Assisting in Obstetrics and Gynecology
Learning Objectives
1. Define, spell, and pronounce the terms listed in the vocabulary.
2. Apply critical thinking skills in performing the patient assessment and patient care.
3. Explain the anatomy and physiology of the female reproductive system.
4. Trace the ovum through the three phases of menstruation.
5. Compare current contraceptive methods.
6. Summarize menstrual disorders and conditions.
7. Distinguish among different types of gynecologic infections.
8. Differentiate between benign and malignant neoplasms of the female reproductive system.
9. Prepare for and assist with the female examination, including obtaining a Papanicolaou (Pap) smear.
10. Demonstrate patient preparation for a cryosurgery procedure.
11. Teach the patient the technique for a breast self-examination.
12. Compare the positional disorders of the pelvic region.
13. Summarize the process of pregnancy and parturition.
14. Describe the common complications of pregnancy.
15. Specify the signs, symptoms, and treatments of conditions related to menopause.
16. Outline the medical assistant’s role in gynecologic and reproductive examinations.
17. Demonstrate how to assist with a prenatal examination.
18. Distinguish among diagnostic tests that may be done to evaluate the female reproductive system.
19. Summarize patient education guidelines for obstetric patients.
20. Discuss the legal and ethical implications in a gynecology practice.
Vocabulary
adnexal (add-neks-uhl) Pertaining to adjacent or accessory parts.
Bartholin’s cyst A fluid-filled cyst in one of the vestibular glands that are located on either side of the vaginal orifice.
clitoris (kli′-tuh-ris) A small, elongated erectile body above the urinary meatus at the superior point of the labia minora.
coitus Sexual union between male and female; also called intercourse.
colostrum (koh-lahs′-trum) A thin, yellow, milky fluid secreted by the mammary glands a few days before and after delivery.
dilation The opening of the cervix through the process of labor, measured as 0 to 10 cm dilated.
dilation and curettage (D&C) The widening of the cervix and scraping of the endometrial wall of the uterus.
dysplasia An alteration in cell growth, causing differences in size, shape, and appearance.
effacement The thinning of the cervix during labor, measured in percentages from 0% to 100% effaced.
endocervical curettage The scraping of cells from the wall of the uterus.
human chorionic gonadotropin (HCG) A hormone secreted by the placenta that is found in the urine of pregnant females.
lymphedema (limf-uh-de′-muh) Swelling caused by the accumulation of lymph fluid in soft tissues.
mons pubis The fat pad that covers the symphysis pubis.
multiparous Pertaining to women who have had two or more pregnancies.
myelomeningocele A herniation of a portion of the spinal cord and its meninges that protrudes through a congenital opening in the vertebral column.
nonstress tests (NSTs) Fetal monitoring used in combination with maternal reports of fetal movement to evaluate the fetal heart rate response.
parturition (par-too-rih′-shun) The act or process of giving birth to a child.
stereotactic Pertaining to an x-ray procedure used to guide the insertion of a needle into a specific area of the breast.
vulva The external female genitalia, which begins at the mons pubis and terminates at the anus.
Scenario
Betsy Davis, CMA (AAMA), recently was hired by the University Women’s Hospital to work for Dr. Erin Beck, an obstetrician/gynecologist for a busy family-centered healthcare facility in her community. Betsy has worked for a family practice physician for 3 years, but this is her first position in a specialty practice. Betsy is excited about the opportunity to focus on women’s health issues and is especially interested in helping in the obstetric area of the practice. Betsy’s responsibilities will include understanding current methods of contraception and the patient education factors that are important for each. She also needs to develop expertise in gynecologic diseases and conditions, including diagnostic and treatment protocols for cancers of the female system. Medical assistants in the practice are expected to be able to teach breast self-examination and to answer the questions of pregnant patients concerning a healthy pregnancy, labor, and delivery.
While studying this chapter, think about the following questions:
• What is the basic anatomy and physiology of the female system?
• What does Betsy need to learn about contraceptives to be able to answer patients’ questions?
• Betsy needs to become familiar with which gynecologic disorders?
• What are the primary malignancies of the female system?
• How should Betsy assist Dr. Beck with a Pap smear?
• How can Betsy teach patients to perform a breast self-examination?
• What are the stages of pregnancy and birth?
• How can Betsy help patients understand issues that can arise with menopause?
• What are the typical diagnostic procedures used in obstetrics and gynecology?
The branch of medicine that deals with pregnancy, labor, and the postnatal period is known as obstetrics, and the branch of medicine that deals with diseases of the genital tract in women is called gynecology. Frequently, a physician practices both specialties and is known as an OB/GYN physician. Assessment of the female reproductive system is an important part of healthcare. Patients often are hesitant and uncomfortable about talking about sexual matters, so they wait until symptoms are intolerable or disease is advanced before seeking medical care. In addition to the signs and symptoms of disease, the medical assistant must be aware of the patient’s emotional state and must give support when needed.
Anatomy and Physiology
Female Reproductive System
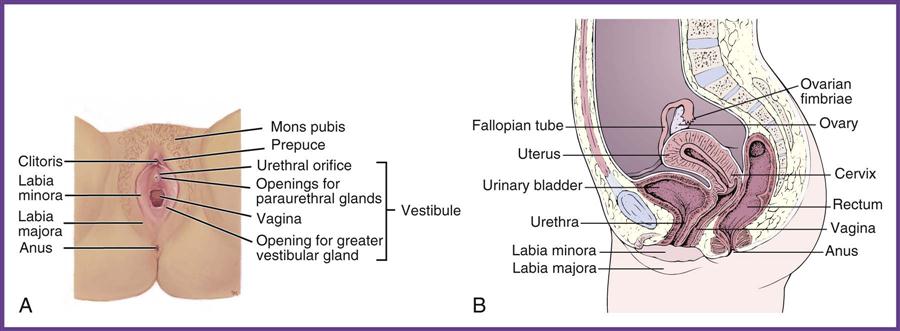
The female reproductive system includes both internal and external organs. The internal organs are located in the pelvis and cannot be seen without special instruments, such as a vaginal speculum or a laparoscope. The external organs can be seen during the physical examination.
The primary parts of the female reproductive system are the vulva, vagina, uterus, fallopian tubes, and ovaries (Figure 41-1). The vulva includes the clitoris, the urethral meatus, and the vaginal orifice. These structures are covered by two sets of lips of tissue. The inner set, the labia minora, is a thin layer of skin that extends from the top of the clitoris to the base of the vaginal opening. The external set, the labia majora, and the mons pubis are covered with hair in the adult.
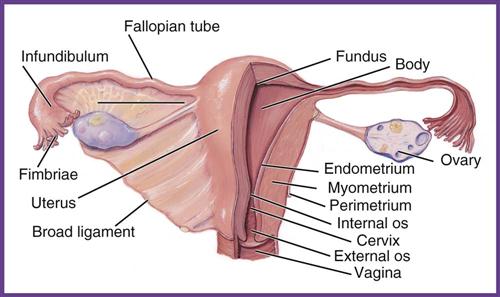
The vagina connects the internal and external organs. This tubelike structure is constructed to receive the penis during coitus. It is lubricated by a mucous membrane lining, and its walls are made up of overlapping tissue in the form of rugae, which allows the vagina to expand during the birth of an infant. At the distal end of the vagina is the cervix, often called the neck of the uterus, which is approximately 1 to 1½ inches long. The uterus is an upside-down, pear-shaped muscular organ, and its sole purpose is to house and nourish the fetus from implantation shortly after conception until parturition. The uterine walls have three layers. The inner layer, the endometrium, is rich in blood and changes in consistency during the menstrual cycle. The middle layer, the myometrium, is the powerful muscular layer that contracts to make the birth of a baby possible. The outer layer, the perimetrium, protects the structure and attaches to ligaments that support and hold the uterus in place (Figure 41-2).
On both sides of the fundus of the uterus are the fallopian tubes, also called the oviducts. These tubes extend from the uterus to the ovaries but do not attach to the ovaries. The distal end of the tube opens freely into the abdominopelvic cavity and acts as a passageway for the ovum to the uterus and for the sperm as they search for the ovum. At the distal end of the fallopian tubes are fingerlike projections, called fimbriae, which move in a wavelike pattern to draw the released ovum into the fallopian tube.
The ovaries are almond-shaped organs that produce and release the egg (ovum) and excrete the hormones necessary for the development of secondary sexual characteristics and the maintenance of a pregnancy. The ovaries secrete the hormones progesterone and estrogen, which regulate reproductive function. For pregnancy to occur, the vagina must receive the sperm from the male; the sperm move up through the opening in the cervix (the cervical os), through the uterus, and into the fallopian tubes. As many as 200 million to 600 million sperm can be deposited, and about 100,000 survive the acidic environment of the vagina to swim toward the egg.
Fertilization occurs when one sperm cell penetrates and fertilizes an egg. Fertilization usually takes place in the distal third of the fallopian tube. The tiny fertilized ovum, now called a zygote, moves by peristalsis and the massaging motion of the cilia that line the fallopian tube into the uterus and implants itself into the uterine wall. After implantation, the placenta forms; this structure supplies the new life with all the nourishment needed for development. Once pregnancy begins, the serum levels of human chorionic gonadotropin (HCG) rise, and the hormone spills into the woman’s urine, where it can be detected with a pregnancy test.
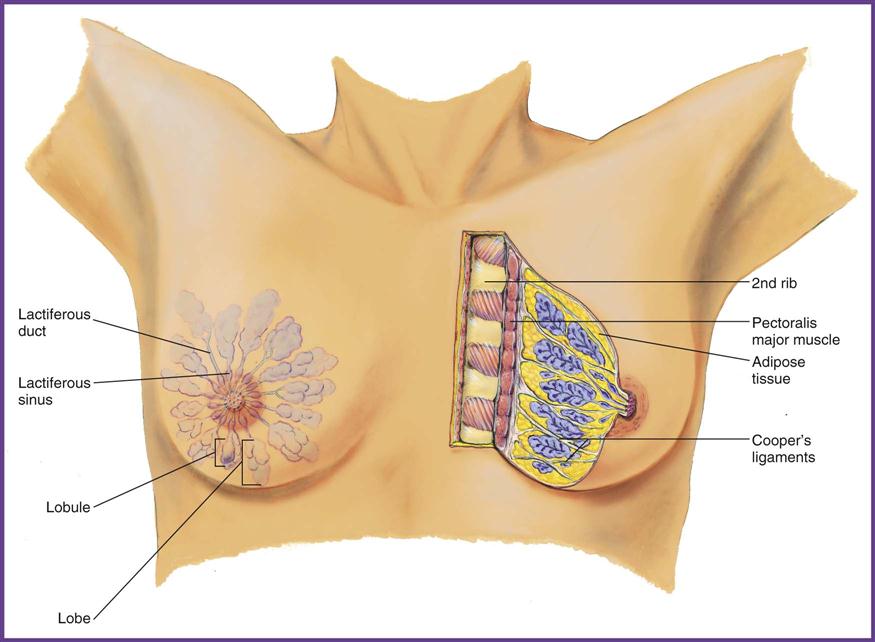
Breast Tissue
Mammary tissue develops from the increased estrogen secretion that occurs during puberty. In the center of each breast is a nipple surrounded by a pigmented region called the areola. Inside the breast are 15 to 20 lobes and their subunits—the lobules of glandular tissue that are separated by connective support tissue and surrounded by adipose tissue. The amount and distribution of adipose tissue determine the size and shape of the breast (Figure 41-3). Breast tissue also contains mammary glands, modified sweat glands that become the organs of milk production, and a system of ducts for delivery of milk to the nipple. Mammary ducts respond to elevated levels of estrogen and progesterone produced during the menstrual cycle by increasing in size, resulting in premenstrual fullness and tenderness of the breasts.
Four hormones control the mammary glands: Estrogen is responsible for the increase in size; progesterone stimulates the development of the duct system; prolactin stimulates the production of milk; and oxytocin causes the ejection of milk from the glands.
Menstruation
When a girl enters puberty, one of the many changes that occur is menarche, or the beginning of the menstrual cycle. Menstruation is a normal body process that occurs in every female. It is the physiologic means by which the body rids itself of the thickened endometrial wall that develops during the average 28-day cycle. The menstrual cycle involves a series of events controlled by hormones from the pituitary gland and the ovaries. The cycle is divided into three phases: the follicular phase, the luteal phase, and the menstrual phase.
Follicular Phase (Proliferative Phase)
The hypothalamus begins the follicular phase by secreting gonadotropin-releasing hormone (GnRH), stimulating the anterior pituitary to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones mature a graafian follicle in an ovary that contains an ovum. The ovarian follicle secretes estrogen, which stimulates the growth of the endometrium. It takes approximately 9 days (to day 14 of the menstrual cycle) for the graafian follicle to ripen and bulge out from the ovarian wall. The ovarian wall becomes thinner as the follicle enlarges until it bursts, allowing the ovum to be liberated into the abdominal cavity. Expulsion of the egg ends the follicular phase. The fallopian fimbriae begin their wavelike motion to fan the ovum into the fallopian tube. The rupture spot on the ovary, now called the corpus luteum, begins to secrete progesterone. Ovulation causes a rise in body temperature, and some women experience cramping and tenderness in the lower abdominal area at this time as a result of the rupture of the graafian follicle.
Luteal Phase (Secretory Phase)
Once ovulation is complete, the luteal phase begins (day 15). During this phase, progesterone secreted by the corpus luteum causes extensive growth of the endometrium as it prepares for a possible pregnancy. If conception occurs, the corpus luteum continues to secrete progesterone until the placenta is well established and can secrete progesterone and HCG to maintain the pregnancy. If conception does not occur, HCG is not secreted, and the corpus luteum atrophies. Without increased levels of progesterone and HCG, the endometrium breaks down, and menstruation begins.
Menstrual Phase
Menstruation begins on day 28. This discharge is made up of necrotic endometrial tissue, mucus, and the blood from the endometrial engorgement. As the uterus contracts to shed the excess tissue, a woman may experience cramping pain and irritability. This phase usually lasts approximately 5 days, and then the follicular phase begins again.
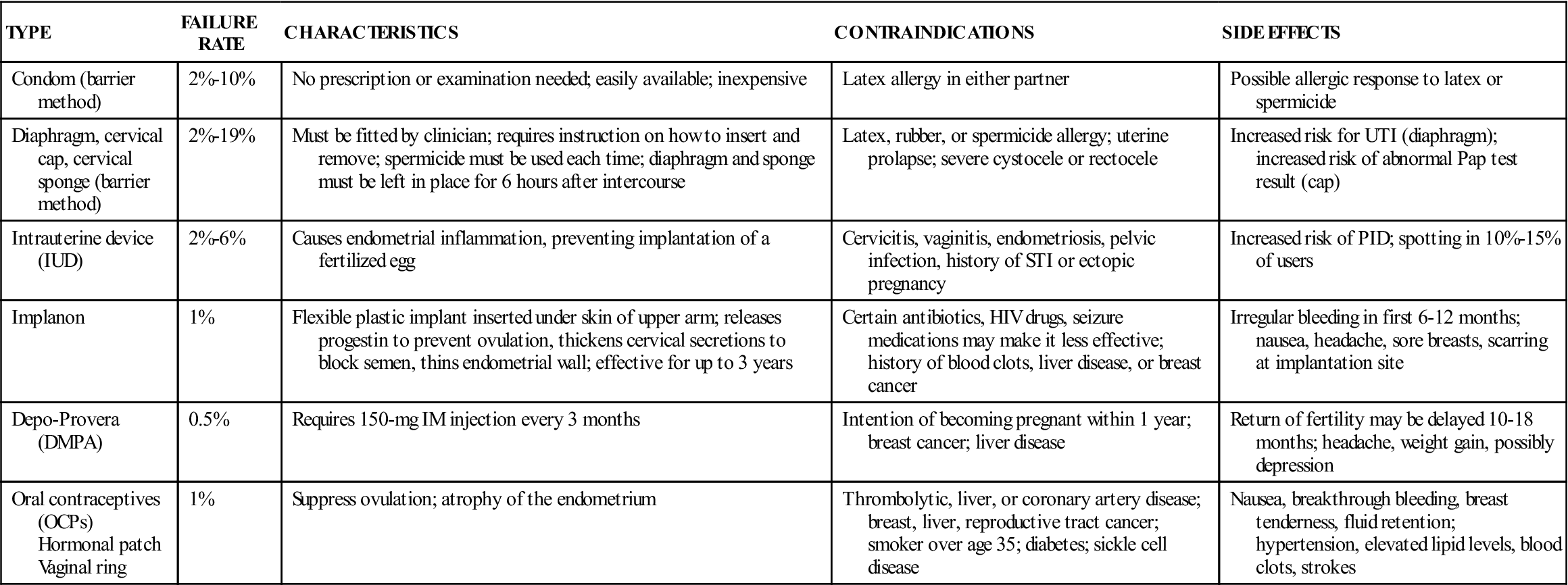
Contraception
A woman’s choice of a contraceptive method is based on many factors. To make an informed choice, a patient should know the risks, benefits, side effects, costs, failure rates, and convenience of each available method. In addition, although condoms are only moderately successful at preventing pregnancy, they should be used consistently to prevent transmission of sexually transmitted infections (STIs). The medical assistant may help provide patient education on contraceptive methods. Table 41-1 summarizes the characteristics of various contraceptive methods.
TABLE 41-1
Characteristics of Various Contraceptive Methods
| TYPE | FAILURE RATE | CHARACTERISTICS | CONTRAINDICATIONS | SIDE EFFECTS |
| Condom (barrier method) | 2%-10% | No prescription or examination needed; easily available; inexpensive | Latex allergy in either partner | Possible allergic response to latex or spermicide |
| Diaphragm, cervical cap, cervical sponge (barrier method) | 2%-19% | Must be fitted by clinician; requires instruction on how to insert and remove; spermicide must be used each time; diaphragm and sponge must be left in place for 6 hours after intercourse | Latex, rubber, or spermicide allergy; uterine prolapse; severe cystocele or rectocele | Increased risk for UTI (diaphragm); increased risk of abnormal Pap test result (cap) |
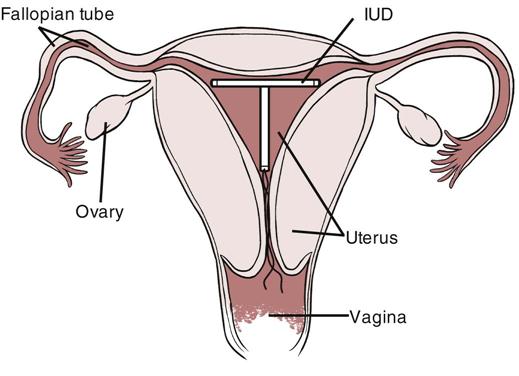
| Intrauterine device (IUD) | 2%-6% | Causes endometrial inflammation, preventing implantation of a fertilized egg | Cervicitis, vaginitis, endometriosis, pelvic infection, history of STI or ectopic pregnancy | Increased risk of PID; spotting in 10%-15% of users |
| Implanon | 1% | Flexible plastic implant inserted under skin of upper arm; releases progestin to prevent ovulation, thickens cervical secretions to block semen, thins endometrial wall; effective for up to 3 years | Certain antibiotics, HIV drugs, seizure medications may make it less effective; history of blood clots, liver disease, or breast cancer | Irregular bleeding in first 6-12 months; nausea, headache, sore breasts, scarring at implantation site |
| Depo-Provera (DMPA) | 0.5% | Requires 150-mg IM injection every 3 months | Intention of becoming pregnant within 1 year; breast cancer; liver disease | Return of fertility may be delayed 10-18 months; headache, weight gain, possibly depression |
| Oral contraceptives (OCPs) Hormonal patch Vaginal ring | 1% | Suppress ovulation; atrophy of the endometrium | Thrombolytic, liver, or coronary artery disease; breast, liver, reproductive tract cancer; smoker over age 35; diabetes; sickle cell disease | Nausea, breakthrough bleeding, breast tenderness, fluid retention; hypertension, elevated lipid levels, blood clots, strokes |
Barrier Methods
Barrier methods of contraception either kill sperm through the use of a chemical spermicide or prevent them from entering the cervical os. These methods, which are relatively inexpensive, include the condom, diaphragm, and cervical cap or sponge. Each method must be used every time the person has intercourse, which means the patient must be motivated to follow through on using it. Patient education on the use of a diaphragm includes the following instructions:
The cervical cap is a thimble-sized, domed barrier device that fits over the end of the cervix. It also is used with spermicidal jelly. It is 92% to 96% effective if used properly. An advantage of this barrier method is that the cap can be inserted up to 12 hours before intercourse and can stay in place up to 72 hours without affecting effectiveness or safety. The cervical sponge contains spermicide and also can be inserted hours before intercourse and is effective for 24 hours. The sponge is 80% to 91% effective if always used as directed.
Hormonal Contraceptives
Hormonal contraceptives are a highly effective and reversible form of contraception. They work by inhibiting ovulation, changing the cervical mucosa, affecting sperm mobility, and preventing thickening of the endometrial wall. Hormonal contraceptives include the birth control pill or patch, the vaginal ring, Depo-Provera injections, and the Implanon implant.
Besides being a highly effective method of birth control, oral contraceptives can be used to treat a wide range of gynecologic conditions, including menstrual irregularities, premenstrual syndrome (PMS) symptoms, and anovulation; they also can be used to prevent ovarian cysts and may be prescribed to increase bone density. However, to be effective, the pills must be taken daily. Failure rates are associated with noncompliance and can range from less than 1% in highly compliant women to greater than 15% in those who do not take the pills as prescribed. Oral contraceptive pills (OCPs) can have serious side effects, so patients should be informed of conditions that require immediate medical attention. These can be remembered with the mnemonic ACHES: abdominal pain (new and severe), chest pain (new and severe), headaches (new or more frequent), eye problems (blurred vision or vision loss), and severe leg pain. These symptoms may indicate the formation of a blood clot in the abdomen, chest, or leg, or they may be signs of a stroke; blood clot formation and stroke are the most serious complications of OCPs.
A type of oral contraception, Seasonale, limits the number of menstrual periods to four a year, although patients are more likely to have spotting and breakthrough bleeding with this hormone therapy than with the traditional 28-day birth control pill. Seasonale is designed to be taken once a day for 84 days, and then an inactive dose is taken for a week, during which the woman would menstruate. A recently released OCP, Yaz, may be prescribed for women suffering from a severe form of PMS called premenstrual dysphoric disorder (PMDD) and also is useful for treating acne in female patients at least 14 years of age who have started menstruating.
As mentioned, hormonal contraception also can be delivered via a transdermal patch, the Ortho Evra patch. The patch is a 1¾-inch square that slowly releases estrogen and progestin through the skin and into the bloodstream. It is considered as effective as oral contraceptives in women who weigh less than 198 pounds. Women who choose the patch as a birth control method are exposed to 60% more estrogen than those who take OCPs. For this reason, patch users may be at greater risk of side effects. The side effects of the patch are similar to those of birth control pills, but the risks for heart attack, stroke, and blood clots may be slightly greater. Cigarette smoking increases the risk of serious cardiovascular side effects, especially if the patient is over age 35. Patients should be told not to apply any creams or oils at the application site, to change the patch weekly for 3 consecutive weeks, and to go patch free the fourth week, allowing menstruation to occur. The patch can be applied to the buttocks, lower abdomen, and upper body but not to the breasts. The woman can bathe, shower, and swim while wearing the patch, but if it comes off, it should be replaced immediately.
The vaginal ring (NuvaRing) contraceptive device is made of flexible plastic and is inserted into the vagina. The ring slowly releases estrogen and progestin to prevent pregnancy and provide effective contraceptive action for 1 month after insertion. The device is 2 inches in diameter and can be inserted anywhere in the vagina; however, the deeper it is placed, the less likely it is to be felt after insertion. Side effects of the NuvaRing are similar to those of other hormonal contraceptives, and it may increase the risks of heart attack, stroke, and blood clots. When the patient first starts using the ring, an additional method of birth control must be used for the first week. If the ring falls out, it should be rinsed with warm water and reinserted within 3 hours. If it is out for longer than 3 hours, contraception is not certain and the patient should use another birth control method for 1 week.
Depo-Provera is an injectable contraceptive that contains high doses of progestin. Each dose prevents pregnancy for up to 3 months, but women must be compliant in returning to the healthcare facility for follow-up and repeat doses every 9 to 13 weeks. The first injection should be administered within the first 5 days of the menstrual period for birth control coverage. This is a highly effective method of contraception and is ideal for women who either do not comply with a birth control regimen or do not want to take a pill every day. However, using Depo-Provera for 2 years or longer may increase the risk of bone loss and the eventual development of osteoporosis. Almost all patients using the injections experience some menstrual irregularities, but these usually subside after two doses. Women using this form of hormonal contraception are not at risk for the side effects of estrogen exposure, such as increased risk of blood clots and cardiovascular disease.
The Implanon implant is a single rod about the size of a match that is inserted under the skin of the upper arm. Implanon releases a low, steady dose of progestin, which suppresses ovulation, thickens cervical mucus to block the passage of sperm, and thins the endometrial wall to prevent implantation. It is currently the only contraceptive implant that is approved by the FDA and is designed to prevent pregnancy for up to 3 years after insertion. The Implanon implant has similar risks and contraindications as other hormonal types of contraception.
Intrauterine Devices
The intrauterine device (IUD) (Figure 41-4) is a T-shaped plastic frame with threads attached that is inserted by the physician into the uterus to prevent pregnancy. Two types of IUDs currently are available: the copper type (ParaGard) and the hormonal type (Mirena). Both products inhibit fertilization by blocking the sperm’s journey to the fallopian tubes, and if fertilization does occur, they prevent the embryo from implanting in the uterine wall. In addition, ParaGard releases copper, which acts to slow sperm in the cervix, and Mirena releases progestin, which reduces sperm mobility and prevents thickening of the endometrial wall during the menstrual cycle. Both types of IUDs are extremely effective at preventing pregnancy (over 99%); the copper type can remain in place as long as 10 years, whereas hormonal IUDs must be replaced every 5 years. The copper IUD may increase vaginal bleeding and menstrual pain, and the hormonal IUD results in both decreased menstrual flow and cramping. Shortly after placement of an IUD, the risk of infection is greater, so the physician may prescribe antibiotics before insertion to reduce this risk. To remove an IUD, the physician gently withdraws it by pulling on the IUD string. In rare instances, it must be removed surgically.
Permanent Methods
Both male and female patients can undergo surgical procedures that are considered permanent contraceptive methods. Vasectomies in the male were addressed in Chapter 40. For the female, a bilateral tubal ligation can be performed in which a portion of both fallopian tubes is excised or ligated. The cost and rate of complications are higher for tubal ligations than for vasectomies. In addition, tubal ligations must be done on an outpatient basis with general anesthesia, so the woman has that additional risk. Both procedures can be reversed, but not always successfully.
Gynecologic Diseases and Disorders
Menstrual Disorders and Conditions
Amenorrhea is the absence of menstruation for a minimum of 6 months; in oligomenorrhea, the woman has not experienced a period for 35 days to 6 months. The absence of menstruation outside pregnancy could be the result of a number of factors, including hormonal imbalance, thyroid disease, ovarian failure, or structural defects in the female sex organs. If a patient has established menstruation that stops, this usually is the result of a problem with the hypothalamus or the pituitary. Suppression of the hypothalamus can occur as the result of an eating disorder, stress, or extreme exercise that results in low body fat content.
Women who do not ovulate and therefore do not go through a monthly shedding of the endometrial wall of the uterus are at greater risk for cancer of the endometrium and the breast. Patients usually are started on oral contraceptives that artificially provide the hormones needed to create a monthly menstrual cycle. These women may experience fertility problems and require further testing and medical intervention to become pregnant.
Abnormal menstrual bleeding is a common cause of OB/GYN visits. Menorrhagia is excessive menstrual blood loss, such as a menses lasting longer than 7 days. The physician may ask the patient to count the number of tampons and pads used for several cycles to establish a method of determining an estimate of blood loss. Iron-deficiency anemia is a sign that a woman is losing excessive amounts of blood. Metrorrhagia is spotting or bleeding between menstrual cycles. The physician may prescribe oral contraceptives to atrophy the endometrium and lessen the bleeding. Surgical options for excessive menstrual flow include dilation and curettage (D&C) or, in extreme cases, hysterectomy.
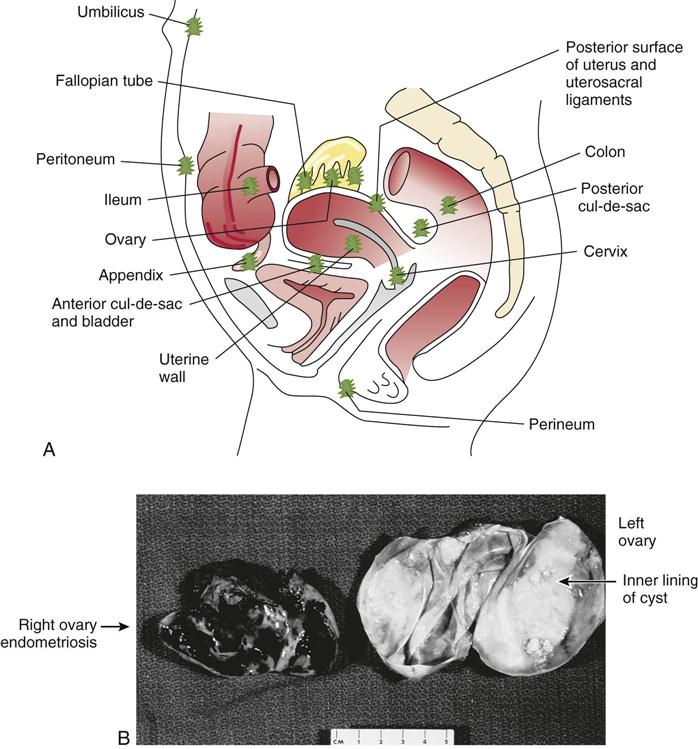
Endometriosis
Endometriosis is characterized by the presence of functional endometrial tissue outside the uterus. It commonly is found attached to the ovaries, urinary bladder, fallopian tubes, uterosacral ligaments, intestines, and peritoneum. Many hypotheses have been offered to explain this migration of endometrial tissue, but the most widely accepted is a retrograde flow during menstruation that causes menstrual fluid and stray endometrial cells to migrate out of the fallopian tubes and implant in the pelvic region. The use of tampons has been suggested as a possible cause. A familial tendency also has been noted; a woman with a first-degree relative (a mother or sister) who has the condition has a 10 times greater risk of developing the disorder.
The ectopic endometrial tissue responds to routine hormonal changes; it proliferates, degenerates, and bleeds just as does the endometrium of the uterus throughout the menstrual cycle. This causes inflammation at the site of the implantation that recurs with each cycle, ultimately leading to adhesions and obstruction of the affected tissue. The primary symptom of endometriosis is dysmenorrhea (painful menstruation). More than one third of affected patients also report dyspareunia (painful intercourse), and others complain of contact pain in the lower abdomen, pelvis, and back beginning 7 days before menses and lasting 3 days after onset. Other symptoms can include profuse menses, hematuria, rectal bleeding, nausea, vomiting, and abdominal cramps. Infertility is a serious problem for approximately 70% of women afflicted with endometriosis because of the buildup of scar tissue and adhesions in and around the fallopian tubes.
Conservative treatment through the use of hormones is recommended when the woman wants to have children. Treatment may consist of a laparoscopy to remove the ectopic endometrial tissue. Pharmaceutical treatment includes continuous use of oral contraceptives to prevent menstruation or Depo-Provera injections. Leuprolide acetate (Lupron) injections may be prescribed intramuscularly every month for 6 months; however, Lupron puts the patient into a state of artificial menopause and can cause menopausal symptoms, including hot flashes, vaginal dryness, and bone density loss. Another medication that causes induced menopause is oral danazol. Danazol lowers estrogen levels and increases androgen levels, which stops ovulation and shrinks endometrial growths; however, it can cause the development of male physical traits, an elevated cholesterol level, and liver disease. In severe cases, a total hysterectomy may be indicated. No cure for endometriosis is known, but pregnancy, breastfeeding, or natural menopause frequently causes remission (Figure 41-5).
Infections
Candidiasis
Candida albicans is the yeastlike fungus responsible for this candidiasis. Candida organisms are commonly part of the normal flora of the mouth, skin, intestinal tract, and vagina. Overgrowth of the organism can be caused by antibiotic use, high estrogen levels, oral contraceptive use, diabetes mellitus, and immunosuppressive disorders, including acquired immunodeficiency syndrome (AIDS). Candidiasis also can be spread through sexual contact. Symptoms include vulvovaginal itching; dry, bright red vaginal tissue; and an odorless, white, “cottage cheese” vaginal discharge. This infection can be treated with prescription antifungal medications, such as oral Diflucan or miconazole or terconazole vaginal suppositories, as well as with over-the-counter (OTC) creams or suppositories, such as Gyne-Lotrimin or Monistat. Women prescribed an antibiotic for a different infection may develop vaginal candidiasis as a side effect. To help prevent the development of a fungal infection during antibiotic therapy, the patient can eat active-culture yogurt and drink acidophilus milk.
Bacterial Vaginosis
Bacterial vaginosis (BV) occurs when the normal level of bacteria in the vagina is disrupted and secondary bacteria begin to grow and infect the tissue lining. Signs and symptoms include vaginal discharge, odor, pain, pruritus, or burning. Although BV is the most common vaginal infection in women of childbearing age in the United States, it does not usually cause complications. However, an infection of the vagina appears to make women more susceptible to STIs, including infection with the human immunodeficiency virus (HIV); it may lead to pelvic inflammatory disease (PID) if the infection spreads; and in pregnant women, it is associated with a premature or low-birth-weight infant. For these reasons, antibiotic therapy is especially important for pregnant women. The antibiotic of choice is either metronidazole (Flagyl) or clindamycin (Cleocin).
Cervicitis
Cervicitis is an inflammation of the cervix caused by an invading organism. The main sign is a thick, purulent, whitish discharge with an acrid odor. Dysuria may also be noted. Cervicitis can occur after vaginal delivery as a result of an infected cervical laceration, but most cases are caused by an STI. Treatment consists primarily of antibiotics, although cauterization may be indicated when cervical erosion exists.
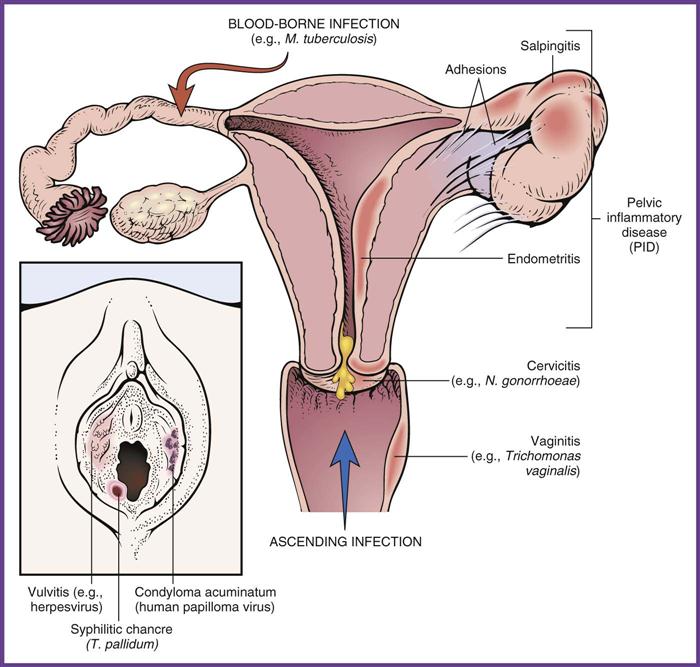
Pelvic Inflammatory Disease
PID is any acute or chronic infection of the reproductive system that ascends from the vagina (vaginitis), cervix (cervicitis), uterus (endometritis), fallopian tubes (salpingitis), and ovaries (oophoritis). These infections may cause the fallopian tubes to fill with pus, and chronic episodes can result in scarring of the fallopian tubes and the formation of adhesions. PID is caused by advanced, untreated vaginosis, gonorrhea, or chlamydial infection; or it can develop from infection after pelvic surgery, tubal examination, or abortion. PID is responsible for a large percentage of cases of infertility in women, primarily resulting from adhesions that form in the fallopian tubes, preventing the ovum from migrating through the tube. The patient may be asymptomatic or may complain of purulent vaginal discharge, fever, malaise, dysuria, lower abdominal pain, bleeding, nausea, and vomiting. Cultures of cervical discharge typically are done to determine the pathogenic organism. Treatment should include broad-spectrum antibiotic therapy, such as ofloxacin (Floxin) with Flagyl or ceftriaxone (Rocephin) with doxycycline (Vibramycin). If cultures are positive for an STI, treatment of the patient’s sexual partner is necessary to prevent reinfection.
Sexually Transmitted Infections
The list of infectious diseases spread by sexual contact continues to grow. These diseases are considered the most common contagious diseases in the United States. All STIs are transmitted from one person to another through body fluids such as blood, semen, or vaginal secretions during vaginal, anal, or oral sex (Figure 41-6). A summary of STIs was included in Chapter 40. This chapter focuses on the impact of STIs on women.
The human papilloma virus (HPV), which causes genital warts, is a matter of special concern in women. The infection may be asymptomatic up to 2 years after exposure; however, regardless of whether the virus causes symptomatic wart development, the infection can lead to serious complications in women. HPV infection typically is first diagnosed by abnormal Pap test results, because all 40 HPV types that are sexually transmitted can cause Pap test abnormalities. A positive Pap test result is followed up with an HPV DNA test to diagnose the specific strain of HPV that caused the infection. Although most women have a healthy immune system that can successfully clear the virus without the development of future health problems, approximately 15 high-risk HPV types are linked to the development of cervical carcinoma. Women diagnosed with one of these carcinogenic strains must have regular Pap testing, usually every 3 to 6 months, for early detection and treatment of precancerous and cancerous cells on the cervix.
The vaccine Gardasil is available to protect women from the four HPV types that cause 90% of genital warts, as well as cancers of the cervix, anus, vagina, vulva, and throat. Gardasil is routinely recommended for 11- and 12-year-old girls, as well as for those females between the ages of 13 and 26 who have not completed the vaccination series. The goal is to vaccinate young girls before they are sexually active. Even if a patient has been infected with one or more HPV types, she should still be vaccinated because this will give her protection from the HPV types not yet acquired. The Advisory Committee on Immunization Practice of the Centers for Disease Control and Prevention (CDC) recently made recommendations that males 9 through 26 years of age should also receive the Gardasil vaccine. The goal is to prevent the transmission of HPV to partners and to affect the rapid increase in the incidence of HPV-related throat and anal cancers. The vaccine is administered in three separate injections over a 6-month period, and total costs can range from $320 to $500.
Table 41-2 summarizes the effects of STIs on women. Individuals 35 to 44 years of age have the highest reported incidence of HIV infection and AIDS. The percentage of women and girls infected with HIV is declining, largely because of educational emphasis on the use of condoms; however, women account for 27% of HIV cases diagnosed each year. Because HIV can be transmitted through the placenta to the developing fetus, it is crucial that women be diagnosed either before pregnancy or as early in the pregnancy as possible. Treatment of HIV-positive pregnant women with a three-part ZDV regimen (zidovudine, AZT, or Retrovir) can cut the risk of transmission to below 2%. Even where resources are limited, a single dose of medicine given to mother and baby can reduce the risk of HIV infection in the infant by 50%. According to this treatment protocol, the pregnant woman should start taking ZDV at 14 to 34 weeks; it should be administered intravenously during labor and delivery; and it should be given to the infant every 6 hours for 6 weeks after birth. Because some AIDS drugs are very dangerous for developing infants, the medication regimen of a woman currently receiving treatment may be changed during pregnancy. Women who are HIV positive should never breastfeed, because the virus is present in breast milk.
TABLE 41-2
Sexually Transmitted Infections in Women
| INFECTION (CAUSATIVE ORGANISM) | SIGNS AND SYMPTOMS | TREATMENT |
| Chlamydia (Chlamydia trachomatis) | Dysuria; urinary frequency; abdominal pain; increased or decreased vaginal discharge. May cause endometritis, PID, and urethritis. Transmission to newborn can occur during vaginal delivery; causes neonatal eye infections and pneumonia. | Curable with antibiotic therapy; azithromycin (Zithromax), tetracycline, or Vibramycin |
| Genital herpes simplex virus (HSV-2) infection | Painful genital vesicles and ulcers; erythema and pruritus; tingling or shooting pain 1-2 days before outbreak; cycle through episodes. Viral shedding may occur during asymptomatic periods. Newborns can be infected by active lesions in vagina at birth. Brain damage, blindness, or death of the newborn may occur. Cesarean section if active lesions at time of birth. Increases risk for cervical cancer. | No cure, but antiviral therapy during episodes shortens duration of lesions; acyclovir (Zovirax), famciclovir (Famvir), or valacyclovir (Valtrex) |
| Genital warts (HPV) | Most prevalent STI; period of communicability is unknown; lesions seen more frequently in women; tend to recur; 25% of women with HPV develop invasive cervical cancer, should be followed with routine Pap smears (every 3-6 months). | Goal of treatment is to remove symptomatic warts; cryotherapy to lesions; podofilox solution or imiquimod cream to lesions |
| Gonorrhea (Neisseria gonorrhoeae)— bacteria | Dysuria; urinary frequency; abdominal pain; increased or decreased vaginal discharge. May cause endometritis, PID, and urethritis. | Curable with antibiotic therapy; cefixime (Suprax), azithromycin, doxycycline |
| Syphilis (Treponema pallidum)—spirochete bacteria | Six stages that can affect multiple body systems; 10- to 90-day incubation; initial sign is a painless lesion, or chancre, at the exposure site (vulva or vagina); serous discharge from chancre; lymphadenopathy. If not treated, advances to later stages. Can infect fetus via the placenta, resulting in congenital syphilis. | Penicillin G (Wycillin); if patient is allergic to penicillin, doxycycline or tetracycline |
| Trichomoniasis (Trichomonas vaginalis)—protozoa | May be asymptomatic; urinary frequency, urgency, and dysuria; frothy yellow-green vaginal discharge; pruritus. | Metronidazole (Flagyl); partner must be treated |
HPV, Human papillomavirus; PID, pelvic inflammatory disease; STI, sexually transmitted infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree