Chapter 27 1. Describe the clinical manifestations and nursing and collaborative management of problems of the nose. 2. Discuss the clinical manifestations and nursing and collaborative management of problems of the paranasal sinuses. 3. Describe the clinical manifestations and nursing and collaborative management of problems of the pharynx and larynx. 4. Discuss the nursing management of the patient who requires a tracheostomy. 5. Identify the steps involved in performing tracheostomy care and suctioning an airway. 6. Describe the risk factors and warning symptoms associated with head and neck cancer. 7. Discuss the nursing management of the patient with a laryngectomy. 8. Explain the methods used in voice restoration for the patient with temporary or permanent loss of speech. Deviated septum is a deflection of the normally straight nasal septum. Although up to 80% of the adult population may have septums that are slightly off center, the diagnosis of deviated septum is generally reserved for those that are severely shifted.1 Trauma to the nose, either at birth or later in life, is the most common cause of deviated septum.2 Deviation from midline can interfere with airflow and sinus drainage through the narrowed passageway. Symptoms vary depending on the degree of deviation. Minor septal deviations may be asymptomatic. Common manifestations of septal deviation include obstruction to nasal breathing, nasal congestion, frequent sinus infections and nosebleeds (epistaxis), and facial pain. Medical management of deviated septum is focused on symptom control of nasal inflammation and congestion (see Table 27-2). For recurrent or severe symptoms, a nasal septoplasty is performed to reconstruct and properly align the deviated septum. Nasal fractures can be classified as simple or complex. Simple fractures may be unilateral or bilateral and typically produce little or no displacement.3 Powerful frontal blows can cause complex fractures, which may also involve subsequent damage to adjacent facial structures such as the teeth, eyes, or other facial bones. Orbital fractures may be seen with midfacial trauma. On inspection, assess the patient’s ability to breathe through each side of the nose and note the presence of edema, bleeding, or hematoma. Ecchymosis may be under one or both eyes. Ecchymosis involving both eyes is often termed raccoon eyes and may suggest an orbital or basilar skull fracture (see Chapter 57). Inspect the nose internally for evidence of septal deviation, hemorrhage, or clear drainage. Clear, pink-tinged, or persistent drainage after control of epistaxis suggests a CSF leak. Perform a quick test at the bedside or send a specimen to the laboratory to determine if glucose is present; the presence of glucose indicates that the fluid is CSF. Rhinoplasty is performed as an outpatient procedure using regional or general anesthesia. Sometimes nasal tissue is added or removed, and the nose may be lengthened or shortened. Plastic implants are sometimes used to reshape the nose. Incisions are typically inside the nose and are thus hidden. Sonic rhinoplasty incorporates the use of an ultrasonic device to gently aspirate bone, enabling a refined cosmetic result.4 Examples of nasal surgery include rhinoplasty, septoplasty, and nasal fracture reductions. Before surgery, instruct the patient not to take aspirin-containing drugs or NSAIDs for 2 weeks to reduce the risk of bleeding. Encourage preoperative smoking cessation to promote postoperative wound healing. Nursing interventions during the immediate postoperative period include maintenance of the airway; assessment of respiratory status; pain management; and observation of the surgical site for bleeding, infection, and edema. Teaching is important because the patient must be able to detect early and late complications at home. The patient typically experiences temporary edema and ecchymosis. Cold compresses and elevation of the head can help minimize swelling and discomfort. Teach activity restrictions aimed at preventing bleeding and injury (no nose blowing, swimming, heavy lifting, strenuous exercise).5 Subtle swelling may be slow to resolve, delaying the achievement of a full cosmetic result for up to a year. Epistaxis (nosebleed) occurs in a bimodal distribution, with children 2 to 10 years of age and adults over age 50 most affected. Epistaxis can be caused by low humidity, allergies, upper respiratory tract infections, sinusitis, trauma, foreign bodies, hypertension, chemical irritants such as street drugs, overuse of decongestant nasal sprays, facial or nasal surgery, anatomic malformation, and tumors.6 Any condition that prolongs bleeding time or alters platelet counts will predispose the patient to epistaxis. Bleeding time may also be prolonged if the patient takes aspirin, NSAIDs, warfarin, or other anticoagulant drugs. Medical management involves identifying the bleeding site and applying a vasoconstrictive agent, cauterization, or anterior packing. Pledgets (nasal tampon) impregnated with anesthetic solution (lidocaine) and/or vasoconstrictive agents such as cocaine or epinephrine are placed into the nasal cavity and left in place for 10 to 15 minutes. Silver nitrate may be used to chemically cauterize an identified bleeding point after epistaxis is controlled. Thermal cauterization is reserved for more severe bleeding and requires the use of local or general anesthesia.7 If bleeding does not stop, packing may be used. Packing with compressed sponges (e.g., Merocel) or epistaxis balloons (e.g., Rapid Rhino) is preferred over the use of traditional Vaseline ribbon gauze because of the ease of placement. Packing is inserted into the nares and advanced along the floor of the nasal cavity. The sponge expands with moisture to fill the nasal cavity and tamponade bleeding. The balloon is inflated with air to achieve the same pressure effect (Fig. 27-1). Alternatively, absorbable materials such as oxidized cellulose (surgical), gelatin foam (Gelfoam), or a gelatin-thrombin combination (Floseal) may be used as packing for anterior bleeds. In addition to providing pressure to stop bleeding, these materials increase clot formation and protect the nasal mucosa from further trauma.7 A nasal sling (a folded 2 × 2-in gauze pad) may be taped under the nares to absorb drainage. Allergic rhinitis is the reaction of the nasal mucosa to a specific allergen. Allergic rhinitis can be classified according to the causative allergen (seasonal or perennial) or the frequency of symptoms (episodic, intermittent, or persistent).8 Episodic refers to symptoms related to sporadic exposure to allergens that are not typically encountered in the patient’s normal environment, such as exposure to animal dander when visiting another person’s home. Intermittent means that the symptoms are present less than 4 days a week or less than 4 weeks per year. Persistent means that the symptoms are present more than 4 days a week and for more than 4 weeks per year. Sensitization to an allergen occurs with initial allergen exposure, which results in the production of antigen-specific immunoglobulin E (IgE) (see Fig. 14-6). After exposure, mast cells and basophils release histamine, cytokines, prostaglandins, and leukotrienes, which cause the early symptoms of sneezing, itching, rhinorrhea, and congestion. Four to 8 hours after exposure, inflammatory cells infiltrate the nasal tissues, causing and maintaining the inflammatory response. Because symptoms of rhinitis resemble those of the common cold, the patient may believe the condition is a continuous or repeated cold. The most important step in managing allergic rhinitis is identifying and avoiding triggers of allergic reactions (Table 27-1). Instruct the patient to keep a diary of times when the allergic reaction occurs and the activities that precipitate the reaction. Patients are often more aware of intermittent exposure to an allergen such as pets than they are of a more persistent exposure to allergens such as dust mites, cockroaches, or mold. Identifying such triggers is the first step toward avoiding them. TABLE 27-1 PATIENT & CAREGIVER TEACHING GUIDE • Focus on the bedroom. Remove carpeting. Limit furniture. • Put the pillows, mattress, and springs in airtight vinyl bags or containers. • Limit clothing in the bedroom to items used frequently. Place clothing in airtight, zipper-sealed vinyl clothes bags. • Install an air filter. Close the air conditioning vent into the room. Use blinds rather than draperies. • The three Ds that promote growth of mold spores are darkness, dampness, and drafts. • Ventilate closed rooms and open doors. Consider adding windows to dark rooms. Consider keeping a small light on in closets. • Basement light with a timer that provides light several hours a day may decrease mold growth. • Avoid places where humidity is high (e.g., basements, clothes hampers, greenhouses, barns). Dehumidifiers are rarely helpful. The goal of medications is to reduce inflammation associated with allergic rhinitis, reduce nasal symptoms, minimize associated complications, and maximize quality of life. Appropriate oral medication options include H1-antihistamines, corticosteroids, decongestants, and leukotriene receptor antagonists (LTRAs). Intranasal medications include antihistamines, anticholinergics, corticosteroids, cromolyn, and decongestants9 (Table 27-2). TABLE 27-2 DRUG THERAPY • Warn patient that operating machinery and driving may be dangerous because of sedative effect. • Teach patient to report palpitations, change in heart rate, change in bowel or bladder habits. • Instruct patient not to use alcohol with antihistamines because of additive depressant effect. • Rapid onset of action, no drug tolerance with prolonged use.
Nursing Management
Upper Respiratory Problems
Problems of Nose and Paranasal Sinuses
Deviated Septum
Nasal Fracture
Rhinoplasty
Nursing Management Nasal Surgery
Epistaxis
Nursing and Collaborative Management Epistaxis
Allergic Rhinitis
Nursing and Collaborative Management Allergic Rhinitis
Avoiding Allergens in Allergic Rhinitis
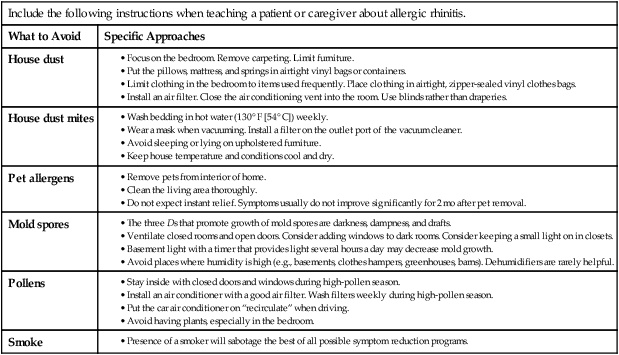
Include the following instructions when teaching a patient or caregiver about allergic rhinitis.
What to Avoid
Specific Approaches
House dust
House dust mites
Pet allergens
Mold spores
Pollens
Smoke
Rhinitis and Sinusitis
Drug
Mechanism of Action
Side Effects
Nursing Actions
Corticosteroids
Nasal Spray
beclomethasone (Beconase)
budesonide (Rhinocort)
ciclesonide (Omnaris)
flunisolide (Nasalide)
fluticasone (Flonase)
fluticasone furoate (Veramyst)
mometasone (Nasonex)
triamcinolone (Nasacort)
Inhibits inflammatory response of allergic rhinitis. At recommended dose, systemic side effects are unlikely because of low systemic absorption. Systemic effects may occur with higher than recommended doses.
Mild transient nasal burning and stinging, mucosal drying.
In rare instances, localized fungal infection with Candida albicans.
Mast Cell Stabilizer
Nasal Spray
cromolyn spray (NasalCrom)
Suppresses release of histamine and other inflammatory mediators from mast cells.
Minimal side effects. Occasional burning or nasal irritation.
Leukotriene Receptor Antagonists (LTRAs) and Inhibitors
Antagonists
zafirlukast (Accolate)
montelukast (Singulair)
Inhibitors
zileuton (Zyflo)
Suppress leukotriene activity, thereby inhibiting airway edema, bronchoconstriction, mucus production, and inflammation (see Fig. 12-2).
Generally well tolerated.
May cause headaches, dizziness, rash, altered liver function tests, GI disturbances.
Zafirlukast and zileuton: Monitor PT levels and theophylline levels if patient is taking warfarin or theophylline.
Anticholinergic
Nasal Spray
ipratropium bromide (Atrovent)
Blocks nasal cholinergic receptors, reducing nasal secretions in the common cold and nonallergic rhinitis.
Nasal dryness and irritation may occur. Does not cause systemic side effects.
Antihistamines
First-Generation Agents (Oral)
azatadine (Optimine)
brompheniramine (Dimetane)
chlorpheniramine (Chlor-Trimeton)
clemastine (Tavist)
dexchlorpheniramine (Polaramine)
diphenhydramine (Benadryl)
levocetirizine (Xyzal)
Bind with H1 receptors on target cells, blocking histamine binding. Relieve acute symptoms of allergic response (itching, sneezing, rhinorrhea).
Cross blood-brain barrier, frequently causing sedation and somnolence.
Can also cause paradoxical stimulation (restlessness, nervousness, insomnia).
Anticholinergic side effects (e.g., palpitations, dry mouth, constipation, urinary hesitancy).
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Nursing Management: Upper Respiratory Problems
Get Clinical Tree app for offline access