Pressure Ulcers
Objectives
• Define the key terms and key abbreviations in this chapter.
• Describe the causes and risk factors for pressure ulcers.
• Identify the persons at risk for pressure ulcers.
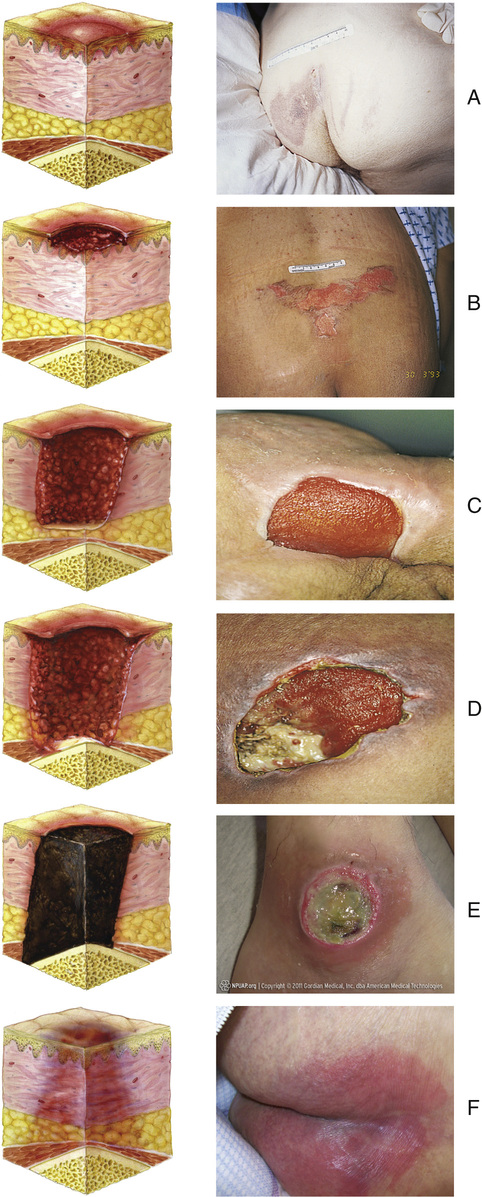
• Describe the stages of pressure ulcers and the Kennedy terminal ulcer.
• Identify the sites for pressure ulcers.
• Explain how to prevent pressure ulcers.
• Identify the complications from pressure ulcers.
• Explain how to promote PRIDE in the person, the family, and yourself.
Key Terms
Before defining pressure ulcer, you need to understand these terms.
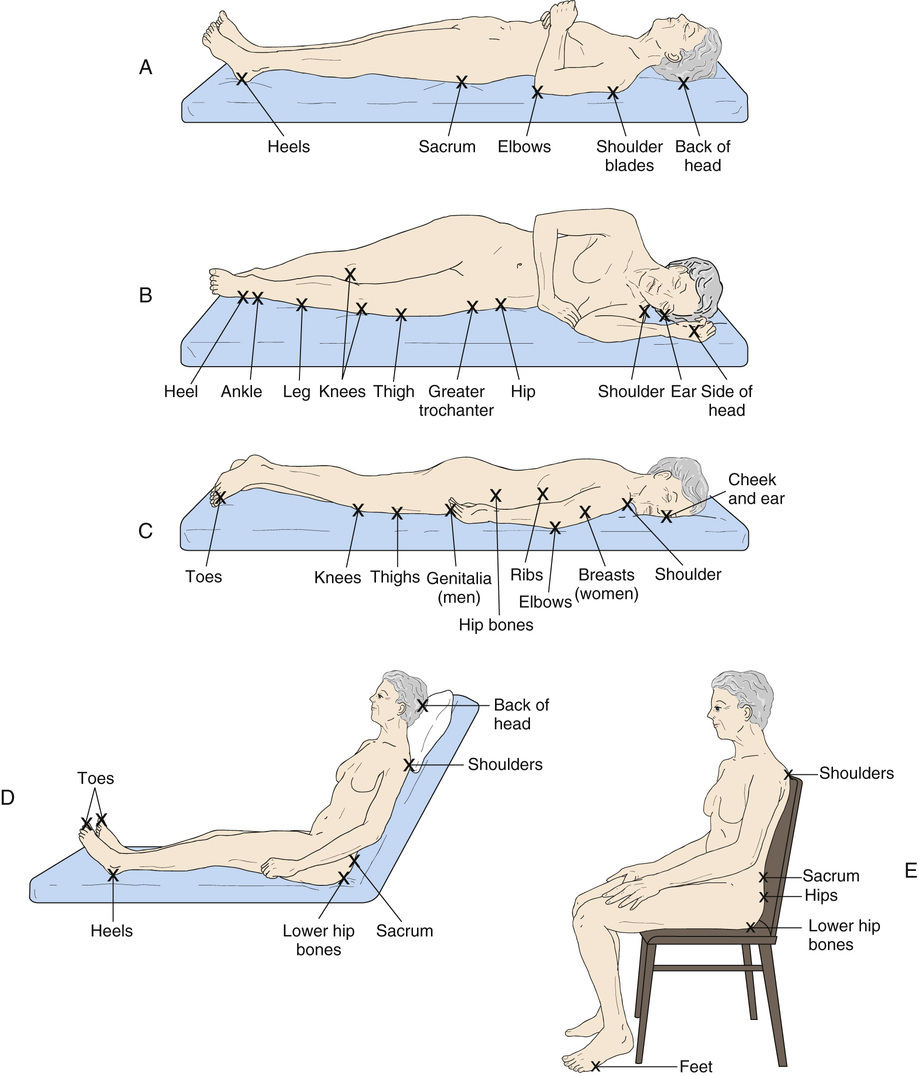
• Bony prominence (pressure point)—an area where the bone sticks out or projects from the flat surface of the body. The back of the hand, shoulder blades, elbows, hips, spine, sacrum, knees, ankles, heels, and toes are bony prominences (Fig. 37-1, p. 622).
• Shear—when layers of the skin rub against each other. Or shear is when the skin remains in place and underlying tissues move and stretch, tearing underlying capillaries and blood vessels. Tissue damage occurs. See Chapter 18.
• Friction—the rubbing of 1 surface against another. The skin is dragged across a surface. Friction is always present with shearing.
Pressure Ulcer Definitions
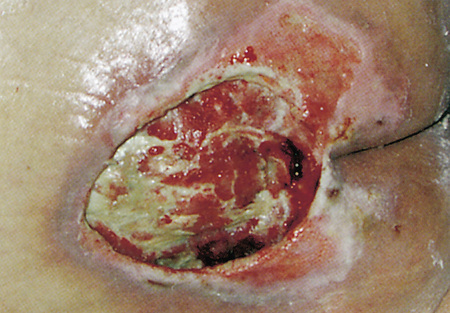
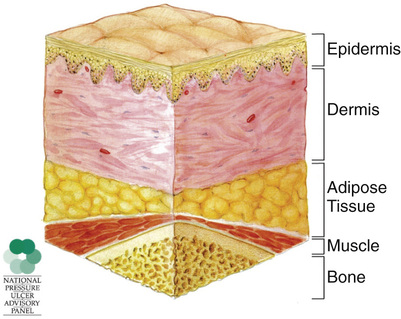
The National Pressure Ulcer Advisory Panel (NPUAP) defines pressure ulcer as a localized injury to the skin and/or underlying tissue, usually over a bony prominence (Fig. 37-2). It is the result of pressure or pressure in combination with shear. Decubitus ulcer, bed sore, and pressure sore are other terms for pressure ulcer.
The Centers for Medicare & Medicaid Services (CMS) defines pressure ulcer as any lesion caused by unrelieved pressure that results in damage to underlying tissues. According to the CMS, friction and shear are factors but not the main causes of pressure ulcers.
Avoidable and Unavoidable Pressure Ulcers
An unavoidable pressure ulcer occurs despite efforts to prevent one through proper use of the nursing process. Such ulcers can develop in hospitals, nursing centers, and home settings. The Kennedy terminal ulcer is unavoidable (p. 626). An avoidable pressure ulcer develops from the improper use of the nursing process.
Agencies must:
• Evaluate the person’s condition and pressure ulcer risk factors.
• Identify and implement measures to meet the person’s needs and goals.
• Monitor and evaluate the effect of such measures.
• Revise the measures as needed.
Agencies must identify persons at risk for pressure ulcers. A person’s risk may increase during an illness (cold, flu) or from condition changes. The person’s care plan must include measures to reduce or remove risk factors.
See Focus on Long-Term Care and Home Care: Avoidable and Unavoidable Pressure Ulcers.
Risk Factors
Pressure, friction, and shearing are the major causes of pressure ulcers. They also cause skin breakdown (Box 37-1) that can lead to pressure ulcers. Skin breakdown involves changes or damage to intact skin. Intact skin is normal skin and skin layers without damage or breaks (Fig. 37-3, p. 624).
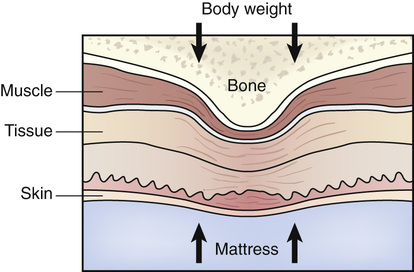
Unrelieved pressure squeezes tiny blood vessels. For example, pressure occurs when the skin over a bony area is squeezed between hard surfaces (Fig. 37-4, p. 624). The bone is 1 hard surface. The other is usually the mattress or chair seat. Squeezing or pressure prevents blood flow to the skin and underlying tissues. Oxygen and nutrients cannot get to the cells. Skin and tissues die.
Friction scrapes the skin, causing an open area. A good blood supply is needed for the open area to heal. A poor blood supply or an infection can lead to a pressure ulcer.
Shear occurs when the person slides down in the bed or chair. Blood vessels and tissues are damaged. Blood flow to the area is reduced.
Other pressure ulcer risk factors include breaks in the skin, poor circulation to an area, moisture, dry skin, and skin irritation by urine and feces.
See Teamwork and Time Management: Risk Factors, p. 624.
Persons at Risk
Persons at risk for pressure ulcers are those who:
• Are bedfast (confined to bed) or chairfast (confined to a chair). Pressure occurs from lying or sitting in the same position too long.
• Have circulatory problems. Cells and tissues die when starved of oxygen and nutrients.
• Are obese. Friction can damage the skin. Persons with bariatric needs are at great risk.
• Have medical devices. A pressure ulcer can develop where medical devices cause pressure on the skin.
• Have a healed pressure ulcer. Healed Stage 3 or 4 pressure ulcers are more likely to recur. See “Pressure Ulcer Stages.”
See Focus on Children and Older Persons: Persons at Risk.
Pressure Ulcer Stages
In persons with light skin, a reddened bony area is the first sign of a pressure ulcer. In persons with dark skin, skin color may differ from surrounding areas. The color change remains after the pressure is relieved. The area may feel warm or cool. The person may complain of pain, burning, tingling, or itching. Or the person may not feel anything unusual. Box 37-2 describes pressure ulcer stages.