Public Health Surveillance and Outbreak Investigation
Objectives
After reading this chapter, the student should be able to do the following:
1. Define public health surveillance.
2. Analyze types of surveillance systems.
3. Identify steps in planning, analyzing, interviewing, and evaluating surveillance.
4. Recognize sources of data used when investigating a disease/condition outbreak.
Key Terms
algorithms, p. 535
biological terrorism, p. 534
BioNet, p. 540
case definition, p. 536
chemical terrorism, p. 534
clusters of illness, p. 533
common source, p. 541
disease surveillance, p. 533
endemic, p. 541
Enhanced Surveillance Project (ESP), p. 540
epidemic, p. 541
event, p. 534
holoendemic, p. 541
hyperendemic, p. 541
infectivity, p. 541
intermittent or continuous source, p. 541
Laboratory Response Network (LRN), p. 540
mixed outbreak, p. 541
National Notifiable Disease Surveillance System (NNDSS), p. 539
outbreak, p. 541
outbreak detection, p. 541
outcome data, p. 534
pandemic, p. 541
pathogenicity, p. 541
point source, p. 541
process data, p. 534
propagated outbreak, p. 541
public health protection, p. 533
PulseNet, p. 540
sentinel, p. 536
sporadic, p. 541
syndronic surveillance systems, p. 540
virulence, p. 541
—See Glossary for definitions
 Marcia Stanhope, RN, DSN, FAAN
Marcia Stanhope, RN, DSN, FAAN
Dr. Marcia Stanhope, as Chair and board member of the local board of health, has been involved in developing policy, processes, and responses for community surveillance and outbreak investigations in her local community. She is also involved in the development of a course on this topic for the doctorate of nursing practice program at the University of Kentucky. The Lexington community, through the health department incident command center, responded to the Hurricane Katrina disaster by establishing shelters for New Orleans residents who had to leave their homes and who came to Kentucky. Dr. Stanhope had an opportunity to participate with the American Red Cross and Dr. Susan Hassmiller (author of Chapter 23) in the past to consider nursing education curricular ideas related to the topic.
Disease surveillance has been a part of public health protection since the 1200s during the investigations of the bubonic plague in Europe. During the 1600s John Grant developed the fundamental principles of public health including surveillance and outbreak investigation, and in the 1700s Rhode Island passed the first public health laws to provide for the protection of health and care of the population of the state. In the eighteenth century, Farr introduced the modern version of surveillance and, along with the United States, Italy, and Great Britain, began required reporting systems for infectious diseases. By 1925 the United States began national reporting of morbidity causes. By 1935 the first national health survey had been conducted, and in 1949 the National Office of Vital Statistics published weekly mortality and morbidity statistics in the Journal of Public Health Reports. This activity was later transferred to the Centers for Disease Control and Prevention, who began publishing the Morbidity and Mortality Weekly Report in 1961. Laws, regulations, reporting mechanisms, and data collections are all essential to surveillance and disease outbreak investigations.
The Constitution of the United States provides for “police powers” necessary to preserve health safety as well as other events (see Chapter 8). These powers include public health surveillance. State and local “police powers” also provide for surveillance activities. Health departments usually have legal authority to investigate unusual clusters of illness as well (CDC, 2009a).
Disease Surveillance
Definitions and Importance
Disease surveillance is the ongoing systematic collection, analysis, interpretation and dissemination of specific health data for use in public health (Lee et al, 2010; Webster’s, 2008). Surveillance provides a means for nurses to monitor disease trends in order to reduce morbidity and mortality and to improve health (Veenema and Toke, 2006).
Surveillance is a critical role function for nurses practicing in the community. A comprehensive understanding and knowledge of the surveillance systems and how they work will help nurses improve the quality and the usefulness of the data collected for making decisions about needed community services, community actions, and public health programming (Box 24-1).
Surveillance is important because it generates knowledge of a disease or event outbreak patterns (including timing, geographic distribution, and susceptible populations). The knowledge can be used to intervene to reduce risk or prevent an occurrence at the most appropriate points in time and in the most effective ways. Surveillance is built on understanding of epidemiological principles of agent, host, and environmental relationships and on the natural history of disease or conditions (see Chapter 12). Surveillance systems make it possible to engage in effective continuous quality improvement activities within organizations and to improve quality of care (Veenema, 2007).
Surveillance focuses on the collection of process and outcome data. Process data focus on what is done (i.e., services provided or protocols for health care delivery). Outcome data focus on changes in health status. The activities generated by analyses of these data aim to improve public health response systems. An example of process data is collection of data about the proportion of the eligible population vaccinated against influenza in any one year. Outcome data in this case are the incidence rates (new cases) of influenza among the same population in the same year.
Although surveillance was initially devoted to monitoring and reducing the spread of infectious diseases, it is now used to monitor and reduce chronic diseases and injuries, and environmental and occupational exposures (Veenema and Toke, 2007) as well as personal health behaviors. Surveillance systems help nurses and other professionals monitor emerging infections and bioterrorist outbreaks (Pryor and Veenema, 2007). Bioterrorism is one example of an event creating a critical public health concern that involves environmental exposures that must be monitored. This event also requires serious planning in order to be able to respond quickly and effectively. Biological terrorism is defined as “the deliberate release of viruses, bacteria, or other germs (agents) used to cause illness or death in people, animals, or plants” (http://www.bt.cdc.gov/bioterrorism) (CDC, 2007). Chemical terrorism is the intentional release of hazardous chemicals into the environment for the purpose of harming or killing (CDC, 2006). In the event of a bioterrorist attack, imagine how difficult it would be to control the spread of biological agents such as botulism or anthrax or chemical agents such as sarin or ricin if no data were available about these agents, their resulting diseases or symptoms, and their usual incidence (new cases) patterns (new cases) in the community. (See Box 24-1 for a summary of the features of surveillance.)
Uses of Public Health Surveillance
Public health surveillance can be used to facilitate the following (CDC, 2010c):
• Estimate the magnitude of a problem (disease or event)
• Determine geographic distribution of an illness or symptoms
• Portray the natural history of a disease
• Detect epidemics; define a problem
• Generate hypotheses; stimulate research
• Monitor changes in infectious agents
• Detect changes in health practices
Purposes of Surveillance
Surveillance helps public health departments identify trends and unusual disease patterns, set priorities for using scarce resources, and develop and evaluate programs for commonly occurring and universally occurring diseases or events (Box 24-2).
Surveillance activities can be related to the core functions of public health: assessment, policy development, and assurance. Disease surveillance helps establish baseline (endemic) rates of disease occurrence and patterns of spread. Surveillance makes it possible to initiate a rapid response to an outbreak of a disease or event that can cause a health problem. For example, surveillance made it possible to respond quickly to the anthrax outbreak that occurred shortly after the September 11th attack on the World Trade Centers. Surveillance also made it possible to respond early to the H1N1 outbreak that initially began in Mexico in 2009 (CDC, 2010a).
Surveillance data are analyzed, and interpretations of these data analyses are used to develop policies that better protect the public from problems such as emerging infections, bioterrorist biological and chemical threats, and injuries from problems such as motor vehicle accidents. In 2006 a lot of emphasis was placed on developing disaster management policies in health care organizations, industries, and homes so the U.S. population could be prepared in the event of an emergency. Surveillance within individual organizations, such as infection control systems in hospitals, can be used to establish policies related to clinical practice that are designed to improve quality of care processes and outcomes. An example is documented by Ergaz et al (2010), where a policy of weekly fecal cultures for vancomycin-resistant enterococci (VRE) was instituted following the investigation of an outbreak of VRE in the neonatal intensive care unit.
Surveillance makes it possible to have ongoing monitoring in place to ensure that disease and event patterns improve rather than deteriorate. They can also make it possible to study whether the clinical protocols and public health policies that are in place can be enhanced based on current science so disease rates actually decline. For example, the ongoing monitoring of obesity in children in a community may show that new clinical and effective protocols need to be developed to be used in school-based clinics to reduce the prevalence of obesity among the school populations.
Surveillance data are very helpful in determining whether a program is effective. Such data make it possible to determine whether public health interventions are effective in reducing the spread of disease or the incidence of injuries. By determining the change in the number of cases at the beginning of a program (baseline) with the number of cases following program implementation, it is possible to estimate the effectiveness of a program. One could then compare the effectiveness of different approaches to reducing the problem or to improving health. Johns et al (2010) investigated whether prior seasonal influenza vaccination was effective against the pandemic strain of H1N1 (pH1N1) virus among military personnel. Their findings indicated that with the seasonal influenza vaccines of 2004 to 2009, moderate protection against H1N1 was associated with the vaccines of these years. The protection seemed to have a greater association with severe disease rather then a mild case regardless of age of the ill person.
Collaboration Among Partners
A quality surveillance system requires collaboration among a number of agencies and individuals: federal agencies, state and local public health agencies, hospitals, health care providers, medical examiners, veterinarians, agriculture, pharmaceutical agencies, emergency management, and law enforcement agencies, as well as 911 systems, ambulance services, urgent care and emergency departments, poison control centers, nurse hotlines, schools, and industry. Such collaboration promotes the development of a comprehensive plan and a directory of emergency responses and contacts for effective communication and information sharing. The type of information to be shared includes the following:
Nurses are often in the forefront of responses to be made in the surveillance process whether working in a small rural agency or a large urban agency; within the health department, school, or urgent care center; or on the telephone performing triage services during a disaster. It is the nurse who sees the event first (ASTDN, 2007).
Nurse Competencies
The national core competencies for public health nurses were developed from the work of the Council on Linkages Between Academia and Public Health Practice (Core Competencies for Public Health Professionals, 2010) and by the Quad Council of Public Health Nursing Organizations (2009). These competencies are divided into eight practice domains: analytical assessment skills, policy/program development, communication, cultural competency, community dimensions of practice, basic public health sciences, financial planning/management, and leadership.
To be a participant in surveillance and investigation activities, the staff nurse must have the following knowledge related to the core competencies:
1. Analytical assessment skills
• Identifying relevant data and information sources
• Partnering with others to give meaning to the data collected
• Providing effective oral and written reports
3. Community dimensions of practice
• Establishing and maintaining links during the investigation
• Developing, implementing, and evaluating an assessment to define the problem
4. Basic public health science skills
• Identifying individual and organizational responsibilities
• Identifying and retrieving current relevant scientific evidence
5. Leadership and systems thinking
• Identifying internal and external issues that have an effect on the investigation
• Promoting team and organizational efforts
• Contributing to developing, implementing, and monitoring of the investigation
While the staff nurse participates in these activities, the nurse clinical specialist should be proficient in applying these competencies. In addition, the nurse applies the nursing process in preparedness as illustrated in Table 24-1.
TABLE 24-1
PHASES OF NURSING PROCESS LINKED TO PREPAREDNESS
| DEFINITION OF PREPAREDNESS | ASSESSMENT | PLANNING | IMPLEMENTATION | EVALUATION |
| Assure capacity to respond effectively to disasters and emergencies | Assess the populations at risk for special needs during a disaster | Develop plans to care for special needs populations during a disaster | Conduct training, drills, and exercises related to care of special needs persons | Evaluate plans for serving populations with special needs |
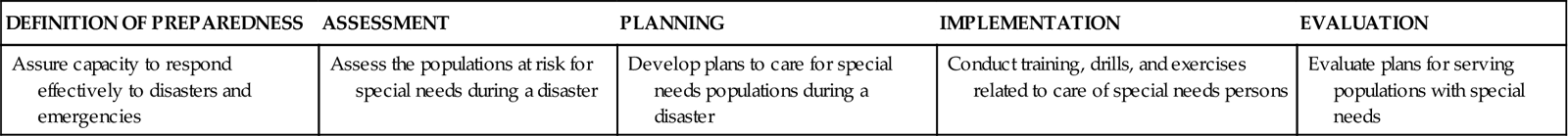
Excerpted from ASTDN: The role of public health nurses in emergency preparedness and response, 2007, The Association, Table 1, Phases of Disaster Linked to the Nursing Process.
The Minnesota Model of Public Health Interventions: Applications for Public Health Nursing Practice (2001, pp 15-16) suggests that surveillance is one of the interventions related to public health nursing practice. The model gives seven basic steps of surveillance for nurses to follow:
1. Consider whether surveillance as an intervention is appropriate for the situation.
2. Organize the knowledge of the problem, its natural course of history, and its aftermath.
3. Establish clear criteria for what constitutes a case.
4. Collect sufficient data from multiple valid sources.
6. Interpret data and disseminate to decision makers.
Data Sources for Surveillance
Clinicians, health care agencies, and laboratories report cases to state health departments. Data also come from death certificates and administrative data such as discharge reports and billing records (Pryor and Veenema, 2007). The following are select sources of mortality and morbidity data:
1. Mortality data are often the only source of health-related data available for small geographic areas. Examples include the following:
• Vital statistics reports (e.g., death certificates, medical examiner reports, birth certificates)
2. Morbidity data include the following:
• Specialized disease registries
A good example of a process in place to collect morbidity data is the National Program of Cancer Registries. This program provides for monitoring of the types of cancers found in a state and the locations of the cancer risks and health problems in the state.
Each of the data sources has the potential for underreporting or incomplete reporting. However, if there is consistency in the use of surveillance methods, the data collected will show trends in events or disease patterns that may indicate a change needed in a program or a needed prevention intervention to reduce morbidity or mortality. Underreporting or incomplete reporting may occur for the following reasons: social stigma attached to a disease (such as HIV/AIDS); ignorance of required reporting system; lack of knowledge about the case definition, procedural changes in reporting, or changes in a database; limited diagnostic abilities; or low priority given to reporting (CDC, 2010a).
Mortality data assist in identifying differences in health status among groups, populations, occupations, and communities; monitor preventable deaths; and help to examine cause-and-effect factors in diseases. Vital statistics can be used to plan programs and to monitor programs to meet Healthy People 2020 goals.
The notifiable disease laboratory as well as hospital discharge and billing data provide mechanisms for classifying diseases and events and calculating rates of diseases within and across groups, populations, and communities.
The sentinel surveillance system provides for the monitoring of key health events when information is not otherwise available or in vulnerable populations to calculate or estimate disease morbidity. Registrations monitor chronic disease in a systematic manner, linking information from a variety of sources (health department, clinics, hospitals) to identify disease control and prevention strategies. Surveys then provide data from individuals about prevalence of health conditions and health risks. Such surveys allow for monitoring changes over time and assessing the individual’s knowledge, attitudes, and beliefs. This information can be used for health education and other planned interventions (CDC, 2009a).
Notifiable Diseases
Before 1990 state and local health departments used many different criteria for identifying cases of reportable diseases. Using different criteria made the data less useful than it could have been because it could not be compared across health departments or states. For this reason some diseases may have been underreported and others may have been overreported. In 1990 the CDC and the Council of State and Territorial Epidemiologists assembled the first list of standard case definitions. This list was revised in 1997, and more information may be found at the CDC Division of Public Health Surveillance and Informatics website (CDC, 1997). This site contains information about the National Notifiable Disease Surveillance System (CDC-NNDSS, 2010d), and the definitions remain the same today.
National Notifiable Diseases
Box 24-3 shows the national notifiable infectious diseases. Reporting of disease data by health care providers, laboratories, and public health workers to state and local health departments is essential if trends are to be accurately monitored. “The data provide the basis for detecting disease outbreaks, for identifying person characteristics, and for calculating incidence, geographic distribution, and temporal trends. They are used to initiate prevention programs, evaluate established prevention and control practices, suggest new intervention strategies, identify areas for research, document the need for disease control funds, and help answer questions from the community” (http://www.ced.gov/epo/dphsi/phs/infdis2010.htm) (CDC, 2010e). The CDC and the Council of State and Territorial Epidemiologists have a policy that requires state health departments to report selected diseases to the CDC’s NNDSS. The data for nationally notifiable diseases from 50 states, the U.S. territories, New York City, and the District of Columbia are published weekly in the Morbidity and Mortality Weekly Report (MMWR). Data collection about these diseases is ongoing and revision of statistics is ongoing. Annual updated final reports are published in the CDC Summary of Notifiable Diseases—United States (CDC, 2010d).



