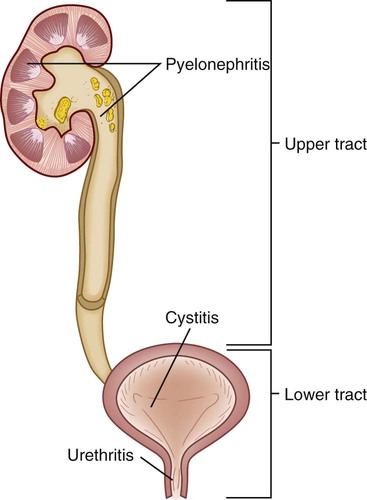
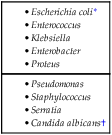
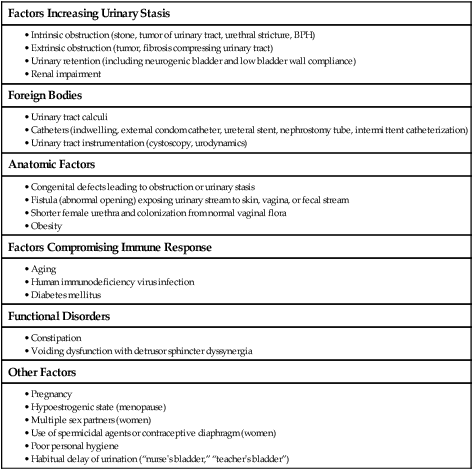
Chapter 46 1. Differentiate the pathophysiology, clinical manifestations, collaborative care, and drug therapy of cystitis, urethritis, and pyelonephritis. 2. Explain the nursing management of urinary tract infections. 3. Describe the immunologic mechanisms involved in glomerulonephritis. 4. Differentiate the clinical manifestations and nursing and collaborative management of acute poststreptococcal glomerulonephritis, Goodpasture syndrome, and chronic glomerulonephritis. 5. Describe the common causes, clinical manifestations, collaborative care, and nursing management of nephrotic syndrome. 6. Compare and contrast the etiology, clinical manifestations, collaborative care, and nursing management of various types of urinary calculi. 7. Differentiate the common causes and management of renal trauma, renal vascular problems, and hereditary kidney diseases. 8. Describe the clinical manifestations and nursing and collaborative management of kidney cancer and bladder cancer. 9. Describe the common causes and management of urinary incontinence and urinary retention. 10. Differentiate among urethral, ureteral, suprapubic, and nephrostomy catheters with regard to indications for use and nursing responsibilities. 11. Explain the nursing management of the patient undergoing nephrectomy or urinary diversion surgery. Renal and urologic disorders encompass a wide spectrum of problems. The diverse causes of these disorders may involve infectious, immunologic, obstructive, metabolic, collagen-vascular, traumatic, congenital, neoplastic, and neurologic mechanisms. This chapter discusses specific disorders of the upper urinary tract (kidneys and ureter) and lower urinary tract (bladder and urethra). Acute kidney injury and chronic kidney disease are discussed in Chapter 47. eTABLE 46-1 Source: American Cancer Society. eTABLE 46-2 Source: American Cancer Society. Urinary tract infections (UTIs) are the most common bacterial infection in women. During their lifetime, at least 20% of women develop at least one UTI.1 More than 100,000 people are hospitalized annually for UTIs. More than 15% of patients who develop gram-negative bacteremia die, and one third of these cases are caused by bacterial infections originating in the urinary tract.2 Escherichia coli is the most common pathogen causing a UTI (Table 46-1) and is primarily seen in women. Bacterial counts of 105 colony-forming units per milliliter (CFU/mL) or higher typically indicate a clinically significant UTI. However, counts as low as 102 to 103 CFU/mL in a person with signs and symptoms are indicative of UTI. TABLE 46-1 CAUSES OF URINARY TRACT INFECTIONS *Causative microorganism for urinary tract infection (UTI) in 80% of cases without urinary tract structural abnormalities or calculi. †Typically identified as the causative microorganism for UTI associated with the use of broad-spectrum antibiotic therapy or in patients with an indwelling catheter. A UTI can be broadly classified as an upper or lower UTI according to its location within the urinary system (Fig. 46-1). Infection of the upper urinary tract (involving the renal parenchyma, pelvis, and ureters) typically causes fever, chills, and flank pain, whereas a UTI confined to the lower urinary tract does not usually have systemic manifestations. Specific terms are used to further delineate the location of a UTI. For example, pyelonephritis implies inflammation (usually caused by infection) of the renal parenchyma and collecting system, cystitis indicates inflammation of the bladder, and urethritis means inflammation of the urethra. Urosepsis is a UTI that has spread systemically and is a life-threatening condition requiring emergency treatment. The urinary tract above the urethra is normally sterile. Several mechanical and physiologic defense mechanisms assist in maintaining sterility and preventing UTIs. These defenses include normal voiding with complete emptying of the bladder, ureterovesical junction competence, and ureteral peristaltic activity that propels urine toward the bladder. Antibacterial characteristics of urine are maintained by an acidic pH (less than 6.0), high urea concentration, and abundant glycoproteins that interfere with the growth of bacteria. An alteration in any of these defense mechanisms increases the risk for a UTI (Table 46-2). TABLE 46-2 RISK FACTORS FOR URINARY TRACT INFECTIONS A common factor contributing to ascending infection is urologic instrumentation (e.g., catheterization, cystoscopic examinations).3 Instrumentation allows bacteria that are normally present at the opening of the urethra to enter into the urethra or bladder. Sexual intercourse promotes “milking” of bacteria from the vagina and perineum and may cause minor urethral trauma that predisposes women to UTIs. An important source of UTIs is health care–associated infections (HAIs), previously called nosocomial infections, which account for 31% of all HAIs.2,4 The cause of HAIs is often E. coli and, less frequently, Pseudomonas organisms. Catheter-acquired urinary tract infections (CAUTIs) are the most common HAIs and are caused by development of bacterial biofilms that are found on the catheter’s inner surface. Most often these infections are underrecognized and undertreated, leading to complications such as renal abscesses, epididymitis, periurethral gland infections, and bacteremia. Lower urinary tract symptoms (LUTS) are experienced in patients who have UTIs of the upper urinary tract, as well as those confined to the lower tract. Symptoms are related to either bladder storage or bladder emptying. These symptoms are presented in Table 46-3. TABLE 46-3 LOWER URINARY TRACT SYMPTOMS (LUTS) • Difficulty starting urine stream • Delay between initiation of urination (because of urethral sphincter relaxation) and beginning of flow of urine
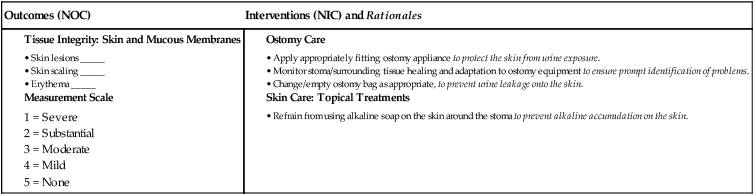
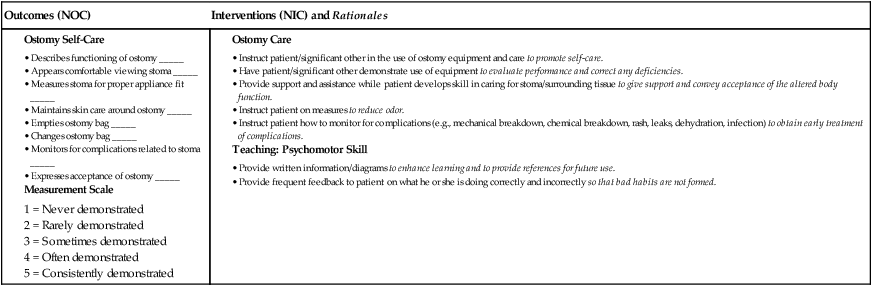
Nursing Management
Renal and Urologic Problems
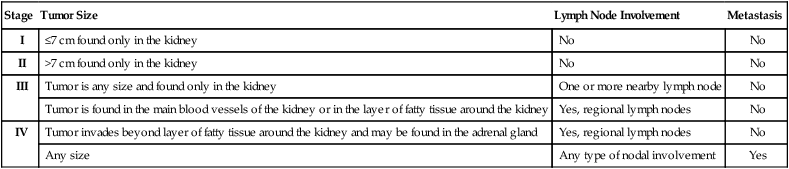
Stage
Tumor Size
Lymph Node Involvement
Metastasis
I
≤7 cm found only in the kidney
No
No
II
>7 cm found only in the kidney
No
No
III
Tumor is any size and found only in the kidney
One or more nearby lymph node
No
Tumor is found in the main blood vessels of the kidney or in the layer of fatty tissue around the kidney
Yes, regional lymph nodes
No
IV
Tumor invades beyond layer of fatty tissue around the kidney and may be found in the adrenal gland
Yes, regional lymph nodes
No
Any size
Any type of nodal involvement
Yes
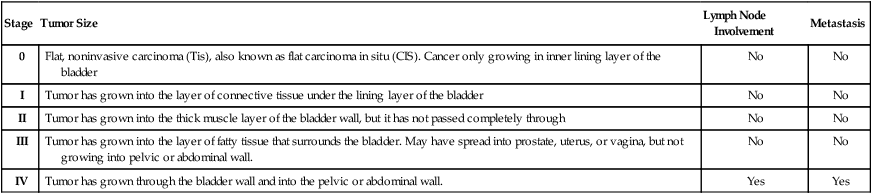
Stage
Tumor Size
Lymph Node Involvement
Metastasis
0
Flat, noninvasive carcinoma (Tis), also known as flat carcinoma in situ (CIS). Cancer only growing in inner lining layer of the bladder
No
No
I
Tumor has grown into the layer of connective tissue under the lining layer of the bladder
No
No
II
Tumor has grown into the thick muscle layer of the bladder wall, but it has not passed completely through
No
No
III
Tumor has grown into the layer of fatty tissue that surrounds the bladder. May have spread into prostate, uterus, or vagina, but not growing into pelvic or abdominal wall.
No
No
IV
Tumor has grown through the bladder wall and into the pelvic or abdominal wall.
Yes
Yes
Infectious and Inflammatory Disorders of Urinary System
Urinary Tract Infection
Classification of Urinary Tract Infection
Etiology and Pathophysiology
Factors Increasing Urinary Stasis
Foreign Bodies
Anatomic Factors
Factors Compromising Immune Response
Functional Disorders
Other Factors
Clinical Manifestations
Symptoms
Description
Emptying Symptoms
Hesitancy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Nursing Management: Renal and Urologic Problems
Get Clinical Tree app for offline access