Assisting in Neurology and Mental Health
Learning Objectives
1. Define, spell, and pronounce the terms listed in the vocabulary.
2. Apply critical thinking skills in performing the patient assessment and patient care.
3. Summarize the anatomy and physiology of the nervous system.
4. Differentiate between the central and peripheral nervous systems.
5. Identify the typical symptoms associated with neurologic disorders.
6. Distinguish among common nervous system diseases and conditions.
7. Describe the pathology of cerebrovascular diseases.
8. Identify the various types of epilepsy.
9. Compare and contrast encephalitis and meningitis.
10. Explain the dynamics of brain and spinal cord injuries.
11. Summarize the neurologic diseases that affect mobility.
12. Differentiate among common mental health disorders.
13. Analyze the medical assistant’s role in the neurologic examination.
14. Explain the common diagnostic procedures for the nervous system.
15. Outline the steps needed to prepare a patient for an electroencephalogram (EEG).
16. Describe the steps for preparing a patient for and assisting with a lumbar puncture.
17. Discuss the implications of patient education in a neurologic and mental health practice.
Vocabulary
anomalies (uh-noh′-muh-lez) Deformities or deviations from a normal condition, resulting from faulty development of a fetus.
ataxia (uh-taks′-e-uh) Failure or irregularity of muscle actions and coordination.
aura A peculiar sensation that precedes the appearance of a more definite disturbance.
benign Not cancerous and not recurring.
blood-brain barrier An anatomic-physiologic structure made up of astrocyte glial cells that prevents or slows the transfer of chemicals into the neurons of the central nervous system (CNS).
coma An unconscious state from which the patient cannot be aroused.
compression The state of being pressed together.
contralateral (kon-trah-la′-tehr-uhl) Pertaining to the opposite side of the body.
cryptogenic (krip-tuh-je′-nik) Pertaining to a disease with an unknown cause.
ipsilateral (ips-uh-la′-tehr-uhl) Pertaining to the same side of the body.
malignant Cancerous.
occlusion Complete obstruction of an opening.
papilledema Swelling of the optic disc from increased intracranial pressure.
paresthesia (par-uhs-thee′-zee-uh) An abnormal sensation of burning, prickling, or stinging.
paroxysmal (par-ehk-siz′-muhl) Pertaining to a sudden, recurrent spasm of symptoms.
plaque An abnormal accumulation of a fatty substance.
radiopaque A substance that can easily be visualized on an x-ray film.
thrombus A blood clot.
transection Cross-section; a division made by cutting across.
turbid Refers to a cloudy solution.
Scenario
Mai Lee, CMA (AAMA), has been working in Dr. Kim Song’s neurology practice for 2 years. Dr. Song has always been pleased with Mai’s professional behavior toward all patients in the practice. She is conscientious about charting notes accurately for each of her patients. Dr. Song has just asked Mai to train a new medical assistant in the clinical procedures of the office. He is expanding his clinic hours and wants to have Mai more involved in assisting him with patients, particularly in patient education. She is excited to have additional responsibilities with Dr. Song’s patients, and she is quite happy about the raise in salary that goes along with her new position.
While studying this chapter, think about the following questions:
• What is the basic anatomy and physiology of the neurologic system?
• Mai should familiarize herself with what neurologic disorders?
• What are the diagnostic and treatment procedures for typical nervous system disorders?
• What is the medical assistant’s role in the neurologic examination?
The human brain weighs about 3 pounds, requires about the same amount of energy needed to light a 20-watt bulb, stores more than 100 trillion bits of information, and works better than any computer. The matter that makes up the brain is approximately 85% water and therefore has a soft texture. Early scientists believed that the brain’s function was to cool the blood. Today’s scientists have shown us that even though the brain receives 20% of the body’s blood supply, its function is much more complex than simply cooling blood.
Neurologists specialize in the diagnosis and treatment of medical disorders and conditions of the nervous system. A neurosurgeon provides surgical management and treatment for trauma and other conditions requiring surgery. A psychiatrist is a physician who treats behavioral disorders and neurologic conditions that affect behavior.
Anatomy and Physiology of the Nervous System
The nervous system works with the endocrine system to integrate stimuli both from within the body and from the outside environment to regulate body systems so that homeostasis can be maintained. The nervous system is divided into two major parts: the central nervous system (CNS), which is made up of the brain and spinal cord, and the peripheral nervous system (PNS), which includes all the nervous tissue and neurologic responses found outside the CNS.
The brain is the “president” or “chief executive officer” of the body. It constantly receives information from the periphery, including all the organs and systems inside the body and on its surface. This information (i.e., stimuli) is carried to the brain by the peripheral nerves along the afferent, or ascending, tract. The brain monitors and interprets the stimuli received from the afferent nerves and sends appropriate responses back along efferent pathways to the organs or to the body’s surface. These responses from the brain cause a specific reaction in the organ, in the glands, or in skeletal muscles. These reactions keep the body running smoothly and allow it to react instantly to both external and internal stimuli.
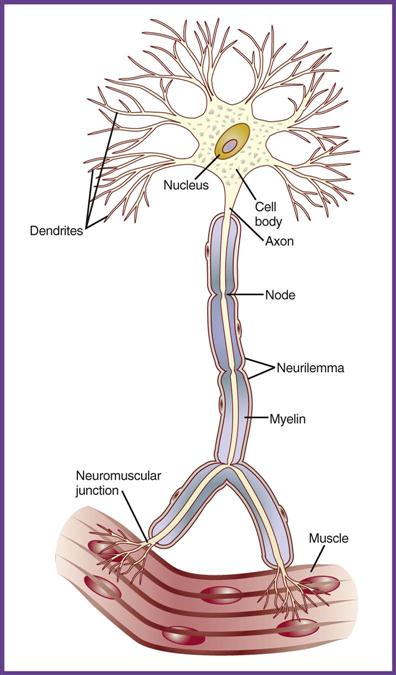
The functioning cell of the nervous system is the neuron (Figure 44-1). The brain contains billions of individual neurons. The nervous system begins very early in embryonic development, by week 3, as the neural tube, which eventually develops into the brain and spinal cord. Each neuron is made up of a main cell body that contains the nucleus and a relatively long extension of the cell, called the axon, which may be covered with a myelin sheath. Multiple filaments, called dendrites, extend from the neuron body. Dendrites receive the nervous impulse from a preceding neuron and carry it into the cell body. Impulses are carried away from the cell body through the axon to another neuron or to cells in another tissue. This transfer of stimuli begins as an electrical impulse that travels down an axon of one neuron and becomes a chemical impulse while moving across the synapse (the space between two neurons) to the dendrite of another neuron. The transfer of impulses from the end of one neuron to the dendrites of another is enhanced by chemical neurotransmitters, which bind to specific receptor sites on the dendrites of the next neuron. If the nerve impulse is traveling to a muscle or to any other organ or tissue instead of another neuron, the chemical neurotransmitters bind to special receptors in the target tissue. Messages move throughout the entire nervous system in this manner. Impulses in the neuron are electrical; the impulses become chemical as a specific neurotransmitter is released at each synapse, and they become electrical again as they are picked up by the subsequent dendrites of another neuron or by the target tissue.
Supportive cells of the nervous system are called glial or neuroglial cells. These specialized cells perform specific functions in the nervous system; for example, Schwann cells form the myelin sheath, and astrocytes help form the blood-brain barrier. However, the glial cells do not carry on any of the functions of the nervous system. The blood-brain barrier closely regulates what substances enter the brain tissue. Oxygen, water, and glucose molecules easily pass into the brain, whereas many chemicals and drugs are prevented from moving into brain tissue. Brain inflammation can increase the ability of many drugs to cross the blood-brain barrier.
Central Nervous System
The brain and spinal cord together make up the CNS. The brain is encased within the skull in the cranial cavity. The spinal cord is a bundle of nervous tissue that extends inferiorly from the brainstem at the base of the brain and exits the skull at the foramen magnum. It descends for about 17 inches inside the spinal canal, which courses through the vertebrae of the backbone.
Brain
The brain accounts for only about 2% of a person’s weight, but it consumes about 20% of the body’s oxygen. The brain is divided into three main areas: the cerebrum, the cerebellum, and the brainstem (Figure 44-2). The cerebrum, the largest and uppermost section of the brain, has multiple convolutions along its surface, called gyri, which are formed by the folding in of the cerebral cortex. The gyri are separated by shallow grooves, called sulci. The gyri greatly increase the surface area of the cerebrum, which maximizes the potential of the CNS neurons in each area. The cerebrum is divided into lobes, which are named after the region of the skull under which they are located. The cerebrum is separated by a longitudinal fissure into left and right hemispheres. The right hemisphere usually controls artistic functions, such as drawing, rhythm, and picture memory. The left hemisphere controls verbal functions, such as reading, writing, speaking, and mathematic calculations. The diencephalon, located deep in the center of the cerebrum near the superior portion of the brainstem, is made up of the thalamus and the hypothalamus. The thalamus acts as a relay station between sensory neurons and the cerebral cortex. The functions of the hypothalamus include controlling the autonomic nervous system, regulating endocrine processes, and managing body temperature, sleep, and appetite to maintain homeostasis. Within the cerebrum are four spaces, called ventricles, which contain cerebrospinal fluid (CSF). CSF nourishes, lubricates, and provides some cushioning protection for the brain and the spinal cord.
The cerebellum is just inferior to the occipital lobe of the cerebrum and controls balance, equilibrium, posture, and muscle coordination. The brainstem controls reflexes and serves as a sensory relay station for input coming into the brain from the body. The brainstem plays a vital role in vision, hearing, respiration, heart rate, blood pressure, waking, and sleeping.
Spinal Cord
The spinal cord extends from the inferior portion of the brainstem to approximately the second lumbar vertebra. Thirty-one pairs of spinal nerves extend from the spinal cord through openings in the vertebrae. Starting just below the first cervical vertebra in the neck, a nerve extends from the spinal cord on each side; therefore, a pair of spinal nerves originates at each level. Each of these pairs of nerves innervates a specific organ or area of the body. The spinal cord carries messages between the spinal nerves and the brain.
Meninges
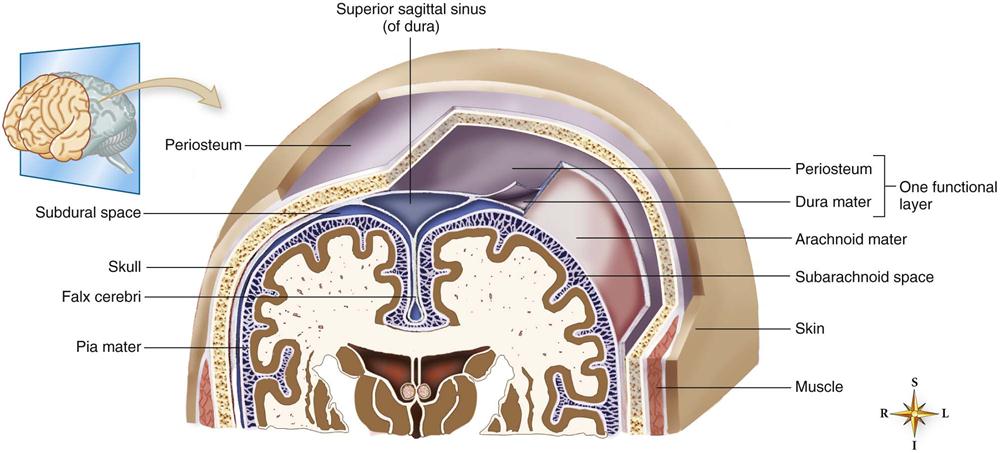
Because the brain and the spinal cord are critical to life, they are well protected. They both are encased in some of the thickest bones in the body; they also are surrounded by three membranes, called meninges; and they are cushioned by the CSF (Figure 44-3).
The outer layer of the meninges is called the dura mater (“hard mother”), because it is a tough membrane, similar to a very strong rubber band. The subdural space lies below the dura mater and contains small veins that have little support. Trauma to the head can cause bleeding of these tiny vessels, ultimately leading to the development of a subdural hematoma. Above the dura mater is the epidural space. The arterial supply to the meninges comes from blood vessels that line the inner aspect of the skull. If the skull is fractured, these arteries can be damaged, resulting in a collection of blood between the skull and the dura mater called an epidural hematoma.
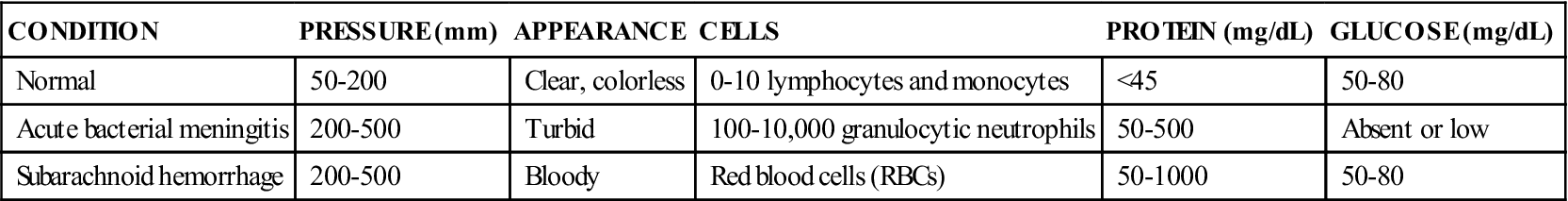
The middle meningeal layer is the arachnoid, which was given that name because of its fine spider web appearance. Beneath the arachnoid membrane in the subarachnoid space is the cerebrospinal fluid, a clear liquid that contains glucose, protein, and chloride produced by specialized cells in the ventricles (Table 44-1). CSF circulates continuously through the ventricles and around the brain and spinal cord, carrying nutrients and removing wastes.
TABLE 44-1
Typical Laboratory Values for Cerebrospinal Fluid
| CONDITION | PRESSURE (mm) | APPEARANCE | CELLS | PROTEIN (mg/dL) | GLUCOSE (mg/dL) |
| Normal | 50-200 | Clear, colorless | 0-10 lymphocytes and monocytes | <45 | 50-80 |
| Acute bacterial meningitis | 200-500 | Turbid | 100-10,000 granulocytic neutrophils | 50-500 | Absent or low |
| Subarachnoid hemorrhage | 200-500 | Bloody | Red blood cells (RBCs) | 50-1000 | 50-80 |
The innermost layer, which covers the brain and spinal cord, is the delicate pia mater (“tender mother”); it is highly vascular and the thinnest of the three layers. The pia mater provides support for the blood vessels of the brain.
Peripheral Nervous System
The PNS is made up of the nerves that exit the brain or spinal cord. The peripheral nerves exiting the brain directly through the cranium are called cranial nerves. The spinal nerves from the spinal cord enter and exit the spinal canal through spaces between the vertebrae. Cranial nerves originate from the underside of the brain and relay information to and from the sensory organs and muscles of the face and neck (Table 44-2).
TABLE 44-2
Cranial Nerves and Their Functions
| CRANIAL NERVE | NAME | FUNCTION |
| I | Olfactory | Smell |
| II | Optic | Vision |
| III | Oculomotor | Eye movement Pupil constriction and accommodation |
| IV | Trochlear | Eye movement |
| V | Trigeminal | Muscles of chewing General sensations from anterior half of head, including entire face and meninges |
| VI | Abducent | Eye movement |
| VII | Facial | Muscles of facial expression Tearing, salivation, and taste |
| VIII | Vestibulocochlear | Hearing and equilibrium |
| IX | Glossopharyngeal | Swallowing and taste |
| X | Vagus | Breathing, speech, sweating, regulating heartbeat, stimulating muscles of gastric region |
| XI | Spinal accessory | Shoulder and head movements |
| XII | Hypoglossal | Tongue movements |
Spinal nerves carry information to and from the brain through the spinal cord. Sensory fibers in these nerves carry stimuli from the skin and internal organs to the CNS. Motor fibers carry messages from the CNS to skeletal muscles, causing them to contract.
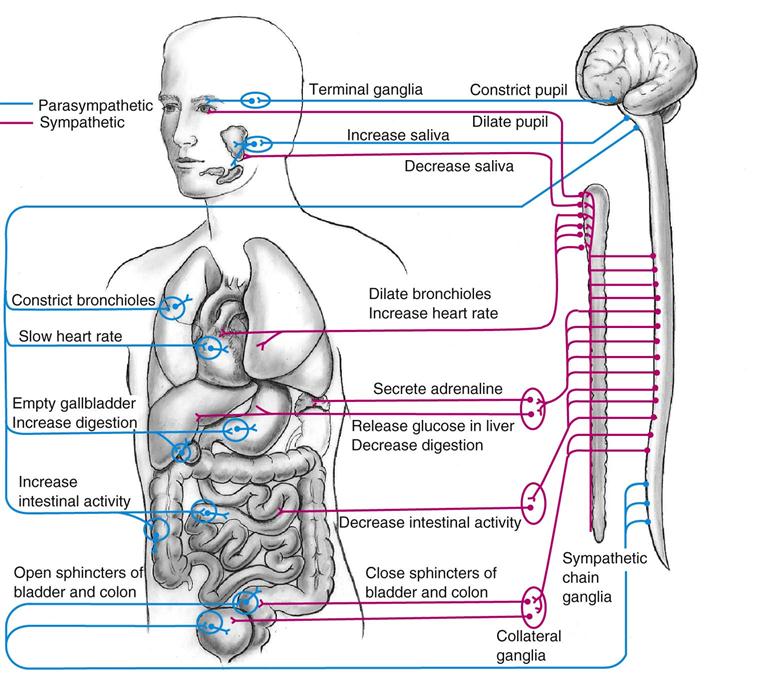
The autonomic nervous system (ANS) is part of the PNS. Autonomic nerves control homeostasis, or keep the body running smoothly, much like a thermostat controls the temperature in a room. The ANS (Figure 44-4) is an automatic system that regulates body functions such as breathing, heart rate, sweating, circulation, and digestion. It also controls the actions of muscles in blood vessel walls, organs, and glands. Just as a thermostat can control both heating and cooling in a room to maintain a comfortable temperature, the autonomic system is made up of two divisions, called the sympathetic system and the parasympathetic system. The sympathetic system promotes responses geared toward protecting the individual (“fight or flight”), generally causing a stimulating effect: it speeds up the heart, raises blood glucose levels and blood pressure, reduces peristalsis, and widens the bronchioles, allowing more oxygen to enter the body quickly. The parasympathetic system generally promotes rest or a reducing effect: it slows the heart rate, constricts the bronchioles, and increases digestive system function.
Diseases and Disorders of the Central Nervous System
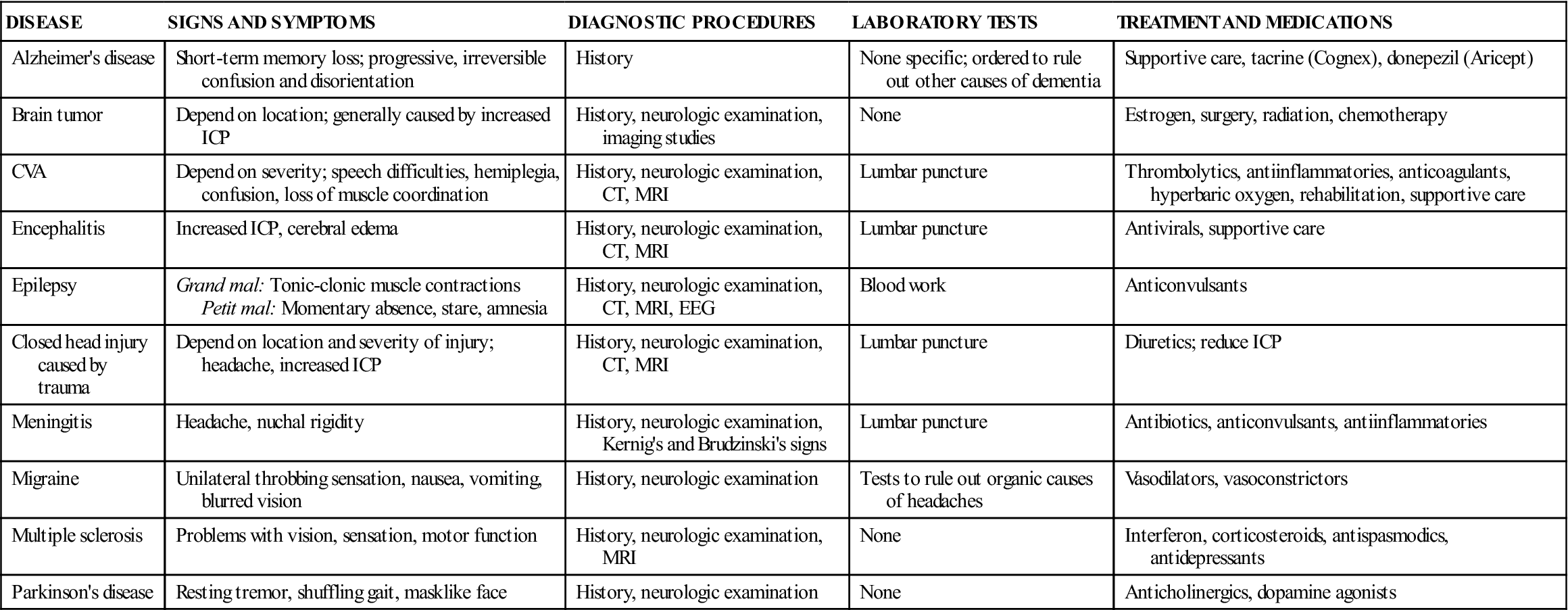
Because the CNS and PNS are so complex, diseases and conditions that affect them can produce a wide range of signs and symptoms. Causes include trauma, infection, congenital anomalies, degeneration, tumors, and vascular disorders (Table 44-3). The medical assistant needs to listen carefully when a patient describes his or her neurologic symptoms. Many different types of symptoms can indicate a serious condition of the nervous system.
TABLE 44-3
Common Diseases and Conditions of the Nervous System
| DISEASE | SIGNS AND SYMPTOMS | DIAGNOSTIC PROCEDURES | LABORATORY TESTS | TREATMENT AND MEDICATIONS |
| Alzheimer’s disease | Short-term memory loss; progressive, irreversible confusion and disorientation | History | None specific; ordered to rule out other causes of dementia | Supportive care, tacrine (Cognex), donepezil (Aricept) |
| Brain tumor | Depend on location; generally caused by increased ICP | History, neurologic examination, imaging studies | None | Estrogen, surgery, radiation, chemotherapy |
| CVA | Depend on severity; speech difficulties, hemiplegia, confusion, loss of muscle coordination | History, neurologic examination, CT, MRI | Lumbar puncture | Thrombolytics, antiinflammatories, anticoagulants, hyperbaric oxygen, rehabilitation, supportive care |
| Encephalitis | Increased ICP, cerebral edema | History, neurologic examination, CT, MRI | Lumbar puncture | Antivirals, supportive care |
| Epilepsy | Grand mal: Tonic-clonic muscle contractions Petit mal: Momentary absence, stare, amnesia | History, neurologic examination, CT, MRI, EEG | Blood work | Anticonvulsants |
| Closed head injury caused by trauma | Depend on location and severity of injury; headache, increased ICP | History, neurologic examination, CT, MRI | Lumbar puncture | Diuretics; reduce ICP |
| Meningitis | Headache, nuchal rigidity | History, neurologic examination, Kernig’s and Brudzinski’s signs | Lumbar puncture | Antibiotics, anticonvulsants, antiinflammatories |
| Migraine | Unilateral throbbing sensation, nausea, vomiting, blurred vision | History, neurologic examination | Tests to rule out organic causes of headaches | Vasodilators, vasoconstrictors |
| Multiple sclerosis | Problems with vision, sensation, motor function | History, neurologic examination, MRI | None | Interferon, corticosteroids, antispasmodics, antidepressants |
| Parkinson’s disease | Resting tremor, shuffling gait, masklike face | History, neurologic examination | None | Anticholinergics, dopamine agonists |
Cerebrovascular Disease
Cerebrovascular disease (CVD) is the third leading cause of death and the most frequent cause of crippling disease in the United States. Generally, CVD is related to arteriosclerosis or atherosclerosis of the cerebral arteries, but it also can be caused by untreated or uncontrolled hypertension, thrombi, or emboli. Arteriosclerosis causes progressive loss of elasticity of the arterial wall and is seen in elderly individuals with CVD. Atherosclerosis, the deposit of fatty plaque on the inside of the arterial wall, can involve any of the major arteries supplying the brain or any of their branches. Sudden narrowing, or occlusion, may occur when an artery becomes blocked by a thrombus or an embolus.
CVD usually is diagnosed through cerebral arterial angiography, in which a radiopaque dye is injected into the suspect vessel and a radiograph is immediately taken. Other confirming tests include magnetic resonance imaging (MRI), computed tomography (CT), and electroencephalography (EEG).
Transient Ischemic Attacks
Transient ischemic attacks (TIAs), also called ministrokes, occur when the blood supply to a particular part of the brain is inadequate for a limited time, usually seconds to minutes. TIAs occur when brain tissue becomes ischemic for a short time, causing the same symptoms as a stroke. Because the cause of the ischemia is limited, the symptoms dissipate quickly. Symptoms can include numbness or weakness in the face, arm, or leg or on one side of the body; confusion or difficulty talking or understanding speech; vision abnormalities, including diplopia; difficulty walking; and vertigo or loss of balance and coordination.
These episodes may occur in the days, weeks, or months before a stroke. Patients and their families should understand that any strokelike symptom should be taken seriously. Individuals experiencing TIAs should be seen within an hour of the onset of symptoms so that they can be evaluated carefully and treated to prevent a possible stroke. Individuals with atrial fibrillation (an irregular rapid firing of electrical activity in the atria of the heart) may be prescribed anticoagulants (e.g., heparin or warfarin [Coumadin]), or they may be put on daily low-dose aspirin or clopidogrel (Plavix), because these individuals are at increased risk of emboli formation. TIAs are important warning signs that the patient is at serious risk of having a debilitating stroke. When TIAs occur, it is time for preventive treatment and patient education, including altering and/or treating such factors as hypertension, smoking, heart disease, diabetes, carotid artery disease (carotid artery occlusion with atherosclerotic plaques), and alcohol abuse.
Cerebrovascular Accident
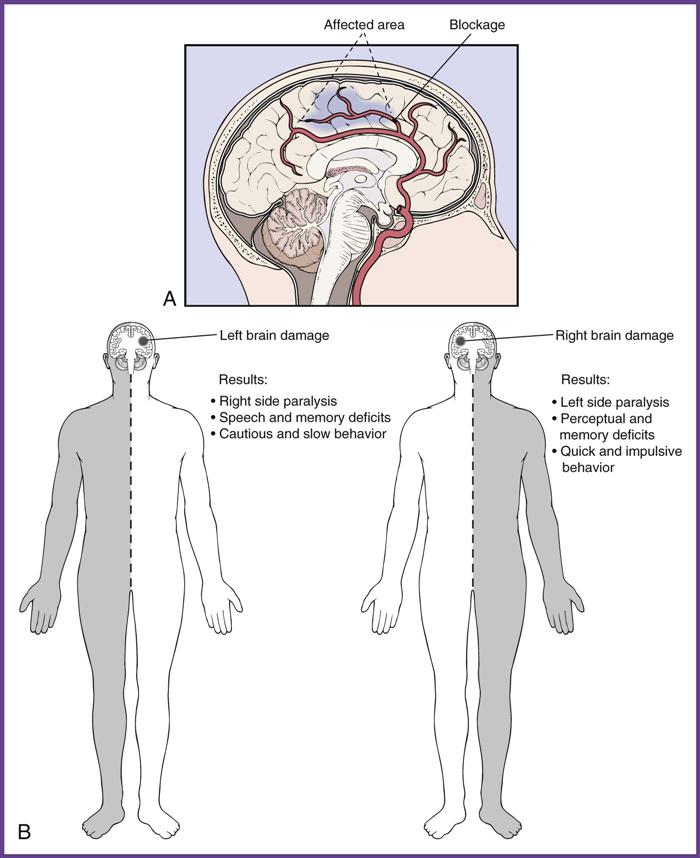
A cerebrovascular accident (CVA) is the most important clinical manifestation of CVD. A CVA, commonly referred to as a stroke, occurs when a vessel in the brain either ruptures or occludes and the tissue on the other side of the damaged vessel becomes oxygen deprived. Cerebral artery ruptures are caused by uncontrolled hypertension or hemorrhaging of a weakened section of an artery in the brain. As a result of the rupture, the surrounding brain tissue fills with blood, damaging and possibly destroying the affected tissue. An occlusion occurs when an embolus or thrombus becomes wedged in an artery and obstructs the flow of blood to an area of the brain (Figure 44-5).
The patient’s subsequent symptoms depend on the location of the arterial occlusion or rupture. Some of the more common symptoms include slurred speech; unexplained confusion; sudden, severe headache; difficulty swallowing; vertigo; diplopia; loss of consciousness; personality change; loss of bowel or bladder control; and paralysis on one side of the body.
Treatment of a stroke requires immediate emergency transport to the hospital. The initial emphasis is on minimizing the long-term disabilities often seen with strokes by providing immediate treatment to salvage as much brain tissue as possible. Thrombolytic drugs to dissolve the clot and anticoagulants may be given if the cause of the stroke was a thrombus or an embolus. However, thrombolytic medication can effectively treat resulting ischemia only if it is given within the first 3 to 6 hours after the ischemia began. If cerebral edema is present, the patient is treated with corticosteroids and diuretics to reverse the swelling. Hyperbaric oxygen also can be used to increase oxygenation of the brain. An important part of the subsequent recovery is extensive treatment in a stroke rehabilitation program that includes physical, occupational, and speech therapies.
Migraine Headache
More than 28 million Americans suffer from migraine headaches, and the condition affects three times more women than men. Migraine headaches are paroxysmal attacks of headaches that can be completely incapacitating and frequently are associated with other symptoms, such as nausea, vomiting, visual disturbances, and throbbing pain on one side of the head. The manifestations of migraine headaches differ from one individual to another. The patient may experience a sensory warning sign (an aura) before the onset of the headache. An aura often consists of some form of visual disturbance, such as dark lines or spots within the visual field or a flash of light.
Medical science has not yet discovered the underlying cause of migraines. However, some researchers believe they may be caused by a combination of a problem with the trigeminal nerve and an imbalance of chemicals in the brain, especially the neurotransmitter serotonin; this causes cerebral blood vessels to become dilated and inflamed, resulting in the acute onset of a terrible headache. Individuals who suffer from migraine headaches report a number of different triggers, including changes in estrogen levels; certain foods, such as alcohol, chocolate, aspartame, caffeine, and monosodium glutamate (MSG); elevated stress levels; bright lights, sun glare, and certain smells; altered sleep patterns; and changes in the weather, especially with changing altitude levels and barometric pressures. The diagnosis usually is established from a complete medical history. EEG, a CT scan, or an MRI study can be performed as part of the diagnostic process to rule out other causes of the headaches.
Drugs used to treat migraines include nonsteroidal antiinflammatory drugs (NSAIDs) or triptans, such as sumatriptan (Imitrex), rizatriptan (Maxalt), or zolmitriptan (Zomig), which mimic the effects of serotonin, causing vascular constriction (these drugs must be taken at the onset of the headache to be effective). Other medications recommended for the prevention of migraines include beta blockers and antidepressants. Antiseizure medications, such as topiramate (Topamax) and gabapentin (Neurontin), may be effective in reducing the frequency and severity of the headaches. Other treatments include biofeedback techniques and elimination diets to avoid migraine triggers.
Dementia and Alzheimer’s Disease
The term dementia describes a group of symptoms caused by altered brain function. Dementia symptoms may include short-term memory loss; disorientation about person, time, and place; neglect of personal hygiene, nutrition, and safety; personality changes; and inability to follow simple directions. Dementia can be caused by multiple conditions. Some can be reversed, such as nutrition disorders or disorientation caused by a minor head injury. Others are irreversible, such as multi-infarct (vascular) dementia and Alzheimer’s disease.
Multi-infarct dementia is caused by a series of small strokes that interfere with the brain’s blood supply, resulting in multiple areas of tissue necrosis. The location of the infarcts determines the degree of disability and the dementia symptoms that might occur. Symptoms of an acute onset of dementia typically are caused by this type of dementia. People with multi-infarct dementia are likely to show signs of improvement or remain stable for long periods and then quickly develop new symptoms if more strokes occur. Untreated or uncontrolled hypertension usually is the cause of this type of dementia.
Alzheimer’s disease is the most common form of dementia among older people today. It is a devastating, chronic, progressive, and degenerative disease that begins in the parts of the brain that control thought, memory, and language. The patient exhibits slow, increasing loss of recent memory; loss of recognition of people, places, and events; confusion and disorientation; and physical deterioration that leads to death. The cause remains unknown, and there is no known cure. Treatment is supportive care only. (Alzheimer’s disease is addressed in more detail in Chapter 48.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree