratory status, respiratory treatments and medications, and the psychosocial implications of the condition 10. Discuss the important nursing care of a child with tuberculosis The respiratory system consists of the nose, pharynx, and larynx (upper respiratory tract) and the trachea, bronchi, and lungs (lower respiratory tract). The respiratory tract continually changes during the first 12 years of a child’s life. There are several anatomic differences that predispose children to respiratory difficulties (Box 11-1). This makes respiratory problems common during childhood. Most problems are mild and can be managed at home. Other conditions can be chronic and have an impact on the growth and development of the child. Respiratory distress and failure are the common factors for cardiac arrest in children. Respiratory diseases account for 25% of hospitalizations for children younger than 15 years of age. Pneumonia accounts for 31%, bronchiolitis and bronchitis for 25%, and asthma for 25% of the respiratory diseases (CDC, 2007). Children with respiratory difficulties have common signs and symptoms that can progress to respiratory failure if not recognized. Assessment findings of the child’s respiratory system will vary depending on the age of the child. The nurse must recognize any change in the child’s breathing status. Signs and symptoms may include fever, anorexia, vomiting, diarrhea, abdominal pain, nasal blockage, nasal drainage, cough, sore throat, retractions, and abnormal respiratory sounds. Respiratory assessment should be comprehensive and frequent as the status can change rapidly. The assessment should include the guidelines shown in Box 11-2. Retractions can indicate respiratory distress. The severity of respiratory distress can be assessed using the depth and location of the retractions (Figure 11-1). In dealing with grieving parents after the death of their infant, the nurse must convey some important facts: that the baby died of a disease entity called SIDS, that this disease currently cannot be predicted or prevented, and that they are not responsible for the child’s death. Grieving parents need time to say good-bye to their child. They should be encouraged to hold and rock their infant, shed tears, and assist in burial preparations. This process, not common in the past, is conducive to the resolution of grief (see also Chapter 22). One mother who was denied this experience stated that 5 years later, while visiting a florist’s shop, she noticed a heart-shaped wreath intended for an infant. She unexpectedly burst into tears and wept. Bronchopulmonary dysplasia (BPD) is a chronic lung disease that occurs in newborns that are premature or have pulmonary disorders that require mechanical ventilator support with high positive pressure and oxygen. The lung tissue is immature and unable to withstand tissue damage resulting from the required oxygen supplement. The resulting fibrosis and alteration in lung compliance may last from several months to years. Improvements in treatment of low–birth weight preterm infants have increased the incidence of this disorder, and continue to be the primary issue for infants younger than 27 weeks of age (Belcastro, 2004). Newer mechanical ventilators are being used for low birth weight neonates in hopes of decreasing BPD. Parents may be extremely anxious caring for a child with BPD. All equipment and procedures should be explained in simple terms. Children with tracheostomies can be cared for in the home setting, and home care teaching of the equipment is needed (Figure 11-2). Review care of the child with tracheostomy in Chapter 3. Extended hospitalization can interfere with the development of the normal parent-child relationship and with the normal development of the infant. Parental participation in the infant’s care should be encouraged. The family’s ability to cope and care for a child with a chronic illness needs to be evaluated as home discharge plans are developed. An adequate period of education may be necessary for the parents to become comfortable with the care required for their child. Families should be referred to social services to assist in providing additional support and to assist in helping the parent gain access to available community services. Parental support groups can be beneficial in providing additional assistance with coping skills necessary for caring for a child with complex care. New treatment guidelines were released in 2004 by the American Academy of Pediatrics (AAP) (Box 11-4). Treatment included an observation option, pain management, and antimicrobial treatment. Development of resistant strains of bacteria and misuse of antimicrobials assisted in the development of new guidelines. When antimicrobials are used, amoxicillin remains the drug of choice, but recurrent infections may require other antimicrobials. Parents are taught to give the entire dose of the antimicrobial even though the child may appear well. Parents will need to understand the new course of treatment using the guidelines and their role in the management of AOM. When the child is hospitalized, intravenous fluids are started to hydrate the child and thin the secretions. The child is placed in an atmosphere of humidified oxygen (mist tent, croupette, or nasal cannula/mask). The goal is to keep oxygen levels at 92% or better with a pulse oximeter. With severe bronchiolitis, the physician may use a bronchodilator and a corticosteroid, but these remain controversial (Zorc, 2010). Antimicrobials may also be used for small or severely ill infants because these infants may be susceptible to a secondary bacterial infection. Fever is controlled with antipyretics. A laboratory study of a nasopharyngeal washing should be done to determine whether the causative organism is RSV. As a precautionary measure for the safety and concern of other children, the infant is placed in contact isolation until RSV has been ruled out. When the causative organism is RSV, no medications can effectively treat the disease. Ribavirin, antimicrobials, antihistamines, and oral decongestants have been identified as being ineffective for treatment (Zorc, 2010). Medical attention has recently focused on active and passive immunizations. RSV-immune globulin (RespiGam) and palivizumab (Synagis) have been approved for use with children at high risk. Palivizumab may be preferred because of ease of administration (intramuscular); lack of interference with mumps, measles, and rubella (MMR) vaccine and varicella vaccine; and lack of complications associated with intravenous immune globulin (RespiGam). Monthly administration during RSV season (October to May) is recommended (AAP, 2009). Nursing diagnoses for the infant with bronchiolitis include the following: • Ineffective airway clearance, related to thick mucus • Impaired gas exchange, related to edema and mucus of the bronchioles • Deficient fluid volume, related to insensible fluid loss from tachypnea and decreased intake • Anxiety, related to unfamiliar environment, respiratory distress, and placement in croupette • Knowledge deficit, related to disease process and treatment Formula-fed infants may have thickened feeding to improve swallowing dysfunction and to prevent aspiration. Breastfed infants should have more frequent feeding with shorter times. This assists in decreasing the workload of the infant and conserves energy. Nasal secretions should be removed with a bulb syringe before feedings (Allen, 2006). The child in a mist tent should have the gown and linens changed if they become damp. Also, moisture buildup should be removed from the tubing and the sides of the tent (see Chapter 3 for detailed care of the child in a mist tent). For home care, cold air humidifiers can be used but must be cleaned properly to prevent bacteria or fungal growth. The major symptoms of CF are manifested in the respiratory tract and the GI tract. The first symptom may be seen in the newborn infant who has a meconium ileus. This condition is seen in approximately 10% to 20% of children who are born with CF. An overview of the manifestations of CF is shown in Figure 11-3.
Respiratory Disorders
Respiratory System
![]() http://evolve.elsevier.com/Price/pediatric/
http://evolve.elsevier.com/Price/pediatric/
Sudden Infant Death Syndrome
Bronchopulmonary Dysplasia
Treatment and Nursing Care
Otitis Media
Treatment and Nursing Care
Bronchiolitis
Treatment
Nursing Care
Cystic Fibrosis
Signs and Symptoms