Chapter 1 Cardiology
Basic concepts—hemodynamics
3 What are the three main factors that affect stroke volume?
The determinants of SV are preload, contractility, and afterload.
4 What is preload, and how does it affect stroke volume?
In addition, a variety of positions or maneuvers can be tried to manipulate venous return (preload) to the heart. For example, both the Valsalva maneuver (expiration against a closed glottis) and standing will decrease preload, and both squatting and passive leg raising will increase preload. Having the patient perform these actions can be useful when distinguishing various murmurs from one another (Fig. 1-1).
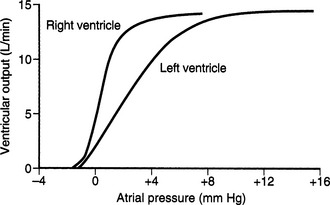
Figure 1-1 Increased ventricular output as a function of end-diastolic volume (reflected by atrial pressure).
(From Guyton AC, Hall JE: Textbook of Medical Physiology, 11th ed. Philadelphia, WB Saunders, 2006, p 112.)
8 What is the mechanism by which the sympathetic nervous system responds to a reduction in blood pressure?
When blood pressure drops, arterial baroreceptors located within the carotid sinus (afferent limb mediated by the glossopharyngeal nerve) sense decreased vessel stretch and fire less frequently. This response increases efferent sympathetic outflow and inhibits parasympathetic outflow, which helps restore the blood pressure by increasing heart rate and stimulating peripheral vasoconstriction. Conversely, if the blood pressure increases, baroreceptors in the carotid sinus or aortic arch (afferent limb mediated by the vagus nerve; responds only to increases in blood pressure) fire more frequently because they are being “stretched” more, which causes greater inhibition of the sympathetic outflow (Fig. 1-2).
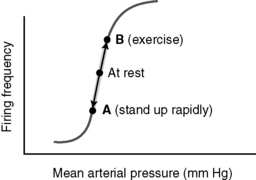
Figure 1-2 Control of blood pressure by the baroreceptor reflex.
(From Brown TA: Rapid Review Physiology. Philadelphia, Mosby, 2007, p 144.)
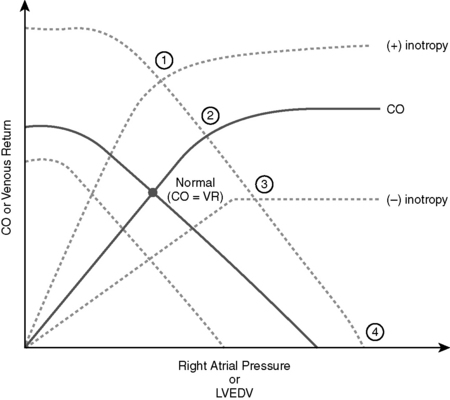
12 Which clinical scenarios would shift the CO and venous return curves to the points labeled 1 to 4 on Figure 1-3?
1. Exercise: Lower limb muscles push blood toward the right atrium and increase venous return. Sympathetic activity increases CO by increasing HR, SV, and contractility.
2. Arteriovenous fistulas: Increased venous return from an arteriovenous fistula will shift the venous return curve to the right. CO does increase but only because of the increased preload (Frank-Starling mechanism); this increase is therefore not due to a change in contractility (inotropy). If these arteriovenous anastomoses were much larger, the operating point of the heart would be shifted to (1) because it would cause a large decrease in SVR and stimulate the activity of the sympathetic nervous system, increasing inotropy; these large anastomoses are sometimes referred to as AV shunts.
3. Compensated heart failure: Patients with this condition have elevated right atrial pressures due to an increased volume status caused by the activity of the renin-angiotensin-aldosterone system (RAAS). Their cardiac function is decreased (decreased inotropy), but they can maintain a normal CO at rest with the increased volume (Frank-Starling mechanism).
4. Ventricular fibrillation: Ventricular fibrillation causes equalization of all pressures. Right atrial pressure increases to become equal to the mean systolic filling pressure. CO in ventricular fibrillation simply becomes equal to zero.
Basic concepts—excitation-contraction coupling
Basic concepts—arrhythmias
1 What is the relationship between the various phases of the ventricular myocyte action potential and the different ion fluxes across the cell membrane?
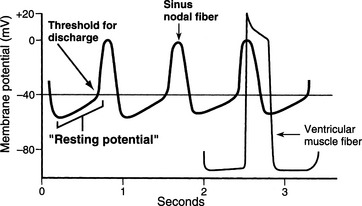
In phase 0 of the action potential, the sharp rise in membrane voltage is due to sodium influx. Phase 1 involves a brief repolarization that is due to the transient outward flow of potassium that follows sodium channel inactivation. In phase 2, the action potential plateaus are due to a balance between calcium influx and potassium efflux. During phase 3, there is rapid repolarization due to unopposed potassium efflux. Phase 4 is the resting potential, which is maintained predominantly through the opening of potassium channels. Intracellular concentrations of K+ are maintained at high levels in cardiac myocytes because of the action of membrane-bound Na+K+-ATPase. Opening of potassium channels during phase 4 leads to potassium efflux (down its concentration gradient). Since the cell is permeable only to potassium at this time, negatively charged counter ions for K+ are unable to diffuse outward with potassium. As potassium leaves the cell, anions left behind cause the cell to become increasingly negative in charge. Therefore the effluxed potassium ions are attracted back toward the interior of the cell to maintain resting potential. Because phase 4 is dominated by potassium permeability, it therefore has a value close to the potassium reversal potential (−85 mV) (Fig. 1-4).
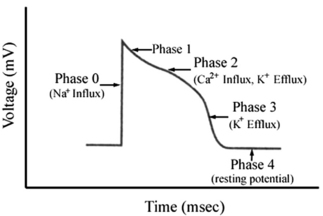
Figure 1-4 Phases of the ventricular myocyte action potential.
(From Brown TA, Brown D: USMLE Step 1 Secrets. Philadelphia, Hanley & Belfus, 2004, p 77.)
2 What is responsible for the drifting of the resting membrane potential in nodal cells?
These cells are more permeable to sodium, so sodium influx during the “resting” membrane potential causes the membrane to gradually depolarize. Because nodal cells lack the fast voltage-gated sodium channels (INa) found in the rest of the myocardium, this is accomplished by the If sodium current, a unique “leaky” sodium channel that promotes the gradual depolarization of these cells through sodium influx. Eventually, when the membrane depolarizes to its “threshold,”; this state will activate slow calcium channels that engender an action potential (Fig. 1-5).
3 Through what mechanism does sympathetic stimulation increase heart rate?
Note: The beta blockers are considered class II antiarrhythmics.
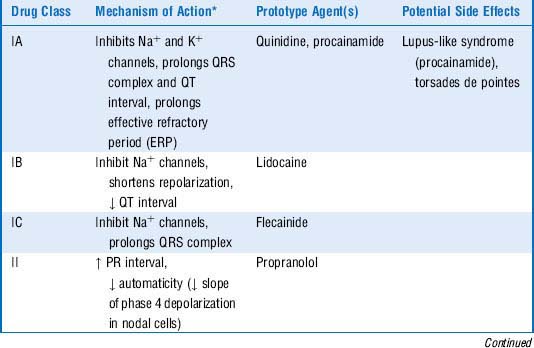
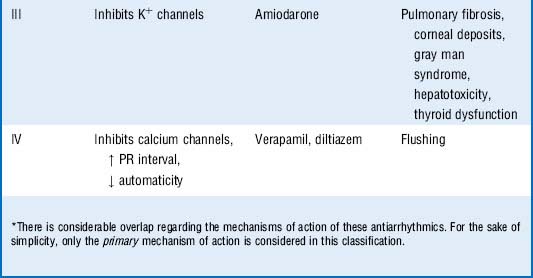
4 What are the classes of antiarrhythmics and how do their mechanisms of action and potential side effects vary?
See Table 1-1 for this information.
2 How is hypertension defined and what are the potential complications?
The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure guidelines (JNC 7) for defining hypertension are presented in Table 1-2.
Table 1-2 Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure Guidelines for Defining Hypertension
| Category | Blood Pressure Range (mm Hg) | |
|---|---|---|
| Systolic | Diastolic | |
| Normal | < 120 | <80 |
| Prehypertension | 120-139 | 80-89 |
| Hypertension: stage 1 | 140-159 | 90-99 |
| Hypertension: stage 2 | ≥160 | ≥100 |
3 What are four classes of drugs that could be useful in treating this man’s hypertension?
 Diuretics (e.g., thiazides, loop, potassium-sparing)
Diuretics (e.g., thiazides, loop, potassium-sparing)
 Inhibitors of the renin-angiotensin-aldosterone system (e.g., angiotensin-converting enzyme [ACE] inhibitors, angiotensin receptor blockers)
Inhibitors of the renin-angiotensin-aldosterone system (e.g., angiotensin-converting enzyme [ACE] inhibitors, angiotensin receptor blockers)
 Vasodilators (e.g., direct-acting, calcium channel blockers)
Vasodilators (e.g., direct-acting, calcium channel blockers)
6 Caution should be used in prescribing beta blockers for patients with which comorbid conditions and why?
 Asthma: Risk of worsening bronchospasm by preventing β2-mediated bronchodilation. (Even β1– “selective” antagonists have some effect, especially at high doses.) For the purpose of the USMLE, remember that β1-selective blockers should be used in patients with pulmonary disease.
Asthma: Risk of worsening bronchospasm by preventing β2-mediated bronchodilation. (Even β1– “selective” antagonists have some effect, especially at high doses.) For the purpose of the USMLE, remember that β1-selective blockers should be used in patients with pulmonary disease.
 COPD (chronic obstructive pulmonary disease) patients for similar reasons.
COPD (chronic obstructive pulmonary disease) patients for similar reasons.
 Peripheral arterial disease: Exacerbation of claudication. (Vasodilation in skeletal muscle arterioles is mediated by β2-adrenergic receptors present on vascular smooth muscle cells.)
Peripheral arterial disease: Exacerbation of claudication. (Vasodilation in skeletal muscle arterioles is mediated by β2-adrenergic receptors present on vascular smooth muscle cells.)
 First-degree atrioventricular (AV) block: Beta blockers decrease AV conduction and thus further lengthen the already prolonged PR interval on the electrocardiogram (ECG). This can result in excessive cardiac depression. (Beta blockers should not be given at all to patients with second- or third-degree AV block because they could delay AV conduction even further. Certain calcium channel blockers, such as verapamil and diltiazem, might also reduce AV conduction and, when used in combination with beta blockers, can produce a serious AV block.)
First-degree atrioventricular (AV) block: Beta blockers decrease AV conduction and thus further lengthen the already prolonged PR interval on the electrocardiogram (ECG). This can result in excessive cardiac depression. (Beta blockers should not be given at all to patients with second- or third-degree AV block because they could delay AV conduction even further. Certain calcium channel blockers, such as verapamil and diltiazem, might also reduce AV conduction and, when used in combination with beta blockers, can produce a serious AV block.)
 Diabetes: Beta blockers reduce the normal symptoms of hypoglycemia (e.g., headache, confusion, slurred speech, anxiety, tremors, palpitations) that provide warning to diabetic patients prior to reaching dangerously low blood sugar levels.
Diabetes: Beta blockers reduce the normal symptoms of hypoglycemia (e.g., headache, confusion, slurred speech, anxiety, tremors, palpitations) that provide warning to diabetic patients prior to reaching dangerously low blood sugar levels.
 Because of their ability to reduce myocardial oxygen demand, beta blocker use has been shown to have a survival benefit in patients with congestive heart failure. However, caution should be used when placing patients on beta blockers, as they may initially exacerbate CHF symptoms (decompensated heart failure).
Because of their ability to reduce myocardial oxygen demand, beta blocker use has been shown to have a survival benefit in patients with congestive heart failure. However, caution should be used when placing patients on beta blockers, as they may initially exacerbate CHF symptoms (decompensated heart failure).
 Erectile dysfunction: beta blockers may inhibit b2 adrenergic receptor-mediated vasodilation.
Erectile dysfunction: beta blockers may inhibit b2 adrenergic receptor-mediated vasodilation.
 Depression: Mechanism of action is unclear, but presumably involves alterations in monoamine neurotransmitter signaling.
Depression: Mechanism of action is unclear, but presumably involves alterations in monoamine neurotransmitter signaling.
7 What might be occurring in this patient and how would you recommend he discontinue his medication?
 Essential hypertension is the most common type of hypertension.
Essential hypertension is the most common type of hypertension.
 The most common causes of secondary hypertension are renal artery stenosis and primary hyperaldosteronism.
The most common causes of secondary hypertension are renal artery stenosis and primary hyperaldosteronism.
 Beta blockers lower blood pressure in part by reducing renin secretion from the kidneys (primarily a β1-receptor–mediated effect).
Beta blockers lower blood pressure in part by reducing renin secretion from the kidneys (primarily a β1-receptor–mediated effect).
 Beta blockers decrease atrioventricular (AV) conduction and therefore should be used cautiously in patients with first-degree heart block.
Beta blockers decrease atrioventricular (AV) conduction and therefore should be used cautiously in patients with first-degree heart block.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree