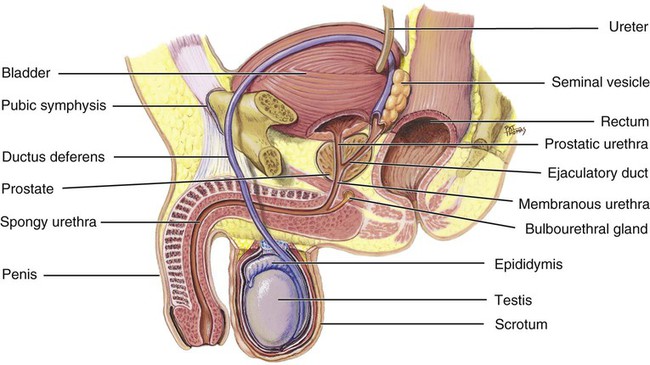
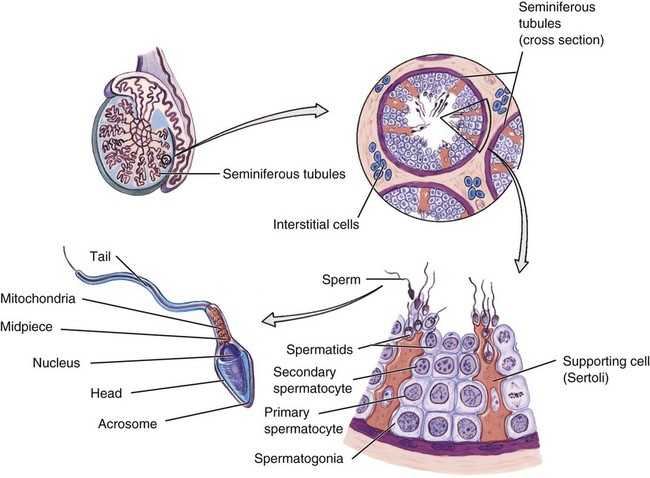
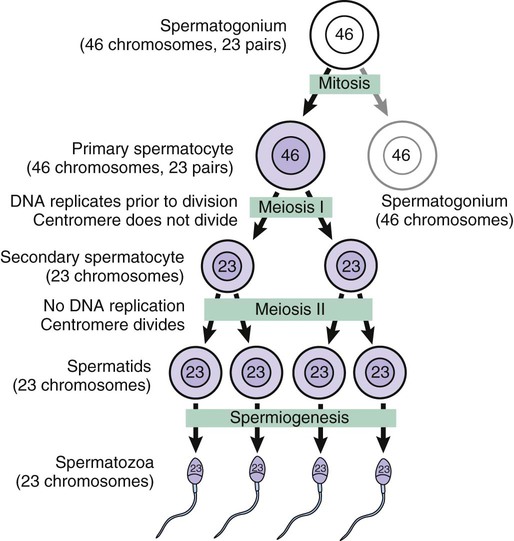
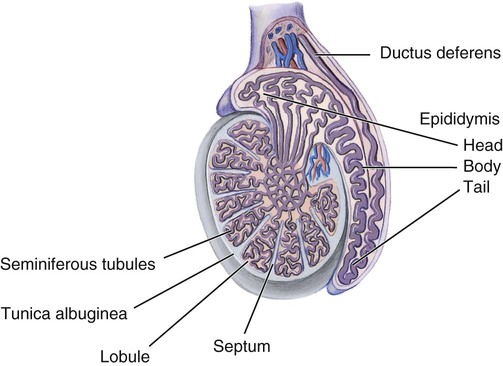
1. Distinguish between primary and secondary reproductive organs. 2. Describe the location and structure of each component of the male reproductive system. 3. Explain the process by which spermatids become mature sperm. 4. Trace the pathway of sperm from the testes to the outside of the body. 5. Outline the physiologic events in the male sexual response. 6. Describe the roles of gonadotropin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and testosterone in male reproductive functions. 7. Identify each component of the female reproductive system, including the mammary glands. 9. Describe the development of ovarian follicles. 10. Outline the physiologic events in the female sexual response. 11. Describe the roles of GnRH, FSH, LH, estrogen, and progesterone in female reproductive functions. 12. Describe what happens in each phase of the ovarian and uterine cycles, when each phase occurs, and how the cycles interact. 13. Describe ways in which the aging of an individual affects the reproductive system. • To produce egg and sperm cells • To transport and sustain these cells • To nurture the developing offspring The male reproductive system produces, sustains, and transports sperm; introduces the sperm into the female vagina; and produces hormones. Figure 16-1 illustrates the organs of the male reproductive system. Each testis is an oval structure about 5 cm long and 3 cm in diameter (Figure 16-2). A tough, white fibrous connective tissue capsule, known as the tunica albuginea (TOO-nik-ah al-byoo-JIN-ee-ah), surrounds each testis. The tunica albuginea extends inward to form septa that partition the testis into lobules. Each testis contains about 250 lobules. Each lobule contains one to four highly coiled seminiferous (seh-mye-NIFF-er-us) tubules that converge into a series of duets that exit the testes and enter the epididymis. Interstitial cells (cells of Leydig) are located between the seminiferous tubules within a lobule. Interstitial cells produce male sex hormones. Sperm are produced within the seminiferous tubules. The process of sperm formation is known as spermatogenesis (spur-mat-oh-JEN-eh-sis), which is a form of meiosis. The seminiferous tubules are packed with cells in various stages of spermatogenesis (Figure 16-3). Interspersed with these cells are large cells that extend from the periphery of the tubule to the lumen. These large cells are the supporting cells (Sertoli cells), which support and nourish the other cells. Each primary spermatocyte goes through the first meiotic division (meiosis I) to produce two secondary spermatocytes. In the second meiotic division (meiosis II), each secondary spermatocyte divides to produce two spermatids. As a result of the two meiotic divisions, each primary spermatocyte produces four spermatids (Figure 16-4). During spermatogenesis there are two cellular divisions but only one replication of DNA, so each spermatid has 23 chromosomes (haploid), one from each pair in the original primary spermatocyte. Each successive stage in spermatogenesis is pushed toward the center of the tubule. This results in the more immature cells being at the periphery, and the more differentiated cells are nearer the center (see Figure 16-3). Spermatogenesis (and oogenesis in the female) differs from mitosis (review Chapter 5) because the resulting cells have only half the number of chromosomes as the original cell. When the sperm cell nucleus unites with an egg cell nucleus, the full number of chromosomes is restored. If sperm and egg cells were produced by mitosis, then each successive generation would have twice the number of chromosomes as the preceding one. The final step in the development of sperm is called spermiogenesis (spur-mee-oh-JEN-eh-sis). In this process, the spermatids formed from spermatogenesis become mature spermatozoa, or sperm. The mature sperm cell has a head, midpiece, and tail (see Figure 16-3). The head contains the 23 chromosomes surrounded by a nuclear membrane. The tip of the head is covered by an acrosome (AK-roh-sohm). The acrosome contains enzymes that help the sperm penetrate the female gamete. The midpiece contains mitochondria that provide adenosine triphosphate (ATP). The tail, also called the locomotor region, is a typical flagellum for locomotion. The sperm are released into the lumen of the seminiferous tubule, where they leave the testes and enter the epididymis. In the epididymis the sperm undergo final maturation and become capable of fertilizing a female gamete. Sperm leave the testes through a series of ducts that enter the epididymis (ep-ih-DID-ih-mis) (see Figure 16-2). The epididymis is a long tube that is tightly coiled to form a comma-shaped organ. When the sperm leave the testes, they are immature and incapable of fertilizing ova. They complete their maturation process and become fertile as they move through the epididymis. Mature sperm are stored in the lower portion of the epididymis. The ductus deferens (also called vas deferens) is a tube that is continuous with the epididymis (see Figure 16-2). The ductus deferens enters the abdominopelvic cavity, then descends along the posterior wall of the bladder toward the prostate gland (see Figure 16-1). Sperm are stored in the ductus deferens, near the epididymis, and peristaltic movements propel the sperm through the tube.
Reproductive System
Introduction to the Reproductive System
Male Reproductive System
Testes
Structure
Spermatogenesis
Duct System
Epididymis
Ductus Deferens
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Reproductive System
Get Clinical Tree app for offline access