Robin Webb Corbett and Laura K. Williford Owens antiflatulents, p. 831 congenital rubella syndrome, p. 836 episiotomy, p. 828 flatus, p. 831 folliculitis, p. 828 lactation, p. 827 necrosis, p. 828 occlusive, p. 828 ophthalmia neonatorum, p. 838 puerperium, p. 827 Rh sensitization, p. 835 RhO(D) immune globulin, p. 836 urticaria, p. 837 This chapter focuses on pharmacologic considerations for mothers and infants after delivery. Nonpharmacologic measures and pharmacologic agents related to the relief of common maternal discomforts during the postpartum period are also described. In addition, drugs commonly administered to newborns immediately after delivery are discussed. During the puerperium (the period from delivery until 6 weeks postpartum), the maternal body physically recovers from antepartal and intrapartal stressors and returns to its prepregnant state. Pharmacologic and nonpharmacologic measures commonly used during the postpartum period have five primary purposes: (1) to prevent uterine atony and postpartum hemorrhage; (2) to relieve pain from uterine contractions, perineal wounds, and hemorrhoids; (3) to enhance or suppress lactation (production and release of milk by mammary glands); (4) to promote bowel function; and (5) to enhance immunity (Box 55-1). Whenever possible, nonpharmacologic measures are preferred to the use of drugs or are used in conjunction with drugs (Herbal Alert 55-1). Postpartum nursing care ideally occurs as a partnership between the nurse and the new family. To enhance health and wellness, the nurse collaborates with the mother and family to strengthen the new mother’s self-confidence and ability to handle her own health challenges. The nurse’s role in this system is threefold: “Afterbirth pains” may occur during the first few days postpartum when uterine tissue experiences ischemia during contractions, particularly in multiparous patients and when breastfeeding. Nonsteroidal agents may be used to control postpartal discomfort and pain, with narcotic agents reserved for more severe pain such as that experienced by the patient after cesarean delivery, tubal ligation, or extensive perineal laceration. Box 55-2 lists systemic analgesics commonly used during the postpartum period. Because some systemic analgesics (e.g., codeine, meperidine) can cause decreased alertness, it is important for the nurse to observe the patient as she cares for her newborn to ensure safety. Patients who receive opioids, such as morphine sulfate or codeine sulfate, should be assessed for bowel function and respirations. With continued opioid use, patient assessment of bowel history is necessary, because these drugs can exacerbate the constipation of pregnancy. During the intrapartum period, women are NPO (nothing by mouth) or ingest limited liquids and are not ambulatory, all factors that contribute to decreased bowel activity. In addition, respiratory assessment is important for patients receiving opioids, because respiratory depression may occur. Frequently nonsteroidal agents like ibuprofen and ketorolac tromethamine are used to control postpartum discomfort and pain. Nonsteroidal antiinflammatory drugs (NSAIDs) inhibit the enzyme cyclooxygenase (COX), of which there are two isoenzymes, COX-1 or COX-2; both decrease prostaglandin synthesis. These drugs are effective in relieving mild to moderate pain caused by postpartum uterine contractions, episiotomy, hemorrhoids, and perineal wounds. NSAIDs commonly cause gastrointestinal (GI) irritation, and it is recommended that patients take them with a full glass of water or with food to minimize GI distress. With administration of NSAIDs, a lower narcotic dosage may control pain as a result of the additive analgesic effect. The use of NSAIDs requires ongoing assessment for GI bleeding. These drugs inhibit platelet synthesis and may prolong bleeding time. Patient teaching with this category of drugs is important, because some NSAIDs may be purchased over the counter (OTC). Patient teaching includes avoidance of these drugs while pregnant if symptoms of GI bleeding occur (dark, tarry stools; blood in urine; coffee-ground emesis) and avoidance of the concurrent use of alcohol, aspirin, and corticosteroids, which may increase the risk for GI toxicity. Pregnancy and the delivery process increase the pressure on perineal soft tissue. The tissue may become ecchymotic or edematous. Increased edema, ecchymosis, and pain may occur if an episiotomy (incision made to enlarge the vaginal opening to facilitate newborn delivery) or perineal laceration is present. The perineum is assessed for Redness, Ecchymosis, Edema, Discharge, and Approximation (REEDA). In addition, hemorrhoids that developed during pregnancy may be exacerbated by the pushing during labor. Comfort measures (ice packs immediately after birth, tightening of the buttocks before sitting, use of peribottles and cool or warm sitz baths) and selected topical agents (witch hazel and dibucaine ointment) may relieve pain and minimize discomfort (Table 55-1). Note that rectal suppositories should not be used by women with fourth-degree perineal lacerations. TABLE 55-1 DRUGS USED TO RELIEVE PAIN FROM PERINEAL WOUNDS AND HEMORRHOIDS The most commonly reported side effects of topical or local agents include burning, stinging, tenderness, edema, rash, tissue irritation, sloughing, and tissue necrosis (death of tissue caused by disease or injury). The most commonly reported side effects of hydrocortisone local or topical drugs include burning, pruritus, irritation, dryness, folliculitis (skin inflammation resulting from contact with an irritating substance or allergen), allergic contact dermatitis, and secondary infection. These side effects are more likely to occur when occlusive (i.e., obstructive) dressings are used. In the past, lactation was commonly controlled through drug therapy with one of three agents: chlorotrianisene (Tace), Deladumone OB (combination of estrogen plus androgen in the form of estradiol valerate and testosterone enanthate), or bromocriptine mesylate (Parlodel). Estrogenic substances are much less popular than in the past because of the increased incidence of thrombophlebitis associated with the high dosage needed to suppress lactation and concerns about potential carcinogenic effects. Although these drugs are not used now, your patients and their families may ask about these medications, which were given in the past for lactation suppression. Presently nonpharmacologic measures are recommended for lactation suppression, such as wearing a supportive bra 24 hours a day for 10 to 14 days or using axillary ice packs) (Table 55-2). Other strategies include taking 200 mg of pyrioxidine (vitamin B6) for 5 days, ingesting sage tea approximately every 6 hours, using 3 to 4 mL of alcohol tincture every 6 hours via the mucous membranes, and applying pounded cold cabbage leaves to breasts and aerola, changing every 30 minutes as cabbage leaves wilt. TABLE 55-2 NONPHARMACOLOGIC MEASURES FOR COMMON POSTPARTUM NEEDS
Postpartum and Newborn Drugs
Objectives
Key Terms
![]() http://evolve.elsevier.com/KeeHayes/pharmacology/
http://evolve.elsevier.com/KeeHayes/pharmacology/
Drugs Used during the Postpartum Period
Pain Relief for Uterine Contractions
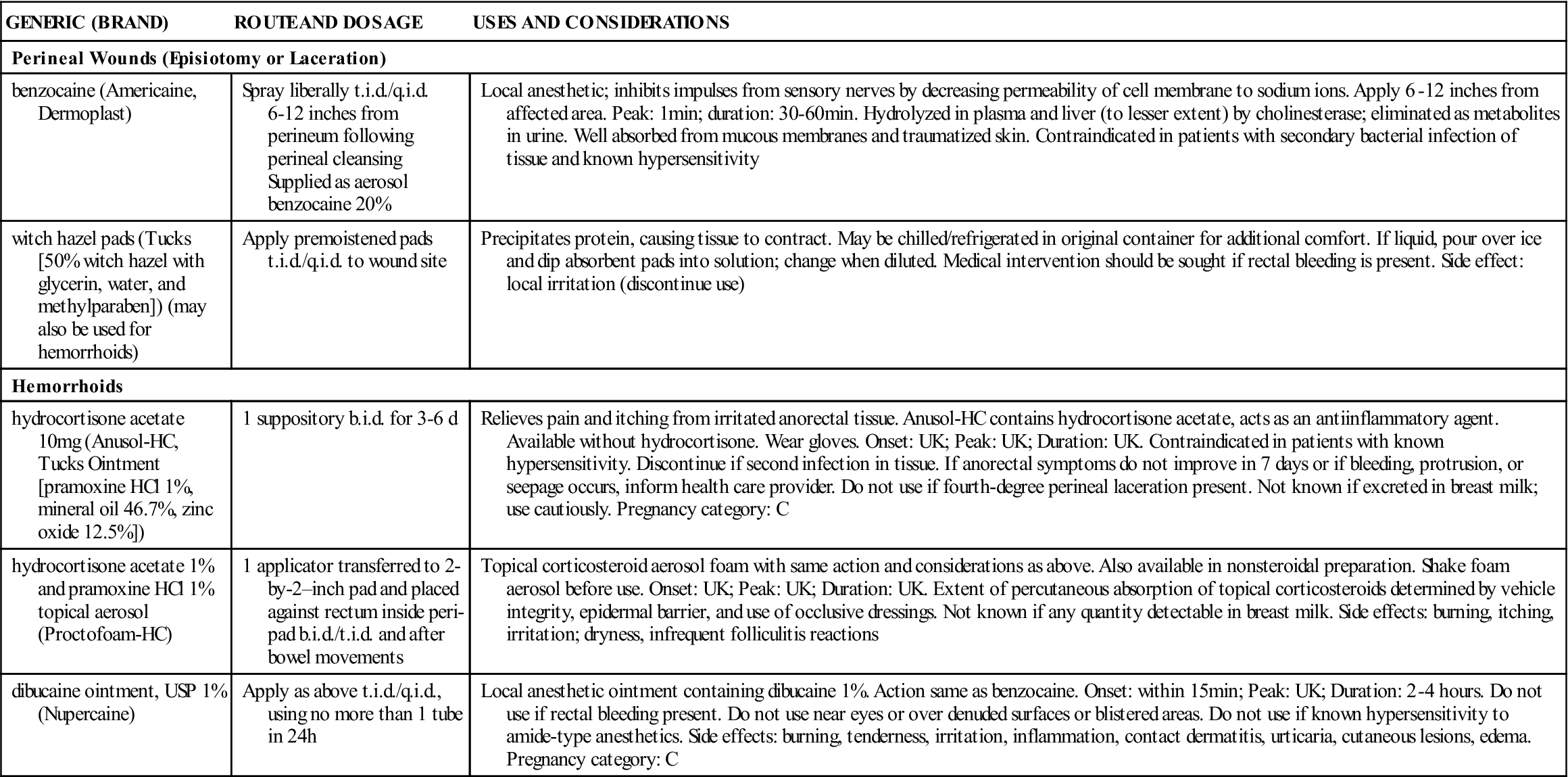
Pain Relief for Perineal Wounds and Hemorrhoids
GENERIC (BRAND)
ROUTE AND DOSAGE
USES AND CONSIDERATIONS
Perineal Wounds (Episiotomy or Laceration)
benzocaine (Americaine, Dermoplast)
Spray liberally t.i.d./q.i.d. 6–12 inches from perineum following perineal cleansing
Supplied as aerosol benzocaine 20%
Local anesthetic; inhibits impulses from sensory nerves by decreasing permeability of cell membrane to sodium ions. Apply 6–12 inches from affected area. Peak: 1 min; duration: 30–60 min. Hydrolyzed in plasma and liver (to lesser extent) by cholinesterase; eliminated as metabolites in urine. Well absorbed from mucous membranes and traumatized skin. Contraindicated in patients with secondary bacterial infection of tissue and known hypersensitivity
witch hazel pads (Tucks [50% witch hazel with glycerin, water, and methylparaben]) (may also be used for hemorrhoids)
Apply premoistened pads t.i.d./q.i.d. to wound site
Precipitates protein, causing tissue to contract. May be chilled/refrigerated in original container for additional comfort. If liquid, pour over ice and dip absorbent pads into solution; change when diluted. Medical intervention should be sought if rectal bleeding is present. Side effect: local irritation (discontinue use)
Hemorrhoids
hydrocortisone acetate 10 mg (Anusol-HC, Tucks Ointment [pramoxine HCl 1%, mineral oil 46.7%, zinc oxide 12.5%])
1 suppository b.i.d. for 3–6 d
Relieves pain and itching from irritated anorectal tissue. Anusol-HC contains hydrocortisone acetate, acts as an antiinflammatory agent. Available without hydrocortisone. Wear gloves. Onset: UK; Peak: UK; Duration: UK. Contraindicated in patients with known hypersensitivity. Discontinue if second infection in tissue. If anorectal symptoms do not improve in 7 days or if bleeding, protrusion, or seepage occurs, inform health care provider. Do not use if fourth-degree perineal laceration present. Not known if excreted in breast milk; use cautiously. Pregnancy category: C
hydrocortisone acetate 1% and pramoxine HCl 1% topical aerosol (Proctofoam-HC)
1 applicator transferred to 2-by-2–inch pad and placed against rectum inside peri-pad b.i.d./t.i.d. and after bowel movements
Topical corticosteroid aerosol foam with same action and considerations as above. Also available in nonsteroidal preparation. Shake foam aerosol before use. Onset: UK; Peak: UK; Duration: UK. Extent of percutaneous absorption of topical corticosteroids determined by vehicle integrity, epidermal barrier, and use of occlusive dressings. Not known if any quantity detectable in breast milk. Side effects: burning, itching, irritation; dryness, infrequent folliculitis reactions
dibucaine ointment, USP 1% (Nupercaine)
Apply as above t.i.d./q.i.d., using no more than 1 tube in 24 h
Local anesthetic ointment containing dibucaine 1%. Action same as benzocaine. Onset: within 15 min; Peak: UK; Duration: 2–4 hours. Do not use if rectal bleeding present. Do not use near eyes or over denuded surfaces or blistered areas. Do not use if known hypersensitivity to amide-type anesthetics. Side effects: burning, tenderness, irritation, inflammation, contact dermatitis, urticaria, cutaneous lesions, edema. Pregnancy category: C
Side Effects and Adverse Reactions
Lactation Suppression





































































