Chapter 2 Pulmonology
Basic concepts—mechanics of breathing
2 What are the forces of resistance for the following:
Tissue resistance is generated as the pleural surfaces slide over each other during respiration. This resistance is normally minimal because of the presence of pleural fluid. Note that tissue resistance can increase markedly in conditions in which the pleural surfaces become adherent to each other, as may occur with an empyema (Fig. 2-1).
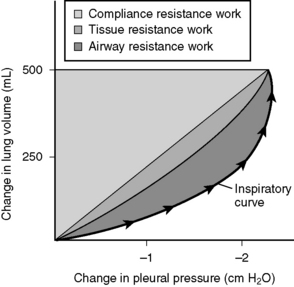
Figure 2-1 Relative contributions of the three types of resistance to the total work of breathing.
(From Brown TA: Rapid Review Physiology. Philadelphia, Mosby, 2007.)
4 With respect to the compliance curve of the lungs, how might breathing at an elevated functional residual capacity in chronic obstructive pulmonary disease result in less “efficient” breathing?
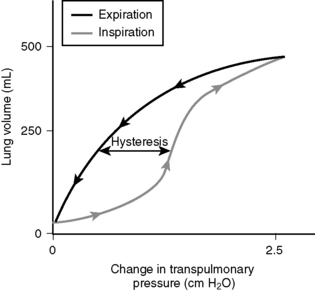
Figure 2-2 shows a compliance curve of the lungs. Note that the lungs are most compliant in the midportion of the inspiratory curve (steepest slope). Breathing at an elevated functional residual capacity (as patients with chronic obstructive pulmonary disease [COPD] are prone to do for a variety of reasons) is less efficient and requires more work.
5 What does pulmonary elastance measure? How is pulmonary elastance altered in restrictive and obstructive lung diseases and why?
6 How does surfactant affect alveolar surface tension?
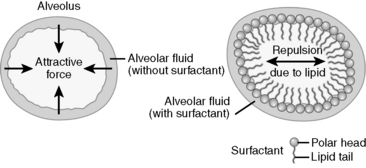
Water molecules lining the surface of alveoli are attracted to each other and are repelled by the hydrophobic air molecules. The attractive force between water molecules generates surface tension, which in turn produces a collapsing pressure that promotes alveolar collapse. Surfactant is composed of phospholipids (mainly lecithin and sphingomyelin) that reduce the collapsing pressure by minimizing the interaction between alveolar fluid and alveolar air (Fig. 2-3).
7 Why are smaller alveoli more prone to collapse, and how is this relevant to neonatal respiratory distress syndrome?
9 What is “dead space”? What is the difference between anatomic dead space and physiologic dead space?
Basic concepts—ventilation-perfusion matching
11 What does the ventilation/perfusion ratio measure, and what is its approximate value? What is an “ideal” value for this ratio?
14 What effect does chronic obstructive pulmonary disease usually have on the ventilation-perfusion ratio?
Basic concepts—gas exchange
16 What influences the diffusion of gases from the alveoli into the pulmonary capillaries, and vice versa?
where Vgas is the volume of gas that traverses the membrane per unit time, A is the surface area of the membrane, D is the diffusivity of the particular gas in the particular membrane, P1 − P2 is the partial pressure difference of the specific gas across the membrane, and T is the thickness of the membrane.
17 What is the alveolar-arterial oxygen gradient and what is the clinical significance of its magnitude?
18 How is the alveolar-arterial oxygen gradient calculated?
where
where FIO2 = the fraction of inspired oxygen (usually 0.21), PB is barometric pressure (usually 760 mm Hg), PH2O is water vapor pressure (usually 47 mm Hg), PACO2 = alveolar pressure of carbon dioxide, which equals the arterial pressure of carbon dioxide due to rapid diffusion across the alveolar membrane, and R = the respiratory quotient (usually 0.8).
20 How does increasing or decreasing the arterial PCO2 affect pH?
When CO2 dissolves in water, the following reaction occurs:
where CA is carbonic anhydrase.
23 What is the principal difference between “restrictive” and “obstructive” lung disease with respect to the FEV1/FVC ratio?
Table 2-1 lists some examples of obstructive and restrictive lung diseases.
Table 2-1 Obstructive and Restrictive Lung Diseases
| Obstructive Lung Diseases | Restrictive Lung Diseases |
|---|---|
| Chronic bronchitis Emphysema Asthma Bronchiectasis Cystic fibrosis | Neuromuscular diseases (poliomyelitis, myasthenia gravis, Duchenne muscular dystrophy, Guillain-Barré syndrome) Acute respiratory distress syndrome (ARDS) Neonatal respiratory distress syndrome Sarcoidosis Idiopathic pulmonary fibrosis Goodpasture’s syndrome Wegener’s granulomatosis Drug toxicity Pleural diseases |
4 About 5% of asthmatics are sensitive to aspirin, and some may even develop fatal bronchospasm from ingesting aspirin. What is currently believed to be the biochemical basis of this?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree