Physiologic Adaptation of the Newborn and Nursing Assessment
Objectives
2. Describe four important neonatal adaptations to extrauterine life.
3. Explain how fluid in the lungs is replaced with air.
4. Relate how the neonate’s pulmonary circulation is established.
5. Differentiate between the three fetal circulatory shunts, including their reasons for closure.
6. Recall the location of brown fat and how it is used in infant heat production.
7. Explain three reasons that the newborn should not be allowed to chill or experience cold stress.
8. Explain four ways to prevent heat loss in the newborn.
9. Recognize the normal range of neonatal vital signs.
10. Describe the assessment of the anterior and posterior fontanelles.
11. Differentiate among molding, cephalohematoma, and caput succedaneum.
12. Review key physical and behavioral assessments of the newborn.
13. Discuss normal newborn reflexes.
Key Terms
acrocyanosis (ak˝ro-si˝ə-no´sis, p. 171)
brown adipose tissue (BAT) (ĂD-ĭ-pōs, p. 167)
cold stress (p. 160)
conduction (p. 165)
convection (p. 165)
cutis marmorata (ku´tis mahr˝mo-ra´ta, p. 171)
desquamation (des˝kwə-ma´shən, p. 171)
ductus arteriosus (p. 162)
ductus venosus (p. 162)
Epstein’s pearls (p. 171)
erythema toxicum (er˝ə-the´mə, p. 171)
evaporation (p. 165)
fontanelles (fon´tə-nel´, p. 170)
foramen ovale (p. 161)
forceps marks (p. 172)
functional residual capacity (FRC) (p. 161)
Harlequin color change (p. 172)
milia (mil´e-ə, p. 172)
miliaria (mil˝e-ar´e-ə, p. 169)
molding (p. 170)
Mongolian spots (p. 172)
nevi (ne´vi, p. 172)
nonshivering thermogenesis (thĕr-mō-JĔN-ĕs ĭs, p. 167)
opisthotonos (o˝pis-thot´ə-nəs, p. 167)
port-wine stain (p. 172)
radiation (p. 167)
surfactant (sŭr-FĂK-tănt, p. 160)
thermoregulation (thĕr-mō-RĔG-ū-LĀ-shŭn, p. 162)
 http://evolve.elsevier.com/Leifer/maternity
http://evolve.elsevier.com/Leifer/maternity
Adjustment to Extrauterine Life
In adapting to life outside of the uterus, the newborn infant must master thermoregulation, metabolic homeostasis, and respiratory gas exchange and convert from fetal to neonatal circulation pathways. These major transitions occur at a time when the infant must also respond to gestational and birth traumas. An understanding of the newborn’s normal adaptation to extrauterine life will enable the nurse to prioritize assessments and nursing interventions and recognize deviations.
To live independently from the mother, the newborn must immediately establish pulmonary ventilation—that is, breathe on his or her own. The newborn must adapt to do the following:
• Quickly breathe and maintain respiration rate
• Replace fluid in the lungs with air
• Open up the pulmonary circulation and close the fetal shunts
• Allow pulmonary blood flow to increase and cardiac output (blood volume) to be redistributed
• Provide energy to maintain body temperature and support metabolic processes
• Dispose of waste products produced by food absorption and metabolic processes
• Detoxify substances entering from the external environment
Respiratory and Circulatory Function
The respiratory and cardiovascular systems are required to quickly adapt to life outside of the uterus. When the cord is clamped, the placental circulation is immediately cut off. The changes that occur in the lungs are described in the following sections.
Preparatory Events to Breathing
In utero, the fetus’s lungs are filled with fluid. This fluid is a combination of secretions of the alveolar cells of the lungs and some amniotic fluid. At birth, air must replace this fluid.
Surfactant, a phospholipid, is produced by the mature lungs in a term fetus. It reduces the force between the moist surfaces of the alveoli, thereby preventing them from collapsing with each expiration and thus promotes lung expansion. Also, surfactant promotes lung compliance (the lung’s ability to easily fill with air). This action is important because, when the newborn begins to breathe, less effort will be required to continue and maintain breathing, reducing the chance that atelectasis (collapsed alveoli of the lung) will occur.
Onset of Breathing
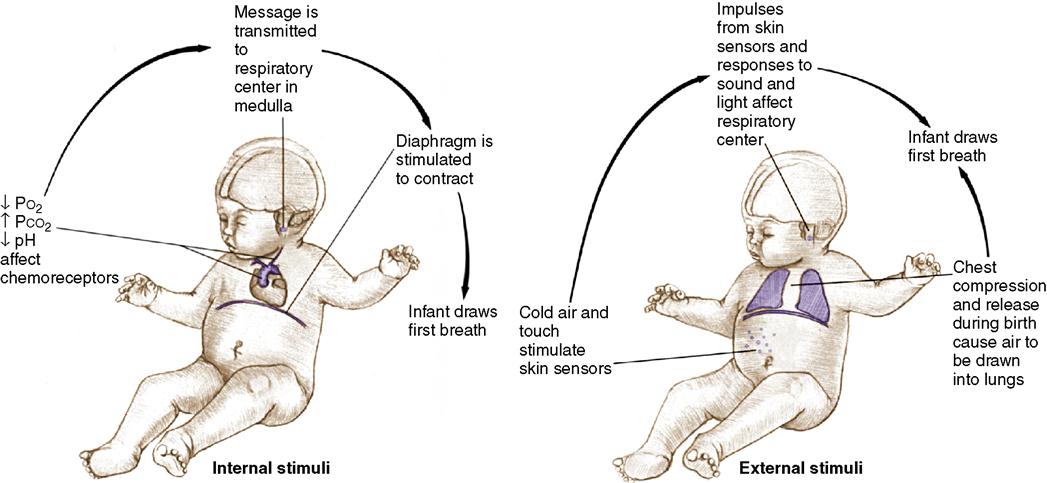
For the neonate’s life to be maintained outside of the uterus, the lungs must function immediately after birth. Pulmonary ventilation must be quickly established through lung expansion. The first breath of the healthy term infant occurs within seconds after birth; by 30 seconds, the neonate usually is breathing quite well on his or her own. Many powerful stimuli send messages to the respiratory center of the neonate’s brain (Figure 9-1). These stimuli can be divided into four categories: sensory, chemical, thermal, and mechanical.
The sensory stimuli that help respirations begin as the neonate emerges from the dark warmth of the uterus to the external environment are cold, touch, movement, light, and sound. Skin sensors are stimulated by tactile drying, wrapping the neonate in warm blankets, and skin-to-skin contact. Clamping the umbilical cord is a powerful chemical stimulus. The newborn experiences a temporary hypoxia when the placental blood flow is stopped due to the clamping of the cord. A decreased blood oxygen level (Po2) and an increased blood carbon dioxide level (Pco2), along with a decreased pH, occur. Acidosis results, which activates the respiratory center in the medulla of the brain to initiate respirations.
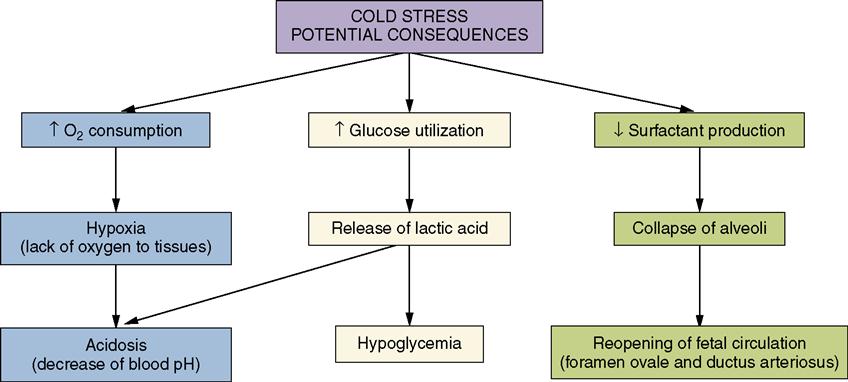
At birth, the newborn must make an adjustment from a warm environment (in utero) to a much cooler one. This temperature change is a major thermal stimulus to respirations. Excessive cooling (cold stress), however, will increase the need for oxygen and can produce acidosis. A lack of oxygen (hypoxia) at the tissue level will depress respirations rather than stimulate them. Because of this, it is very important to keep the infant warm.
The important mechanical stimuli are chest compression and recoil, which cause air to be drawn into and out of the lungs. The chest is compressed as it passes through the birth canal and recoils or expands as it leaves the mother’s body.
Changing from Fluid-Filled to Air-Filled Lungs
During a normal vaginal birth, the infant’s head is delivered first, then the chest. The chest area, made up of cartilage and bones, is squeezed or compressed, promoting drainage of fluid from the lungs. Before the chest is delivered, almost half of the fluid is forced out. As the chest returns (recoils) to its natural position, the infant sucks in air (20 to 40 mL) to replace the fluid forced out without having to make any effort of his or her own. The lung expansion creates the negative intrapleural pressure that is maintained throughout life.
The infant who is delivered by cesarean birth does not experience chest compression followed by chest recoil and thus is at greater risk for respiratory distress. However, there are other mechanisms by which the lungs are cleared besides this “vaginal squeeze.” Some of the fluid is absorbed by the lymphatic vessels, and the rest of the fluid is removed by the pulmonary capillaries. If the fluid is not removed, the infant will experience labored breathing or respiratory distress.
With the first breath, functional residual capacity (FRC) is established. This means a small amount of air is left in the alveoli of the lungs, which allows them to stay partially open during expiration. Surfactant promotes lung expansion and the ability of the alveoli to fill with air. With the establishment of FRC, the second, third, and subsequent breaths do not require as much pressure; with each breath, respiration becomes easier.
The normal newborn respiratory rate is 30 to 60 breaths/minute. The normal newborn’s breathing pattern includes 5- to 15-second pauses, called periodic breathing, and is normal. Cessation of breathing for more than 20 seconds is called apnea and is abnormal. The newborn breathes through the nose, and any nasal obstruction can cause respiratory distress because the newborn will not typically breathe through the mouth.
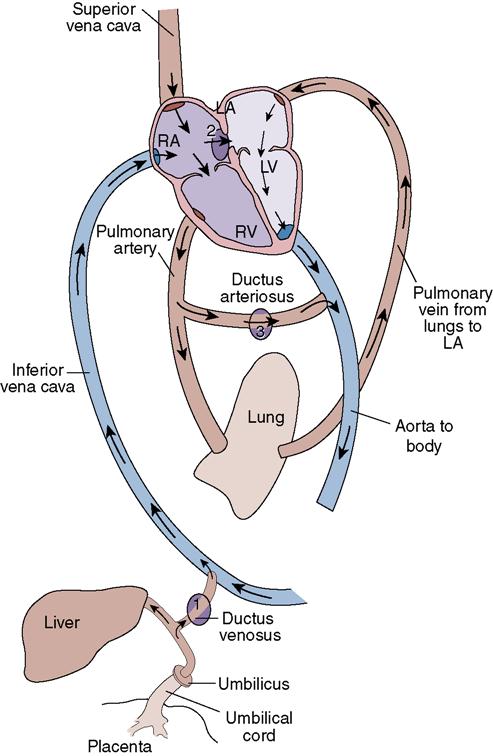
Closing Down the Fetal Structures (Shunts)
During fetal life, most of the blood flow bypasses the nonfunctional lungs and liver. A small percentage of blood goes to the lungs to perfuse the tissues. After birth, the neonate’s blood must begin to circulate to the lungs for oxygenation and to the liver for filtration. In other words, the three fetal shunts—the ductus arteriosus, foramen ovale, and ductus venosus—must close. These closures occur in response to shifts in pressures in the heart, an increase in blood oxygenation level, and cord clamping (Figure 9-2).
Foramen Ovale
The foramen ovale is an opening (a flap in the septum) between the right and left atria of the heart, with blood flow and pressure being greater in the right atrium. It functions like a one-way valve for blood flow, from the right to the left, and shunts blood away from the lungs to the aorta. Clamping the umbilical cord causes a large stream of blood from the placenta to be cut off. As a result, the pressure on the left side of the neonate’s heart becomes greater than that on the right side, placing pressure against the atrial septum, closing the flap of the foramen ovale. The foramen ovale functionally closes approximately 1 minute after birth, complete anatomic closure takes place approximately 2 hours after birth, and by 3 months the atrial septum is permanently fused together.
Ductus Arteriosus
The ductus arteriosus shunts blood from the pulmonary artery to the aorta, bypassing the lungs during fetal life. The pulmonary arterioles dilate in response to the increased aeration of the lungs at birth and the oxygen saturation of the blood increases, causing the ductus arteriosus to constrict and completely close at birth. The functional closure of the ductus arteriosus occurs approximately 15 to 24 hours after birth. The anatomic closure (fibrosis of ductus) occurs approximately 3 to 4 weeks after birth.
It is important to note that the ductus arteriosus can dilate (reopen) during the first several weeks after birth. If the neonate has a decrease in blood pressure and oxygen saturation, there may be a return to fetal-type circulation, with a reopening of the ductus arteriosus. This is referred to as patent ductus arteriosus and can lead to right-sided heart failure and pulmonary congestion. If the ductus arteriosus does reopen, unoxygenated blood will bypass the lungs and go through the pulmonary artery into the aorta and general circulation, and the newborn can become hypoxic and die.
Ductus Venosus
The ductus venosus is a fetal structure (shunt) that allows most oxygenated blood to bypass the liver and enter the inferior vena cava. Clamping the umbilical cord at birth cuts off the umbilical venous blood flow, causing a redistribution of blood, greatly reducing the flow of blood through the ductus venosus. The ductus venosus constricts at birth, closes anatomically approximately 1-2 weeks after birth, and eventually becomes a ligament. The closure of this bypass forces blood perfusion in the liver. The mechanisms for this closure are unknown.
It is important that the health care provider understand the basic mechanisms behind the closure of the fetal structures or shunts. Understanding the pressure changes within the heart and changes in the blood flow pattern will help the health care provider recognize problems or defects and determine appropriate management.
Body System Adaptations and Functions
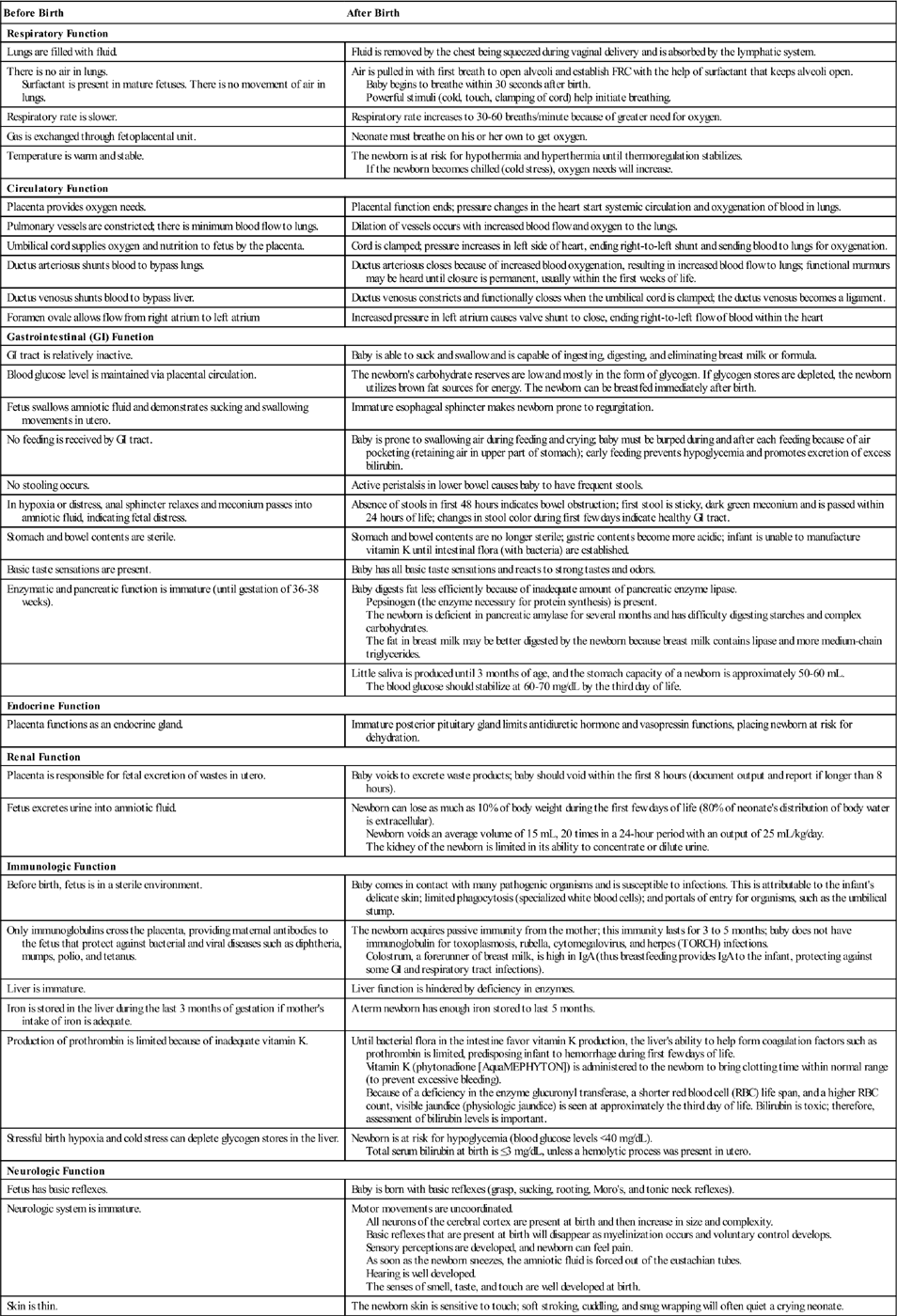
Although significant events occur in the body systems before birth, the body systems of the newborn are required to adapt and function differently after birth. The major adaptations are explored in Table 9-1.
Table 9-1
Characteristics of Body Systems Before and After Birth
| Before Birth | After Birth |
| Respiratory Function | |
| Lungs are filled with fluid. | Fluid is removed by the chest being squeezed during vaginal delivery and is absorbed by the lymphatic system. |
| There is no air in lungs. Surfactant is present in mature fetuses. There is no movement of air in lungs. | Air is pulled in with first breath to open alveoli and establish FRC with the help of surfactant that keeps alveoli open. Baby begins to breathe within 30 seconds after birth. Powerful stimuli (cold, touch, clamping of cord) help initiate breathing. |
| Respiratory rate is slower. | Respiratory rate increases to 30-60 breaths/minute because of greater need for oxygen. |
| Gas is exchanged through fetoplacental unit. | Neonate must breathe on his or her own to get oxygen. |
| Temperature is warm and stable. | The newborn is at risk for hypothermia and hyperthermia until thermoregulation stabilizes. If the newborn becomes chilled (cold stress), oxygen needs will increase. |
| Circulatory Function | |
| Placenta provides oxygen needs. | Placental function ends; pressure changes in the heart start systemic circulation and oxygenation of blood in lungs. |
| Pulmonary vessels are constricted; there is minimum blood flow to lungs. | Dilation of vessels occurs with increased blood flow and oxygen to the lungs. |
| Umbilical cord supplies oxygen and nutrition to fetus by the placenta. | Cord is clamped; pressure increases in left side of heart, ending right-to-left shunt and sending blood to lungs for oxygenation. |
| Ductus arteriosus shunts blood to bypass lungs. | Ductus arteriosus closes because of increased blood oxygenation, resulting in increased blood flow to lungs; functional murmurs may be heard until closure is permanent, usually within the first weeks of life. |
| Ductus venosus shunts blood to bypass liver. | Ductus venosus constricts and functionally closes when the umbilical cord is clamped; the ductus venosus becomes a ligament. |
| Foramen ovale allows flow from right atrium to left atrium | Increased pressure in left atrium causes valve shunt to close, ending right-to-left flow of blood within the heart |
| Gastrointestinal (GI) Function | |
| GI tract is relatively inactive. | Baby is able to suck and swallow and is capable of ingesting, digesting, and eliminating breast milk or formula. |
| Blood glucose level is maintained via placental circulation. | The newborn’s carbohydrate reserves are low and mostly in the form of glycogen. If glycogen stores are depleted, the newborn utilizes brown fat sources for energy. The newborn can be breastfed immediately after birth. |
| Fetus swallows amniotic fluid and demonstrates sucking and swallowing movements in utero. | Immature esophageal sphincter makes newborn prone to regurgitation. |
| No feeding is received by GI tract. | Baby is prone to swallowing air during feeding and crying; baby must be burped during and after each feeding because of air pocketing (retaining air in upper part of stomach); early feeding prevents hypoglycemia and promotes excretion of excess bilirubin. |
| No stooling occurs. | Active peristalsis in lower bowel causes baby to have frequent stools. |
| In hypoxia or distress, anal sphincter relaxes and meconium passes into amniotic fluid, indicating fetal distress. | Absence of stools in first 48 hours indicates bowel obstruction; first stool is sticky, dark green meconium and is passed within 24 hours of life; changes in stool color during first few days indicate healthy GI tract. |
| Stomach and bowel contents are sterile. | Stomach and bowel contents are no longer sterile; gastric contents become more acidic; infant is unable to manufacture vitamin K until intestinal flora (with bacteria) are established. |
| Basic taste sensations are present. | Baby has all basic taste sensations and reacts to strong tastes and odors. |
| Enzymatic and pancreatic function is immature (until gestation of 36-38 weeks). | Baby digests fat less efficiently because of inadequate amount of pancreatic enzyme lipase. Pepsinogen (the enzyme necessary for protein synthesis) is present. The newborn is deficient in pancreatic amylase for several months and has difficulty digesting starches and complex carbohydrates. The fat in breast milk may be better digested by the newborn because breast milk contains lipase and more medium-chain triglycerides. |
| Little saliva is produced until 3 months of age, and the stomach capacity of a newborn is approximately 50-60 mL. The blood glucose should stabilize at 60-70 mg/dL by the third day of life. | |
| Endocrine Function | |
| Placenta functions as an endocrine gland. | Immature posterior pituitary gland limits antidiuretic hormone and vasopressin functions, placing newborn at risk for dehydration. |
| Renal Function | |
| Placenta is responsible for fetal excretion of wastes in utero. | Baby voids to excrete waste products; baby should void within the first 8 hours (document output and report if longer than 8 hours). |
| Fetus excretes urine into amniotic fluid. | Newborn can lose as much as 10% of body weight during the first few days of life (80% of neonate’s distribution of body water is extracellular). Newborn voids an average volume of 15 mL, 20 times in a 24-hour period with an output of 25 mL/kg/day. The kidney of the newborn is limited in its ability to concentrate or dilute urine. |
| Immunologic Function | |
| Before birth, fetus is in a sterile environment. | Baby comes in contact with many pathogenic organisms and is susceptible to infections. This is attributable to the infant’s delicate skin; limited phagocytosis (specialized white blood cells); and portals of entry for organisms, such as the umbilical stump. |
| Only immunoglobulins cross the placenta, providing maternal antibodies to the fetus that protect against bacterial and viral diseases such as diphtheria, mumps, polio, and tetanus. | The newborn acquires passive immunity from the mother; this immunity lasts for 3 to 5 months; baby does not have immunoglobulin for toxoplasmosis, rubella, cytomegalovirus, and herpes (TORCH) infections. Colostrum, a forerunner of breast milk, is high in IgA (thus breastfeeding provides IgA to the infant, protecting against some GI and respiratory tract infections). |
| Liver is immature. | Liver function is hindered by deficiency in enzymes. |
| Iron is stored in the liver during the last 3 months of gestation if mother’s intake of iron is adequate. | A term newborn has enough iron stored to last 5 months. |
| Production of prothrombin is limited because of inadequate vitamin K. | Until bacterial flora in the intestine favor vitamin K production, the liver’s ability to help form coagulation factors such as prothrombin is limited, predisposing infant to hemorrhage during first few days of life. Vitamin K (phytonadione [AquaMEPHYTON]) is administered to the newborn to bring clotting time within normal range (to prevent excessive bleeding). Because of a deficiency in the enzyme glucuronyl transferase, a shorter red blood cell (RBC) life span, and a higher RBC count, visible jaundice (physiologic jaundice) is seen at approximately the third day of life. Bilirubin is toxic; therefore, assessment of bilirubin levels is important. |
| Stressful birth hypoxia and cold stress can deplete glycogen stores in the liver. | Newborn is at risk for hypoglycemia (blood glucose levels <40 mg/dL). Total serum bilirubin at birth is ≤3 mg/dL, unless a hemolytic process was present in utero. |
| Neurologic Function | |
| Fetus has basic reflexes. | Baby is born with basic reflexes (grasp, sucking, rooting, Moro’s, and tonic neck reflexes). |
| Neurologic system is immature. | Motor movements are uncoordinated. All neurons of the cerebral cortex are present at birth and then increase in size and complexity. Basic reflexes that are present at birth will disappear as myelinization occurs and voluntary control develops. Sensory perceptions are developed, and newborn can feel pain. As soon as the newborn sneezes, the amniotic fluid is forced out of the eustachian tubes. Hearing is well developed. The senses of smell, taste, and touch are well developed at birth. |
| Skin is thin. | The newborn skin is sensitive to touch; soft stroking, cuddling, and snug wrapping will often quiet a crying neonate. |
Thermoregulation
Thermoregulation, the ability to produce heat and maintain a normal body temperature, is a vital metabolic function and a continuous challenge for the newborn. Nursing responsibilities related to thermoregulation immediately after birth are discussed in Chapter 7. Cold stress effects are reviewed in Figure 9-3.
Temperature regulation of the newborn is maintained by balancing the amount of heat produced with the amount of heat lost. If the amount of heat lost exceeds the amount of heat produced, the body temperature will fall.
The flexed position of the extremities in a term newborn minimizes the exposure of skin surface to the air, but if the infant has poor muscle tone and the arms and legs do not remain flexed (as seen in the preterm infant), more body surface area is exposed to the air, and the risk of cold stress increases. A major responsibility in newborn care is maintaining a neutral thermal environment that prevents heat loss and cold stress. A neutral thermal environment makes minimum demands on the newborn’s energy reserves, allowing a basal metabolic rate (BMR) with minimum oxygen consumption needs. Maintaining an abdominal skin temperature of 36.5° C (97.7° F) will minimize oxygen consumption needs and conserve energy. A neutral thermal environment is maintenance of 32° C to 34° C (89.6° F to 93.2° F) for an unclothed term newborn (London, Ladewig, Ball, & Bindler, 2006). A neutral thermal environment in the nursery may be 25° C (77° F) for a newborn who is warmly wrapped in an open bassinet (Blackburn, 2007). If a neutral thermal environment is not maintained, the newborn will respond by increasing the BMR, and oxygen consumption needs will increase, resulting in cold stress, depletion of glycogen stores, and resulting acidosis. Kangaroo care (skin-to-skin contact) is the best means of thermal support (see Chapters 10 and 15). Because of this, nonvital procedures such as bathing should not be done until the newborn’s body temperature and respirations have been stabilized.
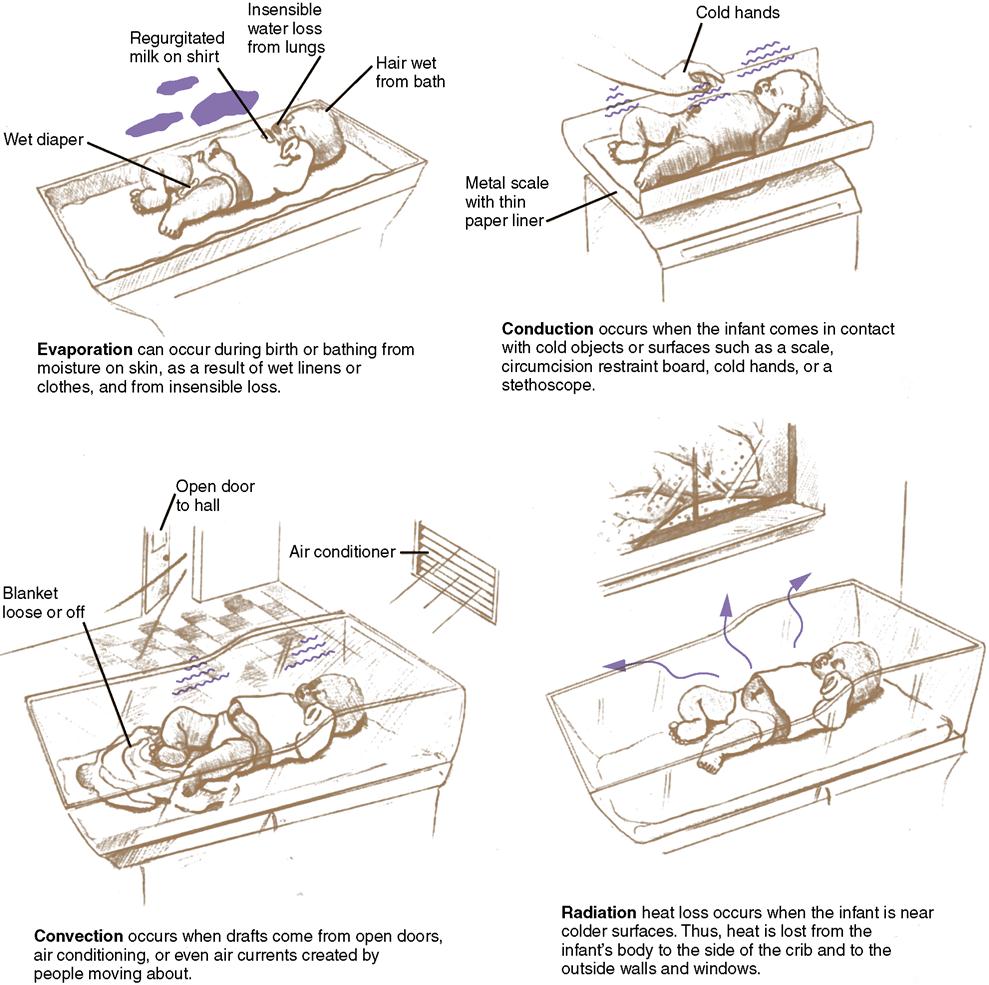
Factors Contributing to Heat Loss
Newborns are prone to heat loss because they have a large body surface area in relation to their weight. Their skin is thin, blood vessels are close to the surface, and there is little subcutaneous fat for insulation. Because of these factors, newborns have a greater transfer of heat to the external environment than do adults. In addition, at birth the newborn’s skin is wet with amniotic fluid, and the room temperature is cooler than the intrauterine environment.
Heat Loss to Environment
Heat loss to the environment takes place in four ways: evaporation, conduction, convection, and radiation (Figure 9-4, Table 9-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree