Patient Education
Learning Objectives
1. Apply critical thinking skills in performing the patient assessment and patient care.
2. Recognize the implications of health and illness models for patient education.
3. Instruct patients according to their needs to promote health maintenance and disease prevention.
4. Define six patient factors that have an impact on learning.
5. List at least five guidelines for patient education that can affect the patient’s overall wellness.
6. Demonstrate empathy in communicating with patients, family members, and staff.
7. Display respect for individual diversity.
8. Summarize educational approaches for patients with language barriers.
9. Determine potential barriers to patient learning.
10. Develop and maintain a current list of community resources related to patients’ healthcare needs.
11. Implement a variety of teaching methods and strategies responsive to the individual patient’s needs.
12. Demonstrate the ability to develop an appropriate and effective patient teaching plan.
13. Demonstrate recognition of the patient’s level of understanding in communications.
14. Document patient education.
15. Describe the role of the medical assistant in patient education.
16. Integrate the legal and ethical elements of patient teaching into the ambulatory care setting.
Scenario
Taylor DiSalvo is a medical assistant in a busy family practice office. He currently is working with one of the patients, Sam Ignatio, who is 62 years old and has been married for 30 years. Mr. Ignatio has just been diagnosed with type 2 diabetes mellitus. Mr. Ignatio knows nothing about his disease or how to manage it; he has never seen a glucometer and never handled needles. In addition, his diet is high in fats and carbohydrates, and he does not exercise regularly. Mr. Ignatio is 50 pounds overweight, has functional deafness in his left ear and decreased sound quality in his right ear, and shows early signs of diabetic-related vision loss. Taylor is responsible for assisting with Mr. Ignatio’s patient teaching plan.
Mr. Ignatio is faced with a serious illness, and his future health depends on compliance with a wide range of lifestyle changes. The methods Taylor chooses to teach this patient about his disease can have a significant impact on his eventual health outcome.
While studying this chapter, think about the following questions:
This chapter focuses on helping students recognize the individual learning needs of patients, and it also provides guidelines for developing effective teaching approaches. The key to patient compliance with prescribed treatments is empowerment; that is, providing the patient with information and support that enable the person to take charge of his or her health problem. The concepts in this chapter are basic to all patient education interventions, and a medical assistant who follows them can positively affect a patient’s understanding of the disease process and the person’s willingness to comply with the disease management steps recommended by the physician.
Patient Education and Models of Health and Illness
Patient education should begin with the first contact between the patient and the healthcare team. A well-informed patient is more likely to comply with treatment and adopt a healthy lifestyle. However, informing a patient about his or her disease is only part of the health teaching process. The key to successful health teaching is to empower the patient to accept the responsibility of his or her disease process and to become willing to implement teaching guidelines.
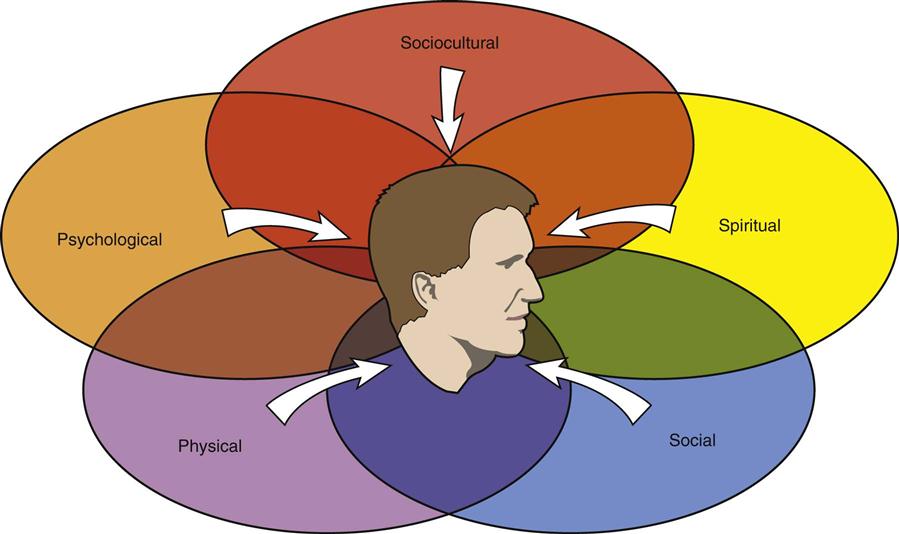
As a result of reductions in hospital admissions and shorter hospital stays, patients and families have had to assume responsibility for care that once was provided by the hospital staff. This means that those who work in ambulatory care settings have an even greater responsibility to meet the educational needs of their patients. To develop an effective teaching approach, we must implement a holistic model that considers not only the patient’s physical state, but also his or her psychological, social, and spiritual needs (Figure 29-1). The holistic model suggests that we look at patients and determine their needs based on a complete view of their lives rather than just as an analysis of their specific diseases. It is our responsibility not only to teach patients about disease processes, but also to help them implement related skills and changes in lifestyle to promote recovery and improve function. In the case of Mr. Ignatio, diabetes mellitus is a complicated disease that requires an in-depth understanding of the disease process and significant lifestyle changes. When considering the impact of this diagnosis on the patient (in this case, Mr. Ignatio), the medical assistant should keep in mind the following factors, because they will affect the patient’s response.
The health belief model may help the medical assistant understand why some people do not follow recommended guidelines to maintain their health and prevent the development of disease.
This model focuses on individuals’ attitudes toward and beliefs about themselves and their health. The model suggests that we first consider how the patient perceives his or her risk of developing a disease and the potential severity of the condition. For example, even though Mr. Ignatio’s mother and sister developed type 2 diabetes in their sixties, he may believe he is not going to have the same problem. Therefore, even though wellness information encouraged him to lose weight, exercise, and eat a healthy diet, he didn’t believe he was in danger of developing diabetes, so he didn’t believe he needed to follow these disease prevention recommendations. He may also believe that even if he does develop diabetes, the consequences of the disease are not that serious, so why bother altering his lifestyle to prevent it?
Another factor considered in the health belief model is the patient’s perceived benefits of action; that is, whether the patient believes altering health behaviors will prevent him from developing the disease. In this case, because Mr. Ignatio has a strong family history of the disease, he may have decided he was going to get diabetes anyway, so why should he bother exercising and watching his diet? He may have believed he was going to develop diabetes no matter what he did, so why bother trying to prevent it? Until the patient believes that teaching and health promotion guidelines affect him and are worth pursuing, he will not follow suggested health promotion tips or comply with treatment protocols.
Table 29-1 outlines the health belief model and presents suggested methods for applying the model in patient teaching efforts in the ambulatory care setting.
TABLE 29-1
| PRINCIPLES | DEFINITION | PATIENT EDUCATION USE |
| Perceived susceptibility | Patient’s opinion on the chances of getting a disorder. | Supply information on the risk level; individual risk is based on health habits and family history. |
| Perceived severity | Patient’s opinion on the seriousness of the condition and its health risks. | Outline the potential complications of the disease. |
| Perceived benefits | Patient’s belief in the value of altering lifestyle factors and complying with treatment. | Emphasize the positive results that can occur if the patient complies with healthcare recommendations. |
| Perceived barriers | Patient’s opinion on the financial and psychological costs of compliance. | Identify patient barriers and work to reduce them through patient education, family outreach, and use of community resources. |
| Cues to action | Methods developed to activate patient compliance. | One-on-one education interventions; detailed handouts; family involvement in education efforts; follow-up at subsequent office visits; referral to community resources. |
| Self-efficacy | Patient has the confidence to take action to achieve a healthier state. | Ongoing education and support. |
The five stages of grief, as defined by Dr. Elisabeth Kübler-Ross, are another model that may be helpful for understanding the way patients respond to health threats. When a patient faces a serious health threat, the grief process may delay the patient in adjusting to the disease and starting to take control of his or her health. For example, Mr. Ignatio may respond to the news of his diagnosis with what is commonly the first stage of the grief process—denial. Perhaps both his mother and sister suffered serious complications from diabetes, including blindness and leg amputation, and he may be using denial to deal psychologically with the burden of the diagnosis. Each individual goes through the stages of grief in his or her own way and at his or her own pace. This process can take weeks to months; however, until the patient reaches the point of accepting the diagnosis and the possible ramifications of the disease, compliance with patient education will be very difficult to achieve.
Patient Factors that Affect Learning
Many factors or characteristics may affect the patient’s ability to learn. Medical assistants must be aware of these factors to develop a patient education approach that best meets the needs of each patient.
Perception of Disease Versus Actual State of Disease
Patients respond to a particular diagnosis in many different ways. One predictor of how a patient will respond, and therefore how he or she will react to health education, is the patient’s perception of the disease. Previous life experiences may greatly influence the patient’s knowledge base and/or desire to learn about the disease. Does the patient recognize and accept the seriousness of the diagnosis? Or, perhaps, does the patient overreact to potential disease risks? Both of these responses affect the patient’s willingness to learn about the disease and his or her compliance with treatment recommendations.
How do you think Taylor’s patient education efforts will be affected if Mr. Ignatio does not consider diabetes a serious disease?
Patient’s Need for Information
The patient’s perception of the impact of the disease on his or her general health also determines the need for information about the disease. Does the patient express a desire to learn all he or she can about the disease, or does the patient resist or act indifferent to teaching efforts? A vital part of patient education is encouraging patient ownership of the learning process. To accomplish this, you first may have to persuade the patient that he or she needs to understand the disease before an improvement in overall wellness can be achieved.
Mr. Ignatio tells Taylor that his father was a diabetic and had to have both legs amputated because of the disease. Mr. Ignatio says that it doesn’t matter whether he controls his blood sugar; he will still have major health complications. What is the appropriate response?
Patient’s Age and Developmental Level
Depending on the patient’s age and ability to understand information about the disease, you may have to adapt the teaching plan to meet specific learning needs. For example, educating a 9-year-old patient with type 1 diabetes about disease management requires a different approach from the one used for Mr. Ignatio. The medical assistant should be flexible and creative in providing learning opportunities that support the physician’s attempt to educate the patient about disease prevention and health maintenance. Often the key to patient understanding and compliance is the involvement of family members.
During his assessment of Mr. Ignatio’s diet, Taylor learns that his wife cooks all his meals and packs his lunch daily. What should Taylor do to make sure Mr. Ignatio’s diet complies with diabetic recommendations?
Patient’s Mental and Emotional State
Even a well-planned teaching intervention can be ineffective if the patient is unable to pay attention because of anxiety, stress, anger, or denial (Figure 29-2). Frequently patients use defense mechanisms to protect themselves from the reality of a serious illness. It is important that the medical assistant be sensitive to the patient’s mental state and adapt teaching interventions as needed.
Mr. Ignatio has just been told about his disease. He already shared that his father died of diabetes. Do you think he is able to pay attention to patient teaching about how to give his insulin injections? What should Taylor do to manage this problem?
Influence of Multicultural and Diversity Factors on Patient Education
Culture, family background, and religious beliefs influence patients’ actions. Working with patients from diverse backgrounds is an exciting challenge; however, for patient education to be successful, it is essential that the medical assistant be aware of and sensitive to the impact of these factors on patient learning (Figure 29-3). Some questions you should consider when teaching a patient from another background include:
• Is language an issue with your patient (Figure 29-4)? If the patient is unable to understand spoken English or to read it correctly, do you have an alternative method for getting the information across?
• What strategies or techniques might minimize patient education problems?
• Are community resources available that could facilitate patient learning?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree