Public Health Policy
Objectives
After reading this chapter, the student should be able to do the following:
1. Discuss the structure of the U.S. government and health care roles.
3. Differentiate between the primary bodies of law that affect nursing and health care.
4. Define key terms related to policy and politics.
5. State the relationships between nursing practice, health policy, and politics.
6. Develop and implement a plan to communicate with policy makers on a chosen public health issue.
7. Locate references related to nursing, public health, and health policy.
Key Terms
advanced practice nurse, p. 176
Agency for Healthcare Research and Quality, p. 170
American Association of Colleges of Nursing, p. 180
American Nurses Association, p. 169
block grants, p. 165
boards of nursing, p. 173
categorical funding, p. 172
categorical programs, p. 167
constitutional law, p. 173
devolution, p. 165
health policy, p. 164
judicial law, p. 173
law, p. 164
legislation, p. 173
legislative staff, p. 176
licensure, p. 174
National Institute of Nursing Research, p. 170
nurse practice act, p. 173
Occupational Safety and Health Administration, p. 169
Office of Homeland Security, p. 172
police power, p. 165
policy, p. 164
politics, p. 164
regulation, p. 173
U.S. Department of Health and Human Services, p. 164
World Health Organization, p. 168
—See Glossary for definitions
 Marcia Stanhope, RN, DSN, FAAN
Marcia Stanhope, RN, DSN, FAAN
Dr. Marcia Stanhope is currently employed at the University of Kentucky College of Nursing, Lexington, Kentucky. She has been appointed to the Good Samaritan Foundation Chair and Professorship in Community Health Nursing. She has practiced community and home health nursing, has served as an administrator and consultant in home health, and has been involved in the development of two nurse-managed centers. At one time in her career, she held a public policy fellowship and worked in the office of a U.S. Senator. She has taught community health, public health, epidemiology, policy, primary care nursing, and administration courses. Dr. Stanhope formerly directed the Division of Community Health Nursing and Administration and served as Associate Dean of the College of Nursing at the University of Kentucky. She has been responsible for both undergraduate and graduate courses in population-centered nursing. She has also taught at the University of Virginia and the University of Alabama, Birmingham. Her presentations and publications have been in the areas of home health, community health and community-focused nursing practice, as well as primary care nursing.
Nurses are an important part of the health care system and are greatly affected by governmental and legal systems. Nurses who select the community as their area of practice must be especially aware of the impact of government, law, and health policy on nursing, health, and the communities in which they practice. Insight into how government, law, and political action have changed over time is necessary to understand how the health care system has been shaped by these factors. Also, understanding how these factors have influenced the current and future roles for nurses and the public health system is critical for better health policy for the nation. Nurses have historically viewed themselves as advocates for the health of the population. It is this heritage that has moved the discipline into the policy and political arenas. To secure a more positive health care system, nurse professionals must develop a working knowledge of government, key governmental and quasi-governmental organizations and agencies, health care law, the policy process, and the political forces that are shaping the future of health care. This knowledge and the motivation to be an agent of change in the discipline and in the community are necessary ingredients for success as a population-centered nurse.
Definitions
To understand the relationship between health policy, politics, and laws, one must first understand the definitions of the terms. Policy is a settled course of action to be followed by a government or institution to obtain a desired end. Public policy is described as all governmental activities, direct or indirect, that influence the lives of all citizens (Birkland, 2005). Health policy, in contrast, is a set course of action to obtain a desired health outcome for an individual, family, group, community, or society. Policies are made not only by governments, but also by such institutions as a health department or other health care agency, a family, or a professional organization.
Politics plays a role in the development of such policies. Politics is found in families, professional and employing agencies, and governments. Politics determines who gets what and when and how they get it (Birkland, 2005). Politics is the art of influencing others to accept a specific course of action. Therefore, political activities are used to arrive at a course of action (the policy). Law is a system of privileges and processes by which people solve problems based on a set of established rules; it is intended to minimize the use of force. Laws govern the relationships of individuals and organizations to other individuals and to government. Through political action, a policy may become a law, a regulation, a judicial ruling, a decision, or an order.
After a law is established, regulations further define the course of action (policy) to be taken by organizations or individuals in reaching an outcome. Government is the ultimate authority in society and is designated to enforce the policy whether it is related to health, education, economics, social welfare, or any other society issue. The following discussion explains the role of government in health policy.
Governmental Role in U.S. Health Care
In the United States, the federal and most state and local governments are composed of three branches, each of which has separate and important functions. The executive branch is composed of the president (or state governor or local mayor) along with the staff and cabinet appointed by this executive, various administrative and regulatory departments, and agencies such as the U.S. Department of Health and Human Services (USDHHS). The legislative branch (i.e., Congress at the federal level) is made up of two bodies: the Senate and the House of Representatives, whose members are elected by the citizens of particular geographic areas.
The judicial branch is composed of a system of federal, state, and local courts guided by the opinions of the Supreme Court. Each of these branches is established by the Constitution, and each plays an important role in the development and implementation of health law and public policy.
The executive branch suggests, administers, and regulates policy. The role of the legislative branch is to identify problems and to propose, debate, pass, and modify laws to address those problems. The judicial branch interprets laws and their meaning, as in its ongoing interpretation of states’ rights to define access to reproductive health services to citizens of the states.
One of the first constitutional challenges to a federal law passed by Congress was in the area of health and welfare in 1937, after the 74th Congress had established unemployment compensation and old-age benefits for U.S. citizens (U.S. Law, 1937a). Although Congress had created other health programs previously, its legal basis for doing so had never been challenged. In Stewart Machine Co. v. Davis (U.S. Law, 1937b), the Supreme Court (judicial branch) reviewed this legislation and determined, through interpretation of the Constitution, that such federal governmental action was within the powers of Congress to promote the general welfare. It was obvious in 2008 and beyond that unemployment benefits are important to the economy and to individuals who lose jobs during a national economic crisis (BLS, 2010).
Most legal bases for the actions of Congress in health care are found in Article I, Section 8 of the U.S. Constitution, including the following:
1. Provide for the general welfare.
2. Regulate commerce among the states.
3. Raise funds to support the military.
Through a continuing number and variety of cases and controversies, these Section 8 provisions have been interpreted by the courts to appropriately include a wide variety of federal powers and activities. State power concerning health care is called police power. This power allows states to act to protect the health, safety, and welfare of their citizens. Such police power must be used fairly, and the state must show that it has a compelling interest in taking actions, especially actions that might infringe on individual rights. Examples of a state using its police powers include requiring immunization of children before being admitted to school and requiring case finding, reporting, treating, and follow-up care of persons with tuberculosis. These activities protect the health, safety, and welfare of state citizens.
Trends and Shifts in Governmental Roles
The government’s role in health care at both the state and federal level began gradually. Wars, economic instability, and political differences between parties all shaped the government’s role. The first major federal governmental action relating to health was the creation in 1798 of the Public Health Service (PHS). Then in 1890 federal laws were passed to promote the public health of merchant seaman and Native Americans. In 1934 Senator Wagner of New York initiated the first national health insurance bill. The Social Security Act of 1935 was passed to provide assistance to older adults and the unemployed, and it offered survivors’ insurance for widows and children. It also provided for child welfare, health department grants, and maternal and child health projects. In 1948 Congress created the National Institutes of Health (NIH), and in 1965 it passed very important health legislation—creating Medicare and Medicaid to provide health care service payments for older adults, the disabled, and the categorically poor. These legislative acts by Congress created programs that were implemented by the executive branch. In March 2010, the most recent legislation passed and signed by President Obama to improve the health of the nation and access to care was the health reform law, the Patient Protection and Affordable Care Act (US LAW, PL 111-148). The legislation was designed to do the following:
• Improve the nation’s fiscal health by reducing the federal deficit by more than $100 billion over the next decade, and more than $1 trillion in the decade after that.” (Kaiser Family Foundation, 2010a)
The U.S. Department of Health and Human Services (USDHHS) (known first as the Department of Health, Education, and Welfare [DHEW]) was created in 1953. The Health Care Financing Administration (HCFA) was created in 1977 as the key agency within the USDHHS to provide direction for Medicare and Medicaid. In 2002 HCFA was renamed the Center for Medicare and Medicaid Services (CMS). During the 1980s, a major effort of the Reagan administration was to shift federal government activities, including federal programs for health care, to the states. The process of shifting the responsibility for planning, delivering, and financing programs from the federal level to the states is called devolution. Throughout the 1980s and 1990s, Congress has increasingly funded health programs by giving block grants to the states. Devolution processes including block granting should alert professional nurses that state and local policy has grown in importance to the health care arena. With the new health reform law, stimulus grants are being provided to state and local areas to improve health care access (HRSA, 2010).
The role of government in health care is shaped both by the needs and demands of its citizens and by the citizens’ beliefs and values about personal responsibility and self-sufficiency. These beliefs and values often clash with society’s sense of responsibility and need for equality for all citizens. A federal example of this ideological debate occurred in the 1990s over health care reform. The Democratic agenda called for a health care system that was universally accessible, with a focus on primary care and prevention. The Republican agenda supported more modest changes within the medical model of the delivery system. This agenda also supported reducing the federal government’s role in health care delivery through cuts in Medicare and Medicaid benefits. The Democrats proposed the Health Security Act of 1993, which failed to gain Congress’s approval. In an effort to make some incremental health care changes, both the Democrats and the Republicans in Congress passed two new laws. The Health Insurance Portability and Accountability Act (HIPAA) allows working persons to keep their employee group health insurance for up to 16 months after they leave a job (U.S. Law 107-105, 1996). The State Child Health Improvement Act (SCHIP) of 1997 provides insurance for children and families who cannot otherwise afford health insurance (U.S. Law, 1997).
With the new health care reform debates, numerous debates occurred in the House of Representatives and the Senate until there was agreement that the Senate version of the bill would be passed. On March 30, 2010 President Obama signed into law the Health Care and Education Reconciliation Act of 2010, which made some changes to the comprehensive health reform law and included House amendments to the new law (Kaiser, 2010a).
This discussion has focused primarily on trends in and shifts between different levels of government. An additional aspect of governmental action is the relationship between government and individuals. Freedom of individuals must be balanced with governmental powers. After the terrorist attacks on the United States in September (World Trade Center attack) and October (anthrax outbreak) of 2001, much government activity was being conducted in the name of protecting the safety of U.S. citizens.
It is interesting to note that before September 11, 2001, the congress and President, recognizing that the public health system infrastructure needed help, passed a law in 2000: “The Public Health Threats and Emergencies Act” (PL 106-505). This was the “first federal law to comprehensively address the public health system’s preparedness for bioterrorism and other infectious disease outbreaks” (Frist, 2002, p 120). This legislation is said to have signaled the beginning of renewed interest in public health as the protector for entire communities. In June 2002 the Public Health Security and Bioterrorism Preparedness and Response Act was signed into law (PL 107-188) in December 2002, with $3 billion appropriated by Congress, to implement the following antibioterrorism activities:
• Improving public health capacity
• Upgrading of health professionals’ ability to recognize and treat diseases caused by bioterrorism
• Speeding the development of new vaccines and other countermeasures
• Improving water and food supply protection
• Tracking and regulating the use of dangerous pathogens within the United States (Frist, 2002)
Yet it remains unclear just how much governmental intervention is necessary and effective and how much will be tolerated by citizens. For example, in 2010 approximately 49% of citizens were against the new health care reform acts, and the Republicans were seen as being obstructionists. A bill was also introduced into the House of Representatives to form a citizens’ alliance for health care reform. From this example, it shows how unclear government actions are when looking at citizen reactions (The Citizens’ Alliance, 2010).
Government Health Care Functions
Federal, state, and local governments carry out five health care functions, which fall into the general categories of direct services, financing, information, policy setting, and public protection.
Direct Services
Federal, state, and local governments provide direct health services to certain individuals and groups. For example, the federal government provides health care to members and dependents of the military, certain veterans, and federal prisoners. State and local governments employ nurses to deliver a variety of services to individuals and families, frequently on the basis of factors such as financial need or the need for a particular service, such as hypertension or tuberculosis screening, immunizations for children and older adults, and primary care for inmates in local jails or state prisons. The Evidence-Based Practice box presents a study that examined the use of a state health insurance program.
Financing
Governments pay for some health care services; the current percentage of the bill paid by the government is about 45.3%, and this is projected to increase to 47.6% by the year 2015. The government also pays for training some health personnel and for biomedical and health care research (NCHS, 2010). Support in these areas has greatly affected both consumers and health care providers. Federal governments finance the direct care of clients through the Medicare, Medicaid, Social Security, and SCHIP programs. State governments contribute to the costs of Medicaid and SCHIP programs. Many nurses have been educated with government funds through grants and loans, and schools of nursing, in the past, have been built and equipped using federal funds. Governments also have financially supported other health care providers, such as physicians, most significantly through the program of Graduate Medical Education funds. The federal government invests in research and new program demonstration projects, with NIH receiving a large portion of the monies. The National Institute of Nursing Research (NINR) is a part of the NIH and, as such, provides a substantial sum of money to the discipline of nursing for the purpose of developing the knowledge base of nursing and promoting nursing services in health care (NINR, 2010).
Information
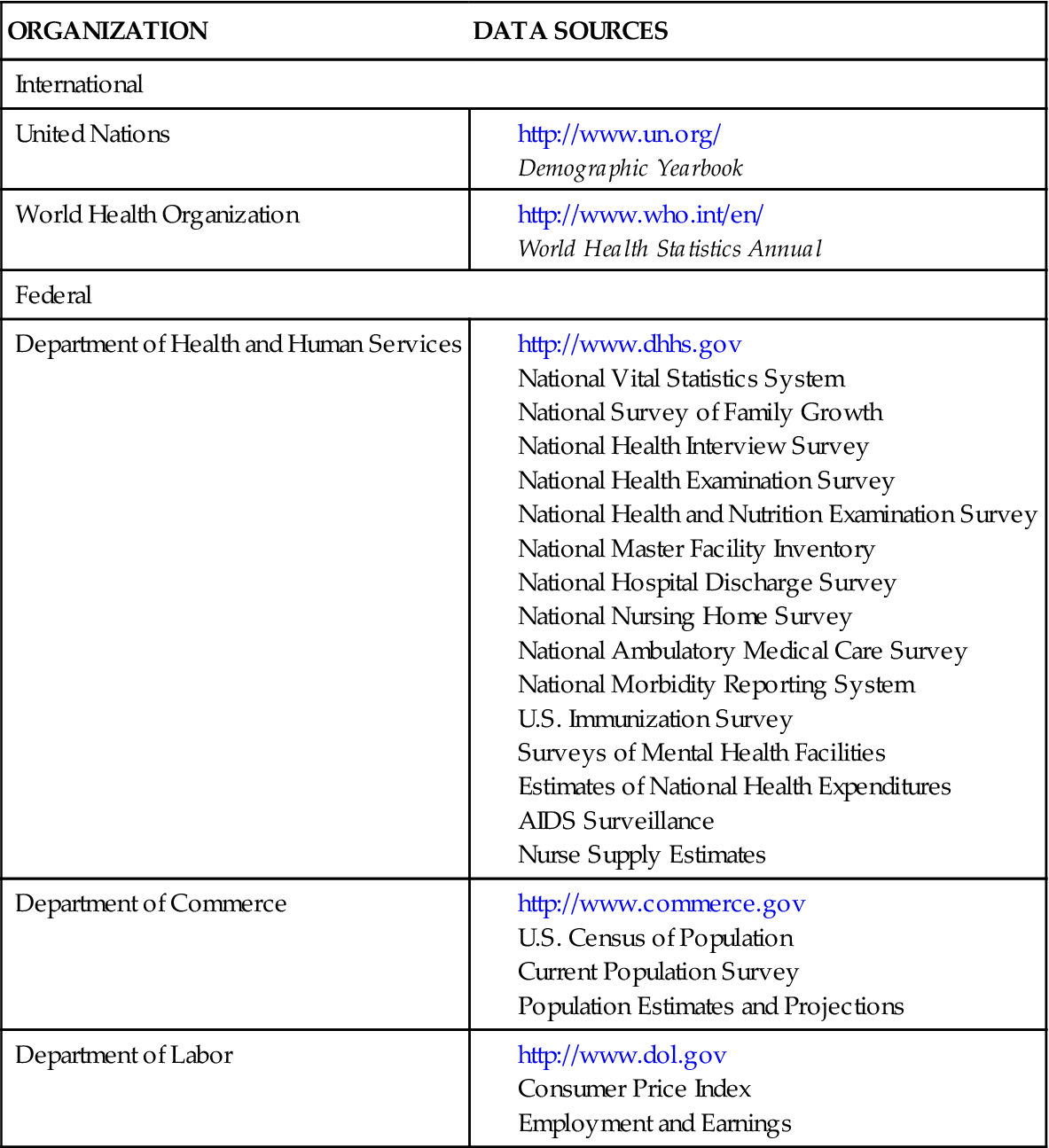
All branches and levels of government collect, analyze, and disseminate data about health care and health status of the citizens. An example is the annual report Health: United States, 2009, compiled each year by the USDHHS (NCHS, 2010). Collecting vital statistics, including mortality and morbidity data, gathering of census data, and conducting health care status surveys are all government activities. Table 8-1 lists examples of available federal and international data sources on the health status of populations in the United States and around the world. These sources are available on the Internet and in the governmental documents’ section of most large libraries. This information is especially important because it can help nurses understand the major health problems in the United States and those in their own states and local communities.
TABLE 8-1
INTERNATIONAL AND NATIONAL SOURCES OF DATA ON THE HEALTH STATUS OF THE U.S. POPULATION
Policy Setting
Policy setting is a chief governmental function. Governments at all levels and within all branches make policy decisions about health care. These health policy decisions have broad implications for financial expenses, resource use, delivery system change, and innovation in the health care field. One law that has played a very important role in the development of public health policy, public health nursing, and social welfare policy in the United States is the Sheppard-Towner Act of 1921 (USDHHS, 2009; USDHHS, HRSA, 2010).
The Sheppard-Towner Act made nurses available to provide health services for women and children, including well-child and child-development services; provided adequate hospital services and facilities for women and children; and provided grants-in-aid for establishing maternal-child welfare programs. The act helped set precedents and patterns for the growth of modern-day public health policy. It defined the role of the federal government in creating standards to be followed by states in conducting categorical programs, such as the Women, Infants, and Children (WIC) and Early Periodic Screening and Developmental Testing (EPSDT) programs. The act also defined the position of the consumer in influencing, formulating, and shaping public policy; the government’s role in research; a system for collecting national health statistics; and the integrating of health and social services. This act established the importance of prenatal care, anticipatory guidance, client education, and nurse-client conferences, all of which are viewed today as essential nursing responsibilities.
Public Protection
The U.S. Constitution gives the federal government the authority to provide for the protection of the public’s health. This function is carried out in numerous venues, such as by regulating air and water quality and protecting the borders from the influx of diseases by controlling food, drugs, and animal transportation, to name a few. The Supreme Court interprets and makes decisions related to public health, such as affirming a woman’s rights to reproductive privacy (Roe v. Wade), requiring vaccinations, and setting conditions for states to receive public funds for highway construction/repair by requiring a minimum drinking age.
Healthy People 2020: an Example of National Health Policy Guidance
In 1979 the surgeon general issued a report that began a 30-year focus on promoting health and preventing disease for all Americans (DHEW, 1979). In 1989, Healthy People 2000 became a national effort with many stakeholders representing the perspectives of government, state, and local agencies; advocacy groups; academia; and health organizations (USDHHS, 1991.
Throughout the 1990s states used Healthy People 2000 objectives to identify emerging public health issues. The success of this national program was accomplished and measured through state and local efforts. The Healthy People 2010 document focused on a vision of healthy people living in healthy communities. Healthy People 2020 has four overarching goals, which can be found in the Healthy People 2020 box; this box compares the goals of Healthy People documents from 2000 to 2020.
Organizations and Agencies that Influence Health
International Organizations
In June 1945, following World War II, many national governments joined together to create the United Nations (UN). By charter, the aims and goals of the UN deal with human rights, world peace, international security, and the promotion of economic and social advancement of all the world’s peoples. The UN, headquartered in New York City, is made up of six principal divisions, several subgroups, and many specialized agencies and autonomous organizations. With the approval and support of the UN Commission on the Status of Women, five world conferences on women have been held. At these conferences, the health of women and children and their rights to personal, educational, and economic security as well as initiatives to achieve these goals at the country level were debated and explored, and policies were formulated (United Nations, 1975, 1980, 1985, 1995, 2000).
One of the special autonomous organizations growing out of the UN is the World Health Organization (WHO). Established in 1946, WHO relates to the UN through the Economic and Social Council to achieve its goal to attain the highest possible level of health for all persons. “Health for All” is the creed of the WHO. Headquartered in Geneva, Switzerland, the WHO has six regional offices. The office for the Americas is located in Washington, DC, and is known as the Pan American Health Organization (PAHO). The WHO provides services worldwide to promote health, it cooperates with member countries in promoting their health efforts, and it coordinates the collaborating efforts between countries and the disseminating of biomedical research. Its services, which benefit all countries, include a day-to-day information service on the occurrence of internationally important diseases; the publishing of the international list of causes of disease, injury, and death; monitoring of adverse reactions to drugs; and establishing of world standards for antibiotics and vaccines. Assistance available to individual countries includes support for national programs to fight disease, to train health workers, and to strengthen the delivery of health services. The World Health Assembly (WHA) is the WHO’s policy-making body, and it meets annually. The WHA’s health policy work provides policy options for many countries of the world in their development of in-country initiatives and priorities; however, although WHA policy statements are important everywhere, they are guides and not law. The WHA’s most recent policy statement on nursing and midwifery was released in 2003, and the current worldwide shortage of professional nurses is now on the WHO agenda and is being addressed by country (WHA, 2003;WHO, 2010).
The World Health Report, first published in 1995, is WHO’s leading publication. Each year the report combines an expert assessment of global health, including statistics relating to all countries, with a focus on a specific subject. The main purpose of the report is to provide countries, donor agencies, international organizations, and others with the information they need to help them make policy and funding decisions. In the 2010 report, the WHO mapped out what countries can do to modify their financing systems so they can move more quickly toward this goal—universal coverage—and sustain the gains that have been achieved. The report builds on new research and lessons learned from country experience. It provides an action agenda for countries at all stages of development and proposes ways that the international community can better support efforts in low-income countries to achieve universal coverage and improve health outcomes (WHO, 2010).
The presence of nursing in international health is increasing. Besides offering direct health services in every country in the world, nurses serve as consultants, educators, and program planners and evaluators. Nurses focus their work on a variety of public health issues, including the health care workforce and education, environment, sanitation, infectious diseases, wellness promotion, maternal and child health, and primary care. Dr. Naeema Al-Gasseer of Bahrain has served as the scientist for nursing and midwifery at the WHO; Marla Salmon, dean of nursing at The University of Washington, chaired a Global Advisory Group on Nursing and Midwifery; and Linda Tarr Whelan served as the U.S. Ambassador to the UN Commission on the Status of Women. Virginia Trotter Betts, past president of the American Nurses Association (ANA), served as a U.S. delegate to both the WHA and the Fourth World Conference on Women in Beijing in 1995, where she participated on the negotiating team of the conference to develop a platform on the health of women across the life span. Many U.S. nurse leaders, such as Dr. Carolyn Williams, current author in this book, have been WHO consultants.
Federal Health Agencies
Laws passed by Congress may be assigned to any administrative agency within the executive branch of government for implementing, supervising, regulating, and enforcing. Congress decides which agency will monitor specific laws. For example, most health care legislation is delegated to the USDHHS. However, legislation concerning the environment would most likely be implemented and monitored by the Environmental Protection Agency (EPA), and that concerning occupational health by the Occupational Safety and Health Administration (OSHA) in the U.S. Department of Labor.
U.S. Department of Health and Human Services
The USDHHS is the agency most heavily involved with the health and welfare of U.S. citizens. It touches more lives than any other federal agency. The following agencies have been selected for their relevance to this chapter.
Health Resources and Services Administration
The Health Resources and Services Administration (HRSA) has been a long-standing contributor to the improved health status of Americans through the programs of services and health professions education that it funds. The HRSA contains the Bureau of Health Professions (BHPr), which includes the Division of Nursing as well as the Divisions of Medicine, Dentistry, and Allied Health Professions. The Division of Nursing is the key federal focus for nursing education and practice, and it provides national leadership to ensure an adequate supply and distribution of qualified nursing personnel to meet the health needs of the nation.
The Division of Nursing has the following strategic goals (USDHHS, 2010):
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


