Public Health and Primary Health Care Systems and Health Care Transformation
Objectives
After reading this chapter, the student should be able to do the following:
2. Define public health and primary health care and explain the nursing roles in each.
4. Describe the current public health system in the United States.
5. Compare and contrast the responsibilities of the federal, state, and local public health systems.
Key Terms
Affordable Health Care for America Act, p. 60
American Recovery and Reinvestment Act of 2009, p. 48
disease prevention, p. 54
disparities, p. 45
electronic health record, p. 51
globalization, p. 52
health care reform, p. 45
Healthy People 2020, p. 54
Institute of Medicine, p. 45
managed care, p. 54
medically underserved areas, p. 56
primary health care, p. 53
public health, p. 45
public health system, p. 56
sentinel events, p. 50
World Health Organization, p. 52
—See Glossary for definitions
 Bonnie Jerome-D’Emilia, PhD, MPH, RN
Bonnie Jerome-D’Emilia, PhD, MPH, RN
Dr. Bonnie Jerome-D’Emilia is an Assistant Professor of Nursing at Rutgers, The State University of New Jersey, in Camden, New Jersey. Dr. Jerome-D’Emilia is the director of the RN to BSN program at the University and teaches community health, leadership, management, and health policy courses. She taught previously at the University of Virginia School of Nursing, where she coordinated the Health Systems Management Master’s program and distance learning. Her research and publications focus on diffusion of innovation in health care and specifically in the treatment of breast cancer in the United States.
It has been said about health care that the only constant is change. Yet if we look back at predictions made in the final years of the twentieth century, the changes that have come to pass are not those that were expected. We thought in 2000 that although our health care system was expensive, and that access and quality were not optimal, the infrastructure was such that we could meet the challenges of the major killers of the time—cardiovascular disease and cancer. However, we had not yet considered the report published by the Institute of Medicine that found that between 44,000 and 98,000 people die each year as a result of preventable medical errors (IOM, 2000). In addition, we had not yet lived through the nightmare of September 11, 2001, when we learned that terrorism could strike on American soil, or August 29, 2005, when category 3 Hurricane Katrina generated flooding in New Orleans that resulted in the worst natural disaster in U.S. history. We had not yet witnessed the release of a global pandemic warning, which followed the occurrence of the H1N1 flu in Mexico, where 854 cases of the flu and 59 deaths were observed between March 18 and April 23, 2009 (WHO, 2010a). Subsequent transmission across large geographical areas spread laboratory confirmed flu cases to 212 countries, resulting in some 15,292 deaths by February 2010 (WHO, 2010b). Nor had we experienced the release of vast reserves of oil in the Gulf of Mexico in April 2010, affecting the lives of people, animals, and the water and land themselves.
We had not yet begun to fund the Global Health Initiative, in which the U.S. government would eventually invest $63 billion over 6 years to assist partner countries to improve the provision of care in the following areas: HIV/AIDS, malaria, tuberculosis, maternal and child health, nutrition, family planning and reproductive health, and neglected tropical diseases. This initiative, which emphasizes a “women and girl approach” in the provision of health care (in recognition of the central role of women in the health of their families and communities) also recognizes that the United States cannot fund these programs indefinitely, and so self sustainability must be integrated into the partner countries’ health systems (Office of U.S. Global AIDS Coordinator, 2010). Most significantly, we had not foreseen that the Presidential election of 2008 would usher in a major battle in health care reform that may change the face of health care in the United States for decades to come. Perhaps we need to reconsider the magnitude of the changes that have bombarded the health care system in the first decade of the twenty-first century, and state instead that the only constant is revolutionary change.
This chapter discusses a health care system in flux and evolving to meet domestic and global challenges. The health care system in the United States, the trends that affect this system, and the impact of these trends on public health are described. The primary health care and public health systems in the United States are described and differentiated, and the changing priorities of these systems to meet the nation’s needs are identified. Nurses play a pivotal role in meeting these needs, and so the role of the nurse in the health system is presented. Box 3-1 lists selected definitions that will help explain concepts introduced in this chapter.
Current Health Care System in the United States
While technology, disasters (both man-made and natural), and global health crises influence how we think about our health care system, the ongoing indicators of cost, access, and quality continue to cause disparities in the U.S. health care system. Further debate on these issues will drive improvements that will lead nurses into new roles, tasks, and challenges in the decade ahead.
Cost
Beginning in 2008, a historic weakening of the national and global economy—the “Great Recession”—lead to the loss of 7 million jobs in the United States (Economic Report, 2010). Even as the Gross Domestic Product (GDP), an indicator of the economic health of a country, declined in 2009, health care spending continued to grow and reached $2.5 trillion in the same year (Truffer et al, 2010). In the years between 2010 and 2019, national health spending is expected to grow at an average annual rate of 6.1%, reaching $4.5 trillion by 2019, for a share of approximately 19.3% of the GDP. This translates into a projected increase in per capita spending from $8046 in 2009 to $13,387 in 2019 (Centers for Medicare and Medicaid Services, 2009a).
Table 3-1 shows the increases in spending from actual expenditures in 2004 to projections for 2019, a 19% increase in GDP and a 52% increase in per capita spending for this time period. These projections reflect the effects of the recession (beginning in 2008) which included a shift toward more public spending to offset the decline of employer-sponsored insurance. For example, as jobs are lost, employer-sponsored insurance is lost as well, so the numbers of Medicaid recipients rose 6.5% and Medicaid spending increased 9.9% (Truffer et al, 2010). In addition to this increase in public spending, private spending declined, which reflects both the increasing number of uninsured among the newly unemployed as well as the decline of disposable income that could be used to pay for out-of-pocket health care expenses. Although the economy strengthened in 2010, jobs did not correspondingly increase, and this slow return to pre-recession employment kept private spending down. By 2012, it is expected that public payment for health care services (programs such as Medicare, Medicaid and the Children’s Health Insurance Plan) will account for over half the health care purchased in the United States (Truffer et al, 2010).
TABLE 3-1
ACTUAL AND PROJECTED NATIONAL HEALTH EXPENDITURES, 2004-2019
| YEAR | 2004 | 2009 | 2014 | 2019 |
| Percent GDP | 15.6 | 17.3 | 17.4 | 19.3 |
| Per capita spending (dollars) | 6327 | 8046 | 10,048 | 13,387 |
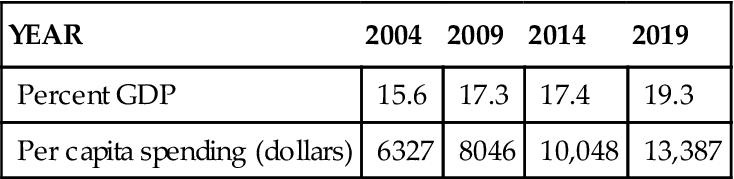
From Centers for Medicare and Medicaid Services: National health projections 2009-2019, forecast summary and selected tables, table 1, 2009. Available at http://www.cms.hhs.gov/NationalHealthExpendData/downloads/proj2009.pdf. Retrieved December 3, 2010.GDP, Gross Domestic Product.
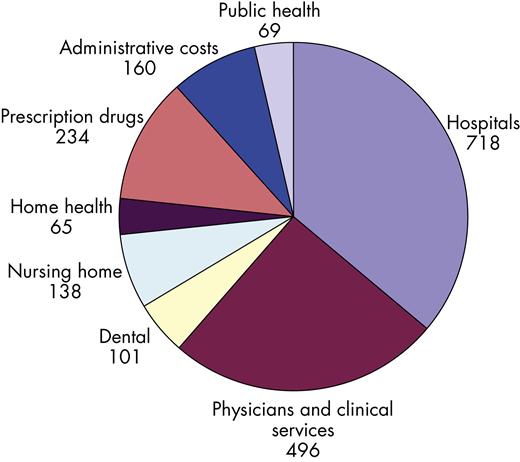
Figure 3-1 illustrates how health care dollars were spent in the year 2008. The largest share of health care expenditures goes to pay for hospital care, with physician services being the next largest item. It is obvious when looking at this chart that the amount of money that has gone to pay for public health services is much lower than the other categories of expenditures. Other significant drivers of the increasingly high cost of health care include:
• Prescription drugs and technology: Prescription drug expenses, although only 10% of health care expenditures in 2008, have been growing rapidly and will continue to do so. Development of new drugs and technologically advanced treatments entail high costs in research and development and lead to an increased demand among consumers (Kaiser Family Foundation, 2009a).
• Chronic disease: At the beginning of the twentieth century, infectious diseases such as pneumonia, flu, and tuberculosis were the major causes of death, and a man who was born in 1900 could expect to die before age 50 (Arias, 2007). At the end of the twentieth century, heart disease and cancer had eclipsed infectious disease as the major causes of death, resulting in the increased costs of prolonged care including nursing home and home health care, as well as costs of medication and treatment.
Following the “Great Recession,” the economic rebound will likely coincide with the burgeoning Medicare enrollment of the aging Baby Boomer population. These new Medicare enrollees will increase Medicare expenditures for the foreseeable future. Medicaid recipients can be expected to decline as jobs are added to the economy, and the percentage of workers covered by employer-sponsored insurance should rise to reflect that growth. Costs will rise as private insurers pass the increased costs of health care onto employers as increased premiums. Employers then pass these premium increases onto their workers, along with higher co-pay and deductible expenses. Although workers’ salaries have not kept pace, employer-sponsored insurance premiums have grown 119% since 1999 (Kaiser Family Foundation, 2009a), and the inability of workers to pay this increased cost has lead to a rise in the percentage of working families who are uninsured.
Access
As costs continue to rise for the provision of health care services, the number of people who can afford to pay for even the most basic care has declined. The U.S. Census Bureau reported that the number of uninsured rose to 46.3 million in 2008 from 45.7 million in 2007, although the percentage of uninsured in the U.S. population remained unchanged at 15.4% of the non-elderly population (DeNavas-Walt, Proctor, and Smith, 2009). In addition, there was a shift to public funding as the number of people insured through private health insurance (including employer-sponsored insurance) decreased by 1 million and the number of people receiving government-provided insurance increased by 4.4 million recipients (DeNavas-Walt, Proctor, and Smith, 2009).
Although 61% of the non-elderly population continues to obtain health insurance through their employer as a benefit, employment does not guarantee insurance (Rowland, Hoffman, and McGinn-Shapiro, 2009). As costs for insurance premiums rise, employers either shift more of these costs to their employees or decline to offer employment-based health coverage at all. This becomes clear when we consider that 9 in 10 (91%) of the middle-class uninsured come from families with at least one full-time worker in jobs that do not offer health insurance or where coverage is unaffordable (Rowland, Hoffman, and McGinn-Shapiro, 2009).
Government programs such as Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP), all described in Box 3-2, play a significant role in meeting the needs of the uninsured. However, as workers lose jobs and employer-sponsored insurance and turn to publically funded programs, states face substantial budget shortfalls, prompting some immediate cuts in the health programs that rely on state funding (Medicaid and CHIP). The continuing growth in the number of uninsured reminds us that there is a significant gap in coverage.
In 2008, 10.8% of white, non-Hispanic Americans were uninsured, compared with 19.1% of African-Americans, 17.6% of Asians, and 30.7% of Latinos (U.S. Census Bureau, 2009). The risk of being uninsured is particularly high for immigrants who are not citizens: 44.7% of non-citizens were uninsured in 2008 (U.S. Census Bureau, 2009). There is a strong relationship between health insurance coverage and access to health care services. Insurance status determines the amount and kind of health care people are able to afford, as well as where they can receive care. The uninsured receive less preventive care, are diagnosed at more advanced disease states, and once diagnosed tend to receive less therapeutic care in terms of surgery and treatment options. A recent study found that as many as 27,000 deaths were the result of a lack of insurance in 2006 (Dorn, 2008).
Even those individuals and families with insurance coverage may find themselves medically underserved. The medically underserved includes those whose insurance does not pay adequately for medical care needed, whose coverage includes high cost sharing and strict limits on covered services, as well as those who live in areas lacking in health care providers. A study in 2007 found that 56 million people in the United States lacked adequate access to primary health care because of shortages of primary health care providers in their communities (National Association of Community Health Centers, 2009). Those who are poor, minority group members, and non-English speakers have the greatest barriers to access.
The uninsured or underinsured have a safety net. There are now more than 6600 federally funded community health centers throughout the United States. The community health center is the backbone of the safety net system. These centers are public and non-profit and receive funding from the federal government. Characteristics of these centers (USDHHS, n.d.a) include the following:
Federally funded community health centers offer a broad range of health and social services, provided by nurse practitioners, physician assistants, physicians, social workers, and dentists. Among the 18 million who received care in these clinics in 2007, one out of every five clients were low-income, uninsured individuals; one in four were low income and members of minority populations; and one in seven were rural residents (National Association of Community Health Centers, 2009).
The American Recovery and Reinvestment Act of 2009 (ARRA), an economic stimulus package designed to offset some of the losses related to the recession, provided $2 billion in additional funding for the nation’s community health centers, including a substantial amount of money to cover the increased demand for services that is likely to occur in a time of rising unemployment. Nineteen states also increased funding for community health centers, although 13 states decreased funding in 2009 because of budgetary shortfalls.
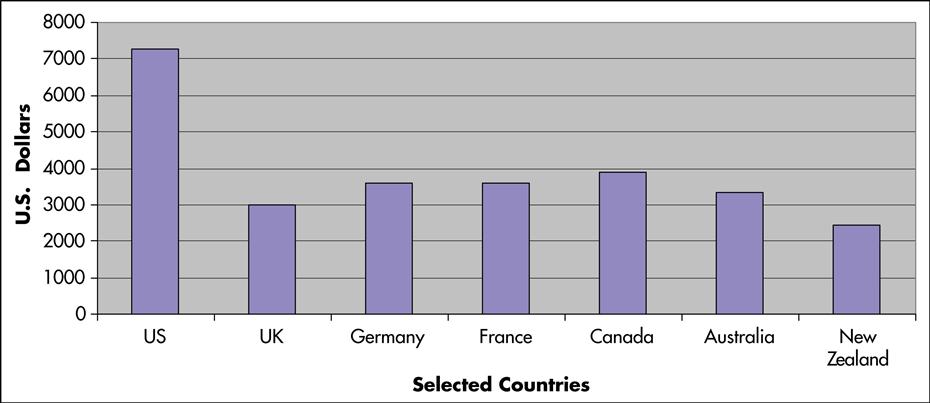
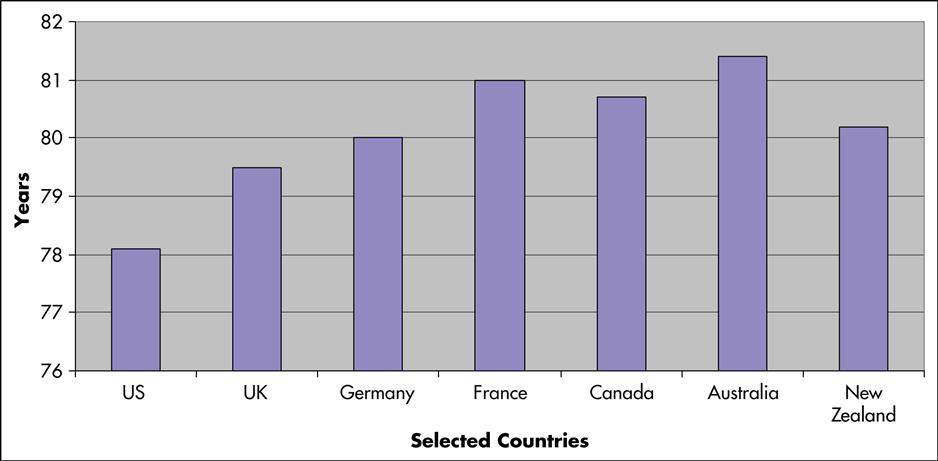
Per capita health spending in the United States continues to exceed spending in the other industrialized countries. Canada, with medical practice styles fairly similar to those in the United States, spent only $5452 per person in 2009, 32% less than the United States (Canadian Institute for Health Information, 2010). In addition, although the United States spends more on health care than any other country (Figure 3-2), when compared with Australia, Canada, Germany, New Zealand, and the United Kingdom, the United States ranks last among these countries in infant mortality and life expectancy (Figure 3-3) (Davis et al, 2007). In 2006, in an international ranking of 191 national health care systems, the United States ranked 43rd for adult female mortality, 42nd for adult male mortality, and 36th for life expectancy (Doe, 2009). These rankings were based on the extent to which the money spent on public health and medical care in these 191 countries improved health, reduced disparities, protected families from impoverishment resulting from medical expenses, and provided services that respect the dignity of clients (Murray and Frenk, 2010).
As the nation’s economy stagnated, it became obvious that the high cost of public funding for health care would only serve to increase the ballooning national deficit. Yet the inequities in access would likely increase unless disparities caused by lack of insurance were addressed as well. The 2008 election ushered in a renewed interest in health reform. Not since President Clinton’s failed effort to pass the Health Security Act in 1993 has an administration attempted a major health reform initiative. The most recent reform efforts were incremental changes or additions to the present system, such as the Children’s Health Insurance Program, passed by President Clinton, and Medicare Part D, the prescription drug coverage addition to the Medicare program, passed during President George W. Bush’s time in office.
President Obama placed the goal of major and systemic health care reform on the top of his agenda and, soon after taking office, instructed the Democratic majorities in the House of Representatives and the Senate to draft a proposal. Debate ensued with much concern over the financial implications of various reform efforts such as the public option, individual mandates, and the health insurance exchange (defined in Box 3-3). Although partisan politics threatened to derail the President’s efforts to pass a major health reform bill in 2010, public concern over health care’s rising costs and lack of access remained high. Indeed, rising health care costs were often cited as the most pressing economic problem in the nation (Teixeira, n.d.). Although the final health care reform bill was more realistically called health insurance reform, its passage by the 111th Congress in March of 2010 was historic; its full enactment, which will take place through 2018, will usher in an era of expanded access to health care in the United States.
Quality
Quality of care leaped to the forefront of concern about health care following the 1999 release of the Institute of Medicine (IOM) report, To Err Is Human: Building a Safer Health System (IOM, 2000). In this groundbreaking report, as many as 98,000 deaths a year were attributed to preventable medical errors. Some of the untoward events categorized in this report included adverse drug events and improper transfusions, surgical injuries and wrong-site surgeries, suicides, restraint-related injuries or death, falls, burns, pressure ulcers, and mistaken client identities. Beyond the cost in human lives, preventable medical errors result in total costs of between $17 billion and $29 billion per year in hospitals nationwide (IOM, 2000). Significant to nurses, the IOM estimated that the number of lives lost to preventable medication errors alone represented more than 7000 deaths annually, with a cost of about $2 billion nationwide. Although the IOM report made it clear that the majority of medical errors today were not produced by provider negligence, lack of education, or lack of training, questions were raised about the nurse’s role and workload and its effect on client safety. In a follow-up report, Keeping Patients Safe: Transforming the Work Environment of Nurses, the IOM (2003) stated that nurses’ long work hours pose one of the most serious threats to client safety, since fatigue slows reaction time, saps energy, and diminishes attention to detail. The group called for state regulators to pass laws barring nurses from working more than 12 hours a day and 60 hours a week—even if by choice (IOM, 2003).
The IOM recommended financial and regulatory incentives to lead to a safer health care system. These recommendations called for the need to stop blaming and punishing individuals for errors and to begin identifying and correcting systems failures by designing safety into the process of care. The Joint Commission (TJC) responded to the report and has developed National Patient Safety Goals specific for each of its accreditation and certification programs (Bleich, 2005). TJC encourages hospitals to report sentinel events, defined as an unexpected occurrence involving death, severe physical or psychological injury, or the risk of injury or death (Liang, 2000; The Joint Commission, 2009). In 2006, TJC began making unannounced hospital inspections.
This culture of safety has made providers and consumers more conscious of safety, but medical errors and untoward events continue to occur. As a means to improve consumer awareness of hospital quality, the Centers for Medicare and Medicaid Services (CMS) began publishing a database of hospital quality measures, Hospital Compare, in 2005. Hospital Compare, a consumer-oriented website that provides information on how well hospitals provide recommended care in such areas as heart attack, heart failure, and pneumonia is available through the CMS website (www.cms.gov). In a further effort, the CMS, in 2008, announced that it will no longer reimburse hospitals for care provided for “preventable complications” such as hospital-acquired infections.
Trends Affecting the Health Care System
Because of the rising national concern with cost, access, and quality of care, it is expected that significant change will occur within the next decade or two. Several trends may shape future changes in the structure of the health care system. These trends include demographics of the population at large and the health care workforce, technology in treatment and in information management, and the recognition that global influences can shape our future.
Demographics
Seventy-seven million babies were born between the years of 1946 and 1963, giving rise to the Baby Boomer generation (Center for Health Communication, 2004). The oldest members of this group turn 65 in 2011, and on average they are expected to live to the age of 83, with many surviving until 90. This generational bubble overwhelmed schools and challenged social norms in childhood and adolescence. Can we expect them to do less as they enter late middle and early old age? Life expectancy has been higher for this group (see Figure 3-3), with much of this increase expected to be attributable to longevity at older age.
In 2007, the number of Medicare beneficiaries reached 44 million, or 15% of the U.S. population, but by 2030 that same population is projected to grow to 79 million (Umans and Nonnemaker, 2009). The cost of Medicare and its share of the GDP is expected to rise astronomically, causing many to think there will be a Medicare shortfall in the middle of this century. The vastly increased numbers of elderly and their greater percentage of the population mean that there will be fewer workers paying taxes into the Medicare system at the same time that the elderly will be consuming more health resources.
A second and equally important demographic trend is the rise in the nation’s foreign-born population: 38.1 million in 2007, or 12.6% of the total U.S. population (U.S. Census Bureau, 2008). Within the foreign-born population, 31% were born in Mexico and an estimated 35 million (12.3%) speak Spanish at home. Following Mexico, the next largest source of immigrants was Asia, and these two geographic areas accounted for 80% of the nation’s foreign-born population in 2007 (Frey et al, 2010).
Twenty-first–century America already looks demographically different than twentieth-century America. The 2000 census showed that America was more ethnically, racially, culturally, and linguistically diverse than ever before. In 2003 the Census Bureau announced that Hispanics now outnumber African-Americans in the United States. States with the largest percentage of foreign-born populations are California, New York, and New Jersey, yet the states with the fastest-growing immigrant populations in 2008 were South Carolina, Georgia, Nevada and Tennessee (Migration Policy Institute, 2010). The Hispanic population is growing most rapidly in the Southeast, the Asian population centers are in the Sun Belt and high-tech areas of the United States, and the African-American population is growing rapidly in the large Southern cities of Atlanta, Houston, and Washington DC (Frey et al, 2010).
The Changing Health Care Workforce
To care for a population that is aging—yet living longer—and is rapidly becoming diverse requires a strong and flourishing health care workforce, yet the workforce faces challenges today.
• In a July 2002 report by the Health Resources and Services Administration, 30 states were found to have shortages of registered nurses in the year 2000. The shortage is projected to intensify over the next two decades, with 44 states and the District of Columbia expected to have RN shortages by the year 2020 (Kaiser Family Foundation, 2008).
• According to projections from the U.S. Bureau of Labor Statistics published in 2004, more than 1 million new and replacement nurses will be needed by 2012. The U.S. Department of Labor has identified registered nursing as the top occupation in terms of job growth through the year 2012 (U.S. Department of Labor, 2008).
• According to an American Association of Colleges of Nursing’s report, preliminery data showed that U.S. nursing schools turned away 52,115 qualified applicants to baccalaureate and graduate nursing programs in 2009 because of a lack of faculty, although other factors such as limitations in clinical sites, classroom space, and clinical preceptors as well as budget constraints were also to blame (AACN, 2005).
In addition to the widespread nursing shortage, chronic, severe workforce shortages among the allied health professions currently exist throughout the United States. According to the U.S. Department of Labor, allied health professionals represent 60% of the American health care workforce, and a shortage of some 1.6 million to 2.5 million allied health workers is predicted by 2020 (Medical News Today, 2006).
Missing Persons: The Lack of Diversity in the Health Care Workforce
Minorities are underrepresented in the physician and nurse workforce relative to their proportion of the total population, but they are overrepresented in lower-paying health professions such as nurse aides and home health aides. The Pew Commission (Grumbach et al, 2003), a national and interprofessional group of health care leaders, suggests that increasing minority representation in the health workforce not only is a commitment to diversity, but also will improve the health care delivery system. The two main arguments that diversity improves health care delivery are: (1) minority health professionals can be expected to practice in underserved areas at a greater rate, and (2) health professionals who share the same culture and language with the clients they serve can provide more effective care (USDHHS, n.d.c; AACN, 2009a).
Technology
Since 2004, when President Bush called for the nationwide adoption of electronic medical records, there has been increased focus on the widespread adoption of innovative technology in health care. This focus has been felt from nursing education, with the increasing number of online nursing programs, to the bedside where personal digital assistants (PDAs) have replaced the pharmacology textbook and bedside computer charting has replaced the paper chart.
The development and refinement of new technologies such as telehealth has opened up new clinical opportunities for nurses, particularly in the management of chronic conditions, home care, rehabilitation, and long-term care. However, along with new opportunities come new challenges and pitfalls. Telehealth, defined as the use of electronic communication networks to transmit client-related information, has been used by the Department of Veterans Affairs to decrease hospitalizations by 20% by improving at-home monitoring of chronically ill clients (Merrill, 2009). And the EmotaMe, an “emotional networking” system unveiled for testing in March 2010, uses concepts from computer games, social networking, and videoconferencing to allow health care providers and family members to monitor and provide emotional, social, and physical support to at-home elderly (Milliard, 2010). Yet while telehealth is seen as a cost-effective way to diagnose and treat rural and isolated clients and to educate rural doctors and nurses, concerns linger about privacy, security, and reimbursement for services provided at a distance and perhaps across state lines.
In the hospital, technology has allowed providers to perform feats of health care that would have been unimaginable just a decade ago. With ultrasound, video-assisted and laser surgery, filmless radiology, robotic pharmacy dispensing, wireless monitoring, and virtual intensive care units, hospitals can provide state-of-the-art care to the sickest of clients. Advanced technology is also being introduced into the health care system as a method of ensuring client safety and improving the quality of care in ways that were addressed by the IOM report on medical errors. The electronic health record (EHR) has been called the most important innovation for client safety, and has been endorsed by Health and Human Services (HHS) Secretary Leavitt (under President Bush) as the means to create a system in which information is digital, privacy protected, and interchangeable (Leavitt, 2010).
An innovative use of the electronic health record to meet the needs of the public health workforce is the ability to embed reminders or guidelines within the EHR. The Practice Partner Research Network’s Colorectal Cancer Screening in Primary Care study looked at the inclusion of reminders for colon cancer screening within a large national group of physicians sharing an EHR system. In this study, evidence-based guidelines were incorporated into progress note templates along with links to previous screening results, and a Health Maintenance section of the EHR was updated with age- and gender-appropriate screening targets. Although screening literature documents the need to overcome barriers that keep clients from following up on screening, such as lack of knowledge and insurance, having a health care provider encourage the need for screening is often the most important factor in fostering client compliance (Shokar, Nguyen-Oghalai, and Wu, 2009). The use of office policies, reminder systems, and communication strategies are crucial tools to enable doctors and nurses to encourage their clients to meet screening goals, and in this study, embedded tools within the EHR resulted in rates of up to 78% in the highest provider practices (Nemeth, Nietert, and Ornstein, 2009).
Publically funded community health centers lag behind private sector health care in adopting and implementing the EHR. In a study by the National Association of Community Health Centers, only 8% of health centers have incorporated the use of electronic records compared with 18% of private physician practices. The overwhelming majority of the community centers cited financial need as the factor that prevented adoption (Smith, 2007). The American Recovery and Reinvestment Act of 2009 included funding to allow community centers to afford the transition to electronic records. Hamilton Community Health Network (Health Care for the Homeless)—a 25-physician, six-center network serving the population of Flint, Michigan, where one in four residents are poor and uninsured—received a $2 million grant to improve facilities and introduce an EHR system (Business Wire, 2009).
Some of the benefits of the EHR for public health (Bower et al, 2005) include the following:
• 24-hour availability of records with downloaded laboratory results and up-to-date assessments
• Coordination of referrals and facilitation of interprofessional care in chronic disease management
• Incorporation of protocol reminders for prevention, screening, and management of chronic disease
• Improvement of quality measurement and monitoring
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


