Communicable and Infectious Disease Risks
Objectives
After reading this chapter, the student should be able to do the following:
2. Explain the clinical signs of selected communicable diseases.
4. Analyze behaviors that place people at risk of contracting selected communicable diseases.
5. Evaluate nursing activities to prevent and control selected communicable diseases.
6. Explain the various roles of nurses in providing care for those with selected communicable diseases.
Key Terms
acquired immunodeficiency syndrome, p. 318
chlamydia, p. 324
directly observed therapy, p. 334
genital herpes, p. 325
genital warts, p. 325
gonorrhea, p. 321
hepatitis A virus (HAV), p. 326
hepatitis B virus (HBV), p. 327
hepatitis C virus (HCV), p. 328
highly active antiretroviral therapy (HAART), p. 318
HIV antibody test, p. 318
HIV infection, p. 318
human immunodeficiency virus, p. 317
human papillomavirus, p. 325
incidence, p. 321
incubation, p. 318
injection drug use, p. 319
non-gonococcal urethritis, p. 325
partner notification, p. 329
pelvic inflammatory disease, p. 324
perinatal HIV transmission, p. 319
prevalence, p. 319
sexually transmitted diseases, p. 317
syphilis, p. 324
tuberculosis, p. 328
 Patty J. Hale, RN, FNP, PhD, FAAN
Patty J. Hale, RN, FNP, PhD, FAAN
Dr. Patty Hale is Professor and Graduate Program Director at James Madison University in Harrisonburg, Virginia. She has practiced public health nursing in Wisconsin and Virginia and has consulted widely with many organizations on community health and infectious diseases, most notably the World Health Organization. Dr. Hale has taught undergraduate and graduate courses in epidemiology, curriculum development and evaluation, community health, and population-focused nursing. An advocate for HIV/AIDS education and prevention, Dr. Hale developed and taught two of the first courses ever on HIV/AIDS early in the epidemic. She formerly taught at the University of Virginia in Charlottesville, Virginia and at Lynchburg College. As a family nurse practitioner, she has practiced in community health centers and, along with students, conducted clinical research. Her publications and presentations have been in the areas of HIV/AIDS, health promotion, service learning, and nursing education. She received a 2005 American Journal of Nursing Book of the Year Award for the CD, Real World Community Health Nursing. Dr. Hale was named a Carnegie U.S. Professor of the Year in 2003, and was the first nurse ever to receive this honor. Dr. Hale holds a bachelor of science from the University of Wisconsin-Milwaukee. She has a master’s in community health nursing and family nurse practitioner from the University of Virginia, and a doctorate in nursing from the University of Maryland at Baltimore.
Knowledge about the risk of communicable diseases has changed dramatically in recent years. For example, in the decades following the development of antibiotics in the 1940s, sexually transmitted diseases (STDs) were considered to be a problem of the past. The recent emergence of new viral STDs and antibiotic-resistant strains of bacterial STDs has posed new challenges. Left unchecked, STDs can cause poor pregnancy outcomes, infertility, and cervical cancers. There is also the problem of co-infection, with one STD increasing the susceptibility to other STDs, such as human immunodeficiency virus (HIV).
This concern about infectious diseases has prompted the development of standards for STDs, HIV and acquired immunodeficiency syndrome (AIDS), hepatitis, and tuberculosis (TB) in the Healthy People 2020 report. The Healthy People 2020 box shows some objectives used to evaluate progress toward decreasing communicable diseases by the year 2020.
Several communicable diseases and all STDs are acquired through behaviors that can be avoided or changed, and thus intervention efforts by nurses have focused on disease prevention. Prevention can take the form of vaccine administration (as with hepatitis A and hepatitis B), early detection (of TB, for example), or instruction of clients about abstinence or safer sex. Individuals who live with chronic infections can transmit them to others.
This chapter describes selected communicable diseases and their nursing management. It concludes with implications for nursing care in primary, secondary, and tertiary prevention.
Human Immunodeficiency Virus Infection
Human immunodeficiency virus (HIV) infection and AIDS have had an enormous political and social impact on society. Controversies have arisen over many aspects of HIV. Fears about HIV may lead to attitudes of blaming clients for their infections and to discrimination. These beliefs are magnified by the fact that this disease has commonly afflicted two groups who have been largely scorned by society: homosexuals and injection drug users (Fair and Ginsberg, 2010). Debates have arisen over how to control disease transmission and how to pay for related health services. An ongoing debate involves whether clean needles should be distributed to injection drug users to prevent the spread of HIV.
Economic costs of HIV/AIDS result from premature disability and treatment. The fact that nearly 75% of new HIV infections occur in persons between the ages of 30 and 49 years may result in disrupted families and lost creative and economic productivity at a period of life when vitality is the norm (CDC, 2009a). The health care delivery costs of those infected are supported primarily by Medicaid and Medicare. Many people with HIV qualify for Medicaid or Medicare because they are indigent or fall into poverty when paying for health care over the course of the illness. Lifetime cost of HIV care for one client is $618,900 (Schackman et al, 2006). The Ryan White Comprehensive AIDS Resource Emergency (CARE) Act provides services for persons with HIV infection (HRSA, 2008). This program provides funds for health care in the geographic areas with the largest number of AIDS cases. Health services that are covered include emergency services, services for early intervention and care (sometimes including coverage of health insurance), and drug reimbursement programs for HIV-infected individuals. The AIDS Drug Assistance Programs (ADAPs) are awards that pay for medications on the basis of the estimated number of persons living with AIDS in the individual state (USDHHS, 2010).
Natural History of HIV
The natural history of HIV includes three stages: the primary infection (within about 1 month of contracting the virus), followed by a period when the body shows no symptoms (clinical
latency), and then a final stage of symptomatic disease (Buttaro et al, 2008).
When HIV enters the body, a person may experience a mononucleosis-like syndrome, referred to as a primary infection, which lasts for a few weeks. This may go unrecognized. The body’s CD4 white blood cell count drops for a brief time when the virus is most plentiful in the body. The immune system increases antibody production in response to this initial infection, which is a self-limiting illness. Symptoms include lymphadenopathy, myalgias, sore throat, lethargy, rash, and fever (CDC, 2010e). Even if the client seeks medical care at this time, the antibody test at this stage is usually negative, so it is often not recognized as HIV.
After a variable period of time, commonly from 6 weeks to 3 months, HIV antibodies appear in the blood. Although most antibodies serve a protective role, HIV antibodies do not. However, their presence helps in the detection of HIV infection because screening tests show their presence in the bloodstream.
HIV-infected persons live several years before developing symptomatic disease. During this prolonged incubation period, clients have a gradual deterioration of the immune system and can transmit the virus to others. The use of highly active antiretroviral therapy (HAART) has greatly increased the survival time of persons with HIV/AIDS.
Acquired immunodeficiency syndrome (AIDS) is the last stage in the long continuum of HIV infection and may result from damage caused by HIV, secondary cancers, or opportunistic organisms. AIDS is defined as a disabling or life-threatening illness caused by HIV; it is diagnosed in a person with a CD4 T-lymphocyte count of less than 200/mL with documented HIV infection (CDC, 2008).
Many of the AIDS-related opportunistic infections are caused by microorganisms that are commonly present in healthy individuals but do not cause disease in persons with an intact immune system. These microorganisms proliferate in persons with HIV/AIDS because of a weakened immune system. Opportunistic infections may be caused by bacteria, fungi, viruses, or protozoa. The most common opportunistic diseases are Pneumocystis jiroveci (carinii) pneumonia and oral candidiasis, but also include pulmonary TB, invasive cervical cancer, or recurrent pneumonia.
In 2008 the case definition for HIV infection was revised to include the HIV classification system based on the number of CD4+ T-lymphocytes. Criteria for defining HIV infection include a positive result from the antibody screening test or a positive result from a nucleic acid test (DNA or RNA). In situations where the mother of a newborn is HIV infected, the HIV nucleic acid test (DNA or RNA) is used to identify HIV/AIDS in infants (CDC, 2008).
TB, an infection that is becoming more prevalent because of HIV infection, can spread rapidly among immunosuppressed individuals. Thus, HIV-infected individuals who live in close proximity to one another, such as in long-term care facilities, prisons, drug treatment facilities, or other settings, must be carefully screened and in some instances deemed non-infectious before admission to such settings. TB is covered in more depth later in this chapter.
Transmission
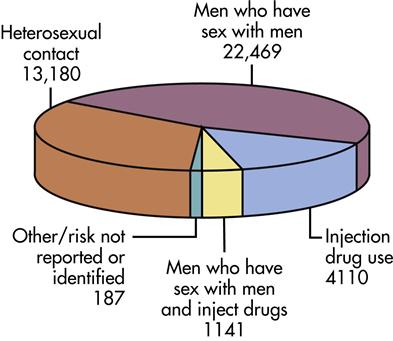
HIV is transmitted through exposure to blood, semen, transplanted organs, vaginal secretions, and breast milk (Heymann, 2008). Persons who had blood exposure or sexual or needle-sharing contact with an HIV-infected person are at risk for contracting the virus. The virus is not transmitted through casual contact such as touching or hugging someone who has HIV infection or through mosquitoes or other insects. Although HIV has been found in saliva and tears in some instances, it has not been reported to be transmitted through contact with these body fluids (Heymann, 2008). The modes of transmission are listed in Box 14-1, and the exposure categories of AIDS are shown in Figure 14-1.
Potential donors of blood and tissues are screened through interviews to assess for a history of high-risk activities and screened with the HIV antibody test. Blood or tissue is not used from individuals with a history of high-risk behavior or who are HIV infected. In addition to being screened, coagulation factors used to treat hemophilia and other blood disorders are made safe through heat treatments to inactivate the virus. Screening has significantly reduced the risk of transmission of HIV by blood products and organ donations.
When a person has an STD infection such as chlamydia or gonorrhea, the risk of HIV infection increases and HIV may also increase the risk for other STDs. This may result from any of the following: open lesions providing a portal of entry for pathogens; STDs decreasing the host’s immune status, resulting in a rapid progression of HIV infection; and HIV changing the natural history of STDs or the effectiveness of medications used in treating STDs (Heymann, 2008).
The nurse serves both as an educator about the modes of transmission and as a role model for how to behave toward and provide supportive care for those with HIV infection. An understanding of how transmission does and does not occur will help family and community members feel more comfortable in relating to and caring for persons with HIV (see Box 14-1).
Epidemiology of HIV/AIDS
Worldwide 38 million persons live with HIV infection. Sub-Saharan Africa accounts for two thirds of all HIV infections (UNAIDS, 2009). The epidemic is also growing in central Asia and Eastern Europe (USAID, 2010). Women are at highest risk for infection because of unprotected sex with infected partners. However, there is some evidence that HIV prevention programs may be changing risk behavior in southern Africa. Worldwide, the treatment of HIV infection has been given higher priority, and the use of HAART has increased to 44% for those who need it. This is up from 2% in 2004 (UNAIDS, 2009).
Nurses must identify the trends of HIV infection in the populations they serve, so that they can screen clients who may be at risk and can adequately plan prevention programs and illness care resources. For example, knowing that AIDS disproportionately affects minorities helps nurses set priorities and plan services for these groups. Factors such as geographic location, age, and ethnic distribution are tracked to more effectively target programs. It is important to identify persons infected with HIV before symptomatic AIDS develops, so that treatment can begin as early as needed.
Since the first cases of AIDS were identified in 1981, the total reported number of persons living with AIDS in the United States has grown to 571,378 in 2007 (CDC, 2009a). Note that this number reflects only those who are living; it does not include those who have died. The prevalence of AIDS has increased from 2004 to 2007, reflecting increased life expectancy from the use of antiretroviral therapy (CDC, 2009a).
Figure 14-1 shows the exposure categories for persons with HIV in 2008. Men who have sex with men (MSM) make up the largest group with HIV in the United States, and the number of persons contracting HIV through heterosexual transmission is the second largest. Heterosexual transmission has surpassed injection drug use (IDU) as the primary mode of HIV transmission in women (CDC, 2006b).
The distribution of pediatric HIV infection has fallen dramatically as a result of prenatal care that includes HIV testing, antiretroviral therapy for the mother, and cesarean delivery. Perinatal HIV transmission has declined, and 92% of pediatric HIV infection results from perinatal exposure (CDC, 2007b).
As seen in Table 14-1, HIV/AIDS has disproportionately affected minority groups. African-Americans make up approximately 12% of the total U.S. population, yet they represent 49% of those reported to have AIDS (CDC, 2010b). This overrepresentation is associated with economically poor, marginalized populations composed of persons who are likely to be urban residents, may use injection drugs, and may use prostitution to obtain illicit drugs.
TABLE 14-1
| RACE/ETHNICITY | MALES (NUMBER) | MALES (RATE) | FEMALES (NUMBER) | FEMALES (RATE) | TOTAL |
| White, non-Hispanic | 16,280 | 19.6 | 3300 | 3.8 | 19,600 |
| African American, non-Hispanic | 16,120 | 115.7 | 8810 | 55.7 | 24,900 |
| Hispanic | 7420 | 43.1 | 2300 | 14.4 | 9700 |
| Asian/Pacific Islander | 1010 | 18.0 | 180 | 3.0 | 1200 |
| Native American/Alaskan Native | 150 | 15.5 | 130 | 12.8 | 290 |
| Total | 41,400 | 34.3 | 15,000 | 11.9 | 56,300 |
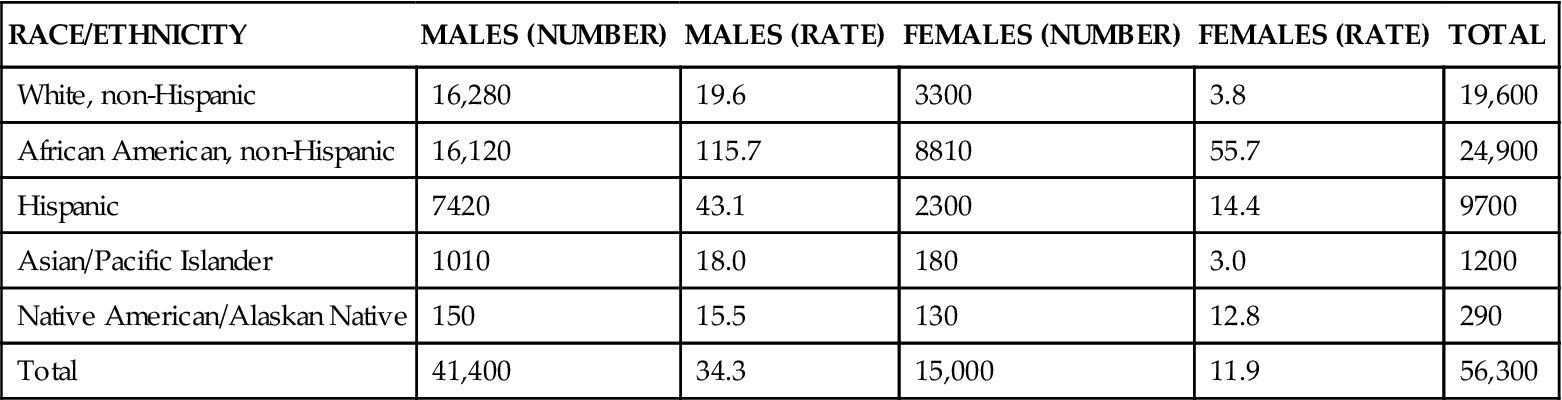
From Centers for Disease Control and Prevention, 2007. Available at http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2007report/pdf/table3.pdf. Accessed December 26, 2010.
The geographic distribution of HIV infection is clustered in urban areas. Regionally, the southern United States and the U.S. territories of the Virgin Islands and Puerto Rico report the highest rates (CDC, 2008). States with AIDS prevalence greater than 12.5 per 100,000 population in 2008 were Florida, New York, New Jersey, Delaware, Maryland, Georgia, South Carolina, Louisiana, California, and the District of Columbia (CDC, 2008).
HIV Surveillance
Study of diagnosed cases of AIDS does not reveal current HIV infection patterns because of the interval between infection with HIV and the onset of clinical disease. Moreover, the effectiveness of antiretroviral drugs given early in the HIV infection before symptoms start provides impetus for early identification of infection. Thus in 2008 confidential reporting of HIV-positive status by name was required in all 50 States and the District of Columbia (CDC, 2010d).
HIV Testing
The HIV antibody test is the most commonly used screening test for determining infection. This test does just as its name implies: it does not reveal whether an individual has symptomatic AIDS, nor does it isolate the virus. It does indicate the presence of the antibody to HIV. The most commonly used form of this test is the enzyme-linked immunosorbent assay (EIA). The EIA effectively screens blood and other donor products. To minimize false-positive results, a confirmatory test, the Western blot, is used to verify the results. False-negative results may also occur after infection and before antibodies are produced. Sometimes referred to as the window period, this can last from 6 weeks to 3 months.
In 2004 the use of oral fluid samples for rapid HIV antibody testing was approved. These tests (OraSure, OraQuick) are 99% accurate and provide results within 20 minutes, allowing immediate results to be given (Greenwald et al, 2006). In addition to the rapid results, this test may appeal to persons who fear having their blood drawn. If the test is positive, it requires a second specific confirmatory test. Another option for rapid test results requires blood and is available under the names Reveal Rapid HIV-1 antibody test and Uni-gold Recombigen HIV test.
Routine testing is recommended for all clients attending health department STD clinics, family planning clinics, community health centers, and primary care offices (CDC, 2006c). Voluntary screening programs for HIV may be either confidential or anonymous; the process for each is unique. Confidential testing involves reporting either by identifying the person’s name and address; this information is considered protected by confidentiality. With anonymous testing, the client is given an identification code number that is attached to all records of the test results and is not linked to the person’s name and address. Demographic data such as the person’s sex, age, and race may be collected, but there is no record of the client’s name and address. An advantage of anonymous testing may be that it increases the number of people who are willing to be tested, because many of those at risk are engaged in illegal activities. The anonymity eliminates their concern about the possibility of arrest or discrimination. However, anonymous testing does not allow for follow-up if the test is positive because the client’s name and address are not available.
Perinatal and Pediatric HIV Infection
Perinatal transmission accounts for nearly all HIV infection in children and can occur during pregnancy, labor and delivery, or breastfeeding. The effectiveness of antiretroviral therapy in pregnant women and newborns in preventing transmission from mother to fetus or infant has made pediatric HIV rates decline sharply. On the basis of the effectiveness of antiviral therapy, it is recommended that HIV testing be a routine part of prenatal care and that all pregnant women be tested for HIV (CDC, 2006b). Rapid testing allows rapid results in women who are giving birth, but have not been previously tested for HIV. HIV prevention in women must remain the primary focus of efforts to reduce pediatric HIV infection.
If left untreated, the clinical picture of pediatric HIV infection involves a shorter incubation period than in adults, and symptoms may occur within the first year of life. The physical signs and symptoms in children include failure to thrive, unexplained persistent diarrhea, developmental delays, and bacterial infections such as TB and severe pneumonia (WHO, 2007).
Detection of HIV infection in infants of infected mothers is made through different tests from those used in children over 18 months. The EIA test is not valid because it tests for antibodies, which in the infant reflect passively acquired maternal antibodies. Thus, a diagnosis of HIV infection in early infancy requires the use of other tests that detect HIV DNA or RNA (Havens and Mofenson, 2009).
Despite having an HIV-infected mother, many children do not acquire HIV/AIDS. However, one or both parents may die from HIV infection. The families of many children with AIDS are impoverished, with limited financial, emotional, social, and health care resources. The added strain of this illness makes many individuals and families unable to provide for the emotional, physical, and developmental needs of affected children.
AIDS in the Community
AIDS is a chronic disease, so individuals continue to live and work in the community. Persons with AIDS have bouts of illness interspersed with periods of wellness when they are able to return to school or work. When ill, much of their care is provided in the home. The nurse teaches families and significant others about personal care and hygiene, medication administration, standard precautions to ensure infection control, and healthy lifestyle behaviors such as adequate rest, balanced nutrition, and exercise.
Adherence to HAART is critical for clients since administration must be consistent to be effective (Heymann, 2008). It is important for nurses to educate clients about accurate medication administration. Peer advocates and persons living with HIV infection who are trained to work with infected persons play a vital role in advocacy and teaching self-care management.
The Americans with Disabilities Act of 1990 and other laws protect persons with asymptomatic HIV infection and AIDS against discrimination in housing, at work, and in other public situations (USDJ, 2010). Policies regarding school and worksite attendance have been developed by most states and localities on the basis of these laws. These policies provide direction for the community’s response when a person develops HIV infection. The nurse can identify resources such as social and financial support services and interpret school and work policies.
Mental health issues such as depression, substance abuse, and bipolar disorder are often present in someone newly diagnosed with HIV. These conditions must be addressed prior to or simultaneously with HIV treatment to be effective.
Nurses can assist employers by educating managers about how to deal with ill or infected workers to reduce the risk of breaching confidentiality or wrongful actions such as termination. Disclosing a worker’s infection to other workers, terminating employment, and isolating an infected worker are examples of situations that have resulted in litigation between employees and employers. The CDC supports workplace issues through programs offered by its Business and Labor Resource Service. (See resources on the evolve website at http://evolve.elsevier.com/Stanhope.)
HIV-infected children should attend school since the benefit of attendance far outweighs the risk of transmitting or acquiring infections. None of the cases of HIV infection in the United States have been transmitted in a school setting. Decisions about educational and care needs should be made by an interprofessional team that includes the child’s physician, the nurse, and the child’s parent or guardian.
Individual decisions about risk to the infected child or others should be based on the behavior, neurological development, and physical condition of the child. Attendance may be inadvisable in the presence of cases of childhood infections, such as chickenpox or measles, within the school, because the immunosuppressed child is at greater risk of suffering complications. Alternative arrangements, such as homebound instruction, might be instituted if a child is unable to control body secretions or displays biting behavior.
Resources
As the number of individuals with HIV/AIDS has increased, services to meet these needs have grown. Voluntary and faith-based service organizations, such as community-based organizations or AIDS support organizations, have developed in many localities to address these needs. These services may include counseling, support groups, legal aid, personal care services, housing programs, and community education programs. Nurses collaborate with workers from community-based organizations in the client’s home and may serve to advise these groups in their supportive work. The federal government and many organizations have established toll-free numbers and websites to provide information, as noted on the Evolve website at http://evolve.elsevier.com/Stanhope.
Sexually Transmitted Diseases
The number of new cases (the incidence) of some STDs, such as gonorrhea, has been declining recently, whereas the numbers of others, such as herpes simplex and chlamydia, continue to increase. Chlamydia is the most commonly reported infectious disease; gonorrhea is the second most common. Because of the impact of STDs on long-term health and the emergence of eight new STDs since 1980, continued attention to their prevention and treatment is vital.
The common STDs listed in Table 14-2 are categorized by cause, either viral or bacterial. The bacterial infections include gonorrhea, syphilis, and chlamydia. Most of these are curable with antibiotics, with the exception of the newly emerging antibiotic-resistant strains of gonorrhea.
TABLE 14-2
SUMMARY OF SEXUALLY TRANSMITTED DISEASES



